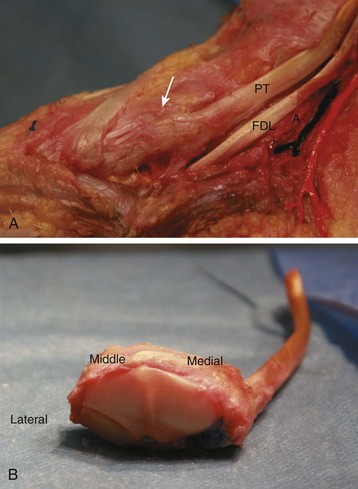
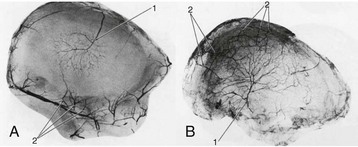
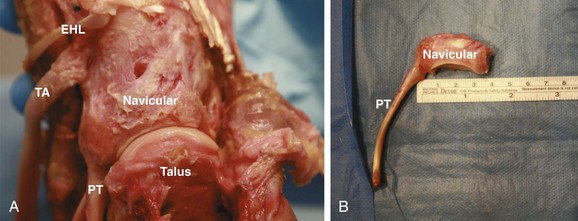
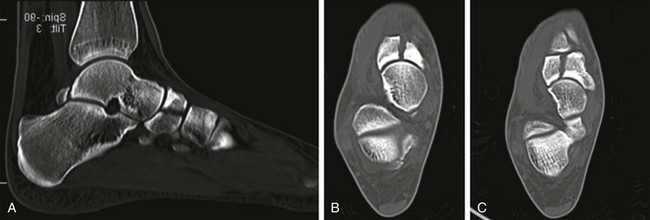
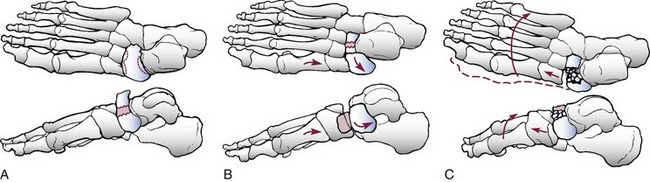
Chapter 40 The tarsal navicular is the keystone to the longitudinal arch of the foot. It lies in the uppermost portion of the medial longitudinal arch of the foot between the head of the talus and the three cuneiforms (Fig. 40-1A and B). Its shape as a six-sided disk with a concave proximal talus-sided portion and convex distal cuneiform portion makes it uniquely shaped for its role as a connection from the hindfoot to the midfoot. This shape also allows the pronation and supination required for the locking and unlocking of the transverse tarsal joint during normal gait biomechanics. The navicular serves as the insertion for the posterior tibial tendon on the medial-sided tuberosity. This allows inversion of the foot and supination of the navicular. The tarsal navicular also has numerous ligamentous attachments (see Fig. 40-1A). The strongest of these ligaments is the confluence of the dorsal talonavicular ligament and the anterior division of the deltoid ligament on the medial side, which joins to form the tibionavicular ligament, as described by Eichenholtz and Levine.35 The spring ligament originates on the sustentaculum tali of the calcaneus, travels under the talar head, and then inserts on the navicular tuberosity. The cuneonavicular ligaments attach plantarly and dorsally, whereas the interosseous cuboideonavicular ligaments attach laterally. Another key anatomic relationship is between the navicular, head of the talus, and anterior process of the calcaneus. These three structures come together to form the acetabulum pedis. This socket relationship, which was described by Sarrafian,7 allows the foot to swivel around the head of the talus at heel strike while the subtalar joint is everted. As the foot moves through midstance, the transverse tarsal joints are parallel, allowing flexibility and shock absorption. As one moves from midstance to toe-off, the subtalar joint is supinated, and the talonavicular and calcenocuboid joints are nonparallel and locked. This provides a stable foot for push-off. The function of the talonavicular joint is critical for subtalar motion during normal gait. Astion et al5 reported that the isolated talonavicular fusion can lead to up to 90% loss of supination. The blood supply, as illustrated in Figure 40-2, is crucial to understanding the pathoanatomy of injuries to the navicular and its healing potential. The navicular is covered nearly completely with cartilage, and thus the blood vessels can enter over a limited number of surfaces. Dorsally, the bone is supplied by branches from the dorsalis pedis artery. Plantarly, the navicular is supplied by the medial plantar branch of the posterior tibial artery. The navicular tuberosity is supplied by a confluence of vessels from the dorsal and plantar vessels. A microangiographic study by Torg111 confirmed these findings and also noted there was a watershed area in the central third that was largely avascular. Sarrafian7 also noted that the number of vessels supplying the navicular decreased with age. The combination of poor central blood supply and the decreasing number of vessels with age contributes to the location and types of pathology seen in the navicular. However, a more recent study by McKeon et al71 that found that only 11.8% of the 60 cadavers that they tested had a watershed area in the central navicular. Avulsion fractures are caused by a forced plantar flexion of the inverted foot. This is a low-energy mechanism of injury. The talonavicular ligament creates a bony avulsion from the navicular as the foot is forcibly plantar flexed and rotated. This fracture pattern is also called a dorsal lip or “chip” fracture, and this is the most common fracture of the navicular. In the Eichenholtz and Levine35 series, such fractures represented 47% of all navicular fractures. Patients usually report a history of acute onset of pain and swelling, with difficulty walking and increased pain with plantar flexion. Physical examination reveals edema in the dorsal midfoot, with ecchymosis and focal tenderness upon palpation of the navicular and/or talonavicular joint. Three weight-bearing views (anteroposterior [AP], lateral, and lateral column oblique) radiographs of the foot should be obtained. The lateral radiograph will best demonstrate the displacement of the fracture, as seen Figure 40-3. When an avulsion fracture is seen, careful attention should be paid to the midfoot as well as the lateral ankle ligaments. Contaminant midfoot injuries and lateral ankle sprain are common. Eichenholtz and Levine35 as well as Richter et al93 have reported that these fractures do well with conservative treatment and can lead to good clinical outcomes in the long term. The avulsion fracture can be managed conservatively in most cases. Immobilization has been recommended by many authors, but the form of immobilization varies.40 If the size of the fragment is small, an elastic dressing may be applied. If the fragment is larger or if the patient is unable to tolerate the elastic dressing, a controlled ankle movement (CAM) walker boot or even a short-leg walking cast may be considered for additional support and immobilization. The duration of immobilization is dependent on the patient’s weight-bearing tolerance and the presence of concomitant injury to the midfoot or lateral ligaments, which will dictate the time until the patient can bear weight without immobilization. Typically, patients are immobilized for approximately 4 weeks; then they start progressive weight bearing as tolerated. Operative management is rarely indicated in the acute setting. The indications are finding an irreducible dislocation or significant midtarsal subluxation secondary to the size of the fracture fragment. A dorsally or medially based incision can be used to visual the fragment and to perform an open reduction, with placement of a lag screw (Fig. 40-4). When a lag screw is not possible, small fragment plates can the used to hold the piece in position while it heals. There can be problems with hardware prominence if wearing shoes, which, when symptomatic enough, may necessitate hardware removal after fracture union. Figure 40-4 A radiograph of a surgically treated navicular tuberosity fracture with 3.5-mm lag screws. In the chronic setting, surgical intervention should be considered if the patient has a nonunion of the fracture, a painful dorsal prominence, or late midtarsal subluxation. Most commonly, the fracture fragment is small and can simply be excised as recommended by Watson-Jones.115 Late midtarsal subluxation is also uncommon, but, if unable to be managed with longitudinal arch support, may require an arthrodesis of the talonavicular joint. Tuberosity fractures most commonly result from forced eversion of the foot. The inserting medial posterior tibial tendon and the deltoid, as seen previously in Figure 40-1A and B, cause the tuberosity to fail in tension.35,40 Patients report a history of a twisting mechanism and pain on the medial aspect of the foot. Pain with weight bearing is common, and pain is increased with active inversion of the foot. The physician can also passively evert the foot to see if the pain is re-created over the navicular tuberosity. Nonoperative management is the recommended treatment for the fractures by many authors.23,39,40 This is because most of the fractures are minimally displaced and, if the fracture does progress to a nonunion, the sequelae of late operative intervention are minor. Patients should be immobilized with partial weight bearing for 4 weeks. The type of immobilization varies, but reasonable treatment options, based on patient’s pain with weight bearing and comfort level, are an elastic dressing, a walker boot, or a short-leg walking cast. A longitudinal arch support can also be used to remove tension from the posterior tibial tendon. In the chronic setting, many patients with a radiographic nonunion will have a fibrous union and be asymptomatic. For patients with a symptomatic nonunion, a Kidner procedure can be performed, with excision of the nonunion fragment and advancement of the posterior tibial tendon to the prepared navicular body.88 The tendon can then be attached with suture anchors or drill holes and sutures. The postoperative protocol is similar to that of the acute repair. Because of the strong ligamentous attachments on the navicular, fractures of the navicular body are uncommon. The most common mechanism, described by multiple authors,35,67,81,98 is a direct axial load after a fall from height and landing on the foot. However, other mechanisms have also been proposed. Nadeu and Templeton80 as well as Eftekhar et al33 suggested a forcible plantar flexion with abduction of the midtarsal joints. This mechanism would lead to a vertical talar body fracture and dorsal dislocation of a portion of the navicular. Nyska81 went on to further describe this mechanism as a compression moment for the navicular between the cuneiform and the talar head. Still, Main and Jowett67 suggested that the mechanism of these injuries was based on “swivel” of the foot about the axis of the talocalcaneal ligament. This swivel, when combined with a longitudinal load, added the crushing component to the injury. They believed that these injuries occurred in a spectrum from nondisplaced fractures to a fracture-dislocation with secondary fractures of the cuneiforms. In their mechanism, the foot followed the deforming swivel force. Sangeorzan et al98 sought to classify these injuries radiographically. These fractures were differentiated by their degree and direction of displacement, number of articular fragments, alignment of the forefoot, and the presence of associated fractures. The result of that analysis was a classification system of three types. Type 1 is a fracture of the navicular that is transverse in the coronal plane with a resultant dorsal fragment that is less than 50% of the navicular body. On the AP radiograph, the medial border of the foot must not be disrupted, as seen in Figure 40-5. Figure 40-5 Classification of navicular body fractures according to Sangeorzan et al.98 A, Type 1. B, Type 2. C, Type 3. (From Hansen ST Jr, Swiontkowski MF: Orthopaedic trauma protocols, New York, 1993, Raven, p 361.) Type 2 fractures, which are the most common type, have a transverse fracture line from dorsolateral to plantar-medial. The major fragment is dorsomedial, with an often-comminuted plantar-lateral fragment. A key feature is an intact calcaneonavicular joint (see Fig. 40-5). Type 3 fractures have central or lateral comminution (see Fig. 40-5). The larger medial fragment is subluxated or dislocated, leading to a radiographic disruption of the medial border of the foot at the navicular cuneiform joint. There is often disruption or subluxation of the calcaneocuboid joint as well. Type 2 and 3 fractures can have apparent talar head displacement secondary to the rotation of the foot, with a shortened lateral column of the navicular. This lack of lateral column support leads to apparent hindfoot varus, as noted by Sanders and Hansen.96 If the patient’s foot is reasonably aligned, the status of the surrounding soft tissues will dictate the timing of surgery.30 The “wrinkle” test is most commonly used to assess when the soft tissue swelling has decreased adequately for surgical intervention. If reduction with percutaneous pinning is unsuccessful, external fixation can be used. External fixation allows for more stability of the fracture or the unstable dislocation. This technique is useful for patients with severe soft tissue injuries, grossly unstable fractures, significantly comminuted fractures, or to supplement internal fixation. The external fixation pins can be used to assist with reduction via ligamentotaxis. In a medial column external fixator, the pins are most commonly placed in the first metatarsal shaft and then either in the talus and/or the calcaneus. Figure 40-6 depicts a navicular body fracture that was fixed with lag screws and the addition of a medial column external fixator to help maintain medial column length. Internal fixation, which was once condemned, has now become the standard for displaced fractures. Historically, the treatment for all navicular fractures was nonoperative. This was then followed by Crossan’s24 recommendation for resection of the fracture fragments, despite their size. Multiple authors6,67,96,98 noted the late deformities that resulted and poor outcomes that led to medial column collapse, adduction, and a cavovarus foot. Bonvallet,14 in the 1950s, noted these poor outcomes at 6 to 12 months after fragment resection and the resultant iatrogenic flatfoot with degenerative arthritis. He began to advocate anatomic reduction and internal fixation. By the 1970s, Giannestras et al40 and Garcia et al39 noted that patient outcomes were improved with anatomic reduction and internal fixation when compared to closed reduction. Nadeau and Templeton80 also found that open reduction was superior to closed treatment. Therefore the current standard is for open reduction and internal fixation with lag screws, when feasible, and as soon as the soft tissues allow. This strategy reduces the potential for collapse of the medial column as well as the risk of nonunion and osseonecrosis. Arthrodesis of the talonavicular joint has a long history in the literature. In 1933, Wilson119 found that when the navicular could be reduced, primary talonavicular arthrodesis resulted in a painfree foot. In 1942, Dick 29 began to advocate for primary arthrodesis in all dorsally displaced navicular body fractures. Day26 performed an anatomic study in cadavers and found that arthrodesis of the talonavicular (TN) and naviculocuneiform (NC) joints results in a loss of nearly all of the inversion and eversion of the foot. His hypothesis was that patients with TN and NC fusions continued to have pain because of the unfused subtalar joint. Because of this belief, Day recommended a quadruple arthrodesis, with fusion of the TN, NC, subtalar, and calcaneocuboid joints. Currently, arthrodesis is generally reserved in the acute setting for the severely comminuted fractures that cannot be bridged because of instability. Eichenholtz and Levine35 as well as Main and Jowett67 recommended containing the fusion to the affected joints, that is, the TN and NC joints. Main and Jowett68 went on to recommend that the TN joint only be fused in cases of severe comminution because of the resultant loss of motion. Eichenholtz et al35 noted that only in rare circumstances did the fusion need to be extended to the subtalar joint. They also confirmed previous studies that found near-complete loss of inversion and eversion when this was done.35 In their study, patients with a triple arthrodesis never had a result better than “fair,” and this finding was confirmed by Nyska et al.81 Garcia and Parks39 recommended that the degree of articular cartilage damage should guide the surgeon in the decision of whether and where to fuse. Hansen31 has suggested an alternative to arthrodesis, which he describes as “ankylosis.” In this procedure, the fracture fragments are fixed with lag screws, and when there is inadequate bone for stability, the lag screws should be placed across the nonessential naviculocuneiform joints. However, in this technique, the joints are not formally prepared for arthrodesis, and the lag screws are removed when the fracture has healed. Arthrodesis does have a role in the delayed setting after failed conservative or operative management. Arthrodesis is useful for patients with posttraumatic arthritis, residual deformity after fracture union, or painful nonunion of the fracture. Further details and techniques for midfoot fusions can be found in Chapter 20. Displaced navicular body fractures are also treated surgically. Ideally, an anatomic reduction of the fracture and restoration of the TN and NC joints is performed through an incision between the tibialis anterior and tibialis posterior tendons.6,78,98 The reduction can be difficult to obtain. Understanding the vector of pull of the deforming tibialis anterior and tibialis posterior tendons is essential to reduction of the fracture. Assistance with manual traction or a temporary external fixator can be helpful to increase visualization. If these do not allow adequate exposure, a small-fragment distractor may be used (Synthes, Paoli, Pa.). The individual fragments can be manipulated with a combination of K-wires, pointed reduction forceps, and a dental tool. The reduction of the TN and NC joints should be examined carefully via a capsulotomy into each joint. The articular surface is inspected to determine whether a primary arthrodesis should be performed and is generally reserved for those patients whose cartilage is severely damaged. Fixation of the fracture should include lag screw placement and compression when possible. In general, adequate fixation can be achieved with use of 4.0-mm cancellous screws or 3.5-mm cortical screws. Use of 3.5-mm screws has been shown to have a lower chance of screw breakage because of the larger core diameter.31 Cannulated screws have limited indications because of issues with screw breakage and an inability to maintain adequate fixation. For small fracture fragments, mini-fragment screws or bioabsorbable screws can be used for fixation of intraarticular fragments. There are several new plates available that allow multiple screw configurations, as well as a variety of locking and nonlocking options. When placing lag screws in the navicular, careful attention must be paid to the radius of curvature. The navicular has a large radius of curvature, as can be seen in Figure 40-7A and B. Careful selection of a starting point for a lag screw will allow compression across simple fracture patterns and avoidance of the TN and NC joints. The largest series, covering a 25-year period, was published by Richter et al93 and included 155 patients with fractures of the midfoot; however, only 50 of these patients had navicular fractures. Richter et al found that these patients, with an average of 9 years’ follow-up, had significant disability, with average American Orthopaedic Foot and Ankle Society (AOFAS) scores of 71. However, patients with an isolated midfoot fracture had significantly (P < .05) better function than patients with Lisfranc or Chopart fracture dislocations. When analyzing the subgroup with navicular fractures, which were fixed anatomically, with restoration of the medial column, the AOFAS scores were closer to normal. Main and Jowett67 reported on 29 fractures of the navicular body. Fifteen of these fractures were longitudinal, and 14 were longitudinal and medial compression injuries. Twenty-four of the 29 fractures were displaced. Of these displaced fractures, 18 of 24 had fair or poor results. Displacement seemed predictive of outcome because all 5 nondisplaced fractures had good or excellent results. Sangeorzan et al98 reported on his experience with 21 navicular body fractures. These fractures were classified according to the classification system that they proposed. Fifteen of 21 patients had a satisfactory reduction. As the grade in the classification system increased from one to three, the likelihood of obtaining an anatomic reduction decreased. All of the type 1 fractures were reduced, 67% of the type 2, and only 50% of the type 3 fractures had a satisfactory reduction. However, in this series, patients had better outcomes than in other series. Of the 15 patients with satisfactory reduction, 14 had a good result, and the remaining patients had a fair outcome. Patients who did not have a satisfactory reduction had worse clinical outcomes. These authors concluded that the classification of the fracture and the quality of the reduction affect the patient’s outcome. Eichenholtz and Levine35 reported on their series of 67 navicular fractures over a 26-year period. Of interest, 13% of their patients didn’t initially have the foot imaged, and there was a delay in diagnosis. Twelve percent of the other patients had the foot imaged, but the navicular was not noted to be broken. Eichenholtz and Levine noted that these navicular fractures were best viewed from the lateral roentgenogram. In their series, they treated 19 navicular body fractures. Only 1 of these 19 cases was acutely repaired. The other 18 patients were treated conservatively. Five of these 18 patients went on to late arthrodesis, (3 had talonaviculocuneiform arthrodesis, and 2 had a triple arthrodesis). These authors were not able to draw any conclusions regarding surgical versus conservative management from their patient series but reported that late triple arthrodesis resulted in complete pain relief. Vaishya and Patrick113 have reported on cases of fracture dislocation isolated to the navicular.1 They have reported significant variability in the functional outcomes. One patient was able to hike more than 30 miles, whereas other patients had poor long-term results requiring further surgery. Stress fractures of the navicular were first reported in the 1970s. Towne112 described two cases of a fatigue fracture in 1970. Devas28 then reported two additional cases in 1975. Goergen at al41 reported two cases in running athletes. In their report, they treated one fracture with open reduction and internal fixation. Orava et al82 found only one case among 142 navicular fractures. They reported the incidence as 0.7% of these injuries. This rate of occurrence was challenged when, in 1981, Hunter51 reported that these injuries were more common than stated in Orava’s report and more frequent in running athletes. Later in the same year, Torg111 conducted a multicenter study that included 21 cases of navicular stress fracture. A 1994 report by Khan et al59 reported stress fractures and their high rate of occurrence in track and field athletes. Their report included an algorithm for diagnosis and treatment of these injuries. The mechanism, as with all stress fractures, is an overuse injury. Patients usually give a history of insidious onset of a pain in the midfoot or anterior ankle that is poorly defined. Some report a history of “cramping” or “soreness” in the dorsal midfoot or longitudinal arch with activity.51,59,111,132 Patients with a cavovarus foot position are at increased risk for this injury. Hunter50 found that when patients stand on their toes and exert a downward pressure on the metatarsal head, their symptoms are exaggerated. This could explain why these injuries are more common in track and field athletes who run on the forefoot. Several authors have emphasized the importance in timely diagnosis in athletes because failure of diagnosis may result in fracture displacement.51,59,69,111 Initial evaluation of the patient with a suspected navicular stress fracture should include weight-bearing AP, lateral, and lateral column oblique radiographs.111 The radiographs must be carefully examined for subtle radiolucent lines. A coned-down AP view of the navicular may also be helpful because greater penetration of the beam may lead to higher sensitivity of plain radiographs.51,111 It can be very difficult to differentiate between a bipartite navicular and a navicular stress fracture.51,111,112 A bipartite navicular is comma shaped and bent, as seen in Figure 40-8. The bipartite navicular also has a characteristic cleft from proximal plantar to distal dorsal, which creates a triangular wedge of bone dorsal to the body of the navicular. In contrast, a fatigue fracture occurs in the sagittal plane and most commonly in the central third of the bone.60 An example of this sagittal plane fracture can be seen in Figure 40-9. Radiographs are often negative in cases of fatigue fracture of the navicular, particularly at presentation. Figure 40-8 A and B, Anteroposterior and lateral radiographs of a patient with a bipartite navicular. Note the comma-shaped appearance and the dense sclerosis, indicating the chronic nature of the radiographic findings. C and D, A single sagittal computed tomography scan slice of the same patient, followed by a single representative axial slice. Again note the well-corticated edges of the bipartite navicular, in contradistinction to Figure 40-9, which shows an acute stress fracture. If plain radiographs are negative, a bone scan may be obtained.51,111 However, because of the cost and time of obtaining a bone scan, computerized tomography (CT) scans may be more helpful and more readily available.59,60 The CT scan can delineate the fracture line and amount of displacement. Complete fractures are most commonly in the sagittal plane in the central third of the navicular body, as seen in Figure 40-9.60 Incomplete fractures most commonly involve the dorsal cortex of the proximal articular surface.111 Both bone scans and CT scans can be helpful in distinguishing between stress fractures and a bipartite navicular. Magnetic resonance imaging (MRI) may also be helpful in distinguishing between a bipartite navicular when increased signal intensity is seen on the T2-weighted images. On the T1-weighted images, the clinician may be able to visualize a rounded edge to the fragment, which helps distinguish a bipartite navicular from the less sclerotic acute fracture. A study by Burne et al18 compared CT scans with MRIs for detection of navicular stress fractures and navicular stress reactions. They found that CT scans were more accurate in detecting stress fractures than MRI, but MRI was more sensitive for stress reactions, which may lead to earlier diagnosis and treatment. The literature on the treatment and results of navicular stress fractures is limited to small series. One of the largest series of surgically treated stress fractures is by McCormick et al.69 In this series, the authors reported on 10 surgically treated fatigue fractures. At greater than 3 years average follow-up, 8 out of 10 patients had gone onto radiographic union as shown by CT scan. The authors reported that completely displaced navicular stress fractures have a higher incidence of nonunion. Wiley and Brown117 also noted the difficulty in treating displaced navicular stress fractures. They presented three patients with stiff and painful feet secondary to displacement of the navicular fatigue fracture. Two of these patients had some relief from conservative treatment, and the remaining patient went on to have a triple arthrodesis. Many other authors have recognized the importance of preventing displacement of a navicular stress fracture. Hunter,51 Torg et al,111 and Khan et al59 recommended removing patients from athletic activities to prevent displacement. If the fracture was nondisplaced, the authors recommended strict non–weight bearing in a cast for 6 to 8 weeks. Kahn found that nonunion rates were low after immobilization and a 6-week rehabilitation program with a gradual return to activity. Torg et al111 and Hunter51 recommended that displaced fractures undergo open reduction and internal fixation. The recommended surgical technique described by McCormick et al69 and Torg et al111 is a dorsal approach to the navicular, with an open reduction and lag screw placement from the smaller lateral fragment to the larger medial fragment. In fractures with diastasis, autologous bone graft may be added to the mechanical stability afforded by the lag screw(s). The patient is then kept non–weight bearing for 6 to 8 weeks, with the option for a short-leg cast. The patient’s weight bearing is progressed in a walker boot once there are radiographic signs of callus formation. Patients generally initiate a return to an activity/sports program at 12 weeks postoperatively. Shoe modifications may include a shock-absorbing orthosis or a lateral heel wedge in the case of cavovarus. Pain is used as a guide for both an increase in weight bearing as well as return to sports. Because there were a number of small series detailing incomplete or complete but nondisplaced stress fractures, a meta-analysis was performed by Torg et al110 to establish an evidence-based treatment algorithm. Their results favored non–weight-bearing casting or surgery over weight-bearing casting (P < .0003). They found that there was no statistical difference between non–weight-bearing casts and surgical management. Torg et al recommended conservative treatment with non–weight-bearing casting as the standard of care for incomplete or completed but nondisplaced navicular stress fractures.110 The primary complication of stress fractures of the navicular is delayed union or nonunion. As reported by McCormick et al,69 the rate of nonunion in operatively treated fractures may be as high as 20%. Numerous authors have noted difficulty in healing these fractures in patients treated conservatively as well.36,52,59,111,117 Patients who have progression to nonunion will remain symptomatic with pain. Radiographs will usually demonstrate diastasis of fracture fragments in complete fractures. In incomplete fractures, there will be extension of the fracture fragments. Medullary cysts may also be present in nonunions, as seen in Figure 40-10. Fitch et al36 published a series of 19 patients treated with open en bloc resection of the fracture fragments, with addition of autologous allograft. Of the 15 patients with 1-year follow-up, 12 had been able to return to a preinjury level of activity. The long-term complications of a bipartite navicular in children who had a progressive nonunion was described by Wiley and Brown.117 These authors found that an untreated nonunion led to further displacement and deformity, similar to a comminuted navicular body fracture, with a progressive flatfoot deformity and medial column collapse. Their description was similar to the one by Brailsford,16 who thought that the deformity was due to osteochondritis or osteonecrosis. The treatment for the late deformity, as recommended by Wiley and Brown117 as well as Sanders and Hansen,96 is a triple arthrodesis. Sanders and Hansen96 also brought attention to the importance of correcting the varus hindfoot and adduction of the forefoot. They recommended a Dwyer calcaneal osteotomy with an iliac crest bone block graft to correct the varus hindfoot. They also noted that, in some cases, a quadruple arthrodesis may be necessary to fully correct a late deformity.
Fractures of the Midfoot and Forefoot
The Tarsal Navicular
Anatomy
Types of Fractures
Avulsion Fractures
Nonoperative Management
Operative Management

Navicular Tuberosity Fractures
Nonoperative Management
Operative Management
Navicular Body Fractures
Operative Management
Authors’ Preferred Method of Treatment
Results
Stress Fractures of the Tarsal Navicular
Mechanism of Injury
Radiographic Evaluation

Treatment and Results
Complications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fractures of the Midfoot and Forefoot