Fractures of The Midfoot and Forefoot
MIDTARSAL (CHOPART) JOINT
Epidemiology
Injuries to the midfoot are relatively rare.
the annual incidence of midfoot fractures is 3.6 per 100,000 population per year.
the most commonly fractured bone was the cuboid (50%), followed by the navicular (44%) and the cuneiform (6%).
The male-to-female ratio is 1:1.2.
Anatomy
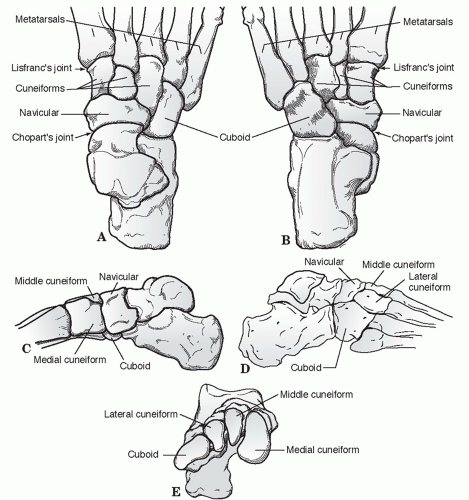
The midfoot is the section of the foot distal to Chopart joint line and proximal to Lisfranc joint line (Fig. 41.1).
Five tarsal bones comprise the midfoot: These are the navicular, cuboid, and the medial, middle, and lateral cuneiforms.
The midtarsal joint consists of the calcaneocuboid and talonavicular joints, which act in concert with the subtalar joint during inversion and eversion of the foot.
The cuboid acts as a linkage across the three naviculocuneiform joints, allowing only minimal motion.
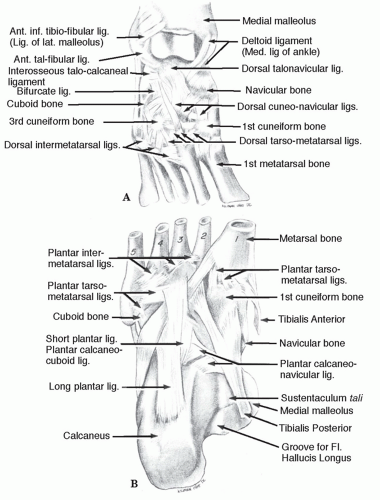
Ligamentous attachments include the plantar calcaneonavicular (spring) ligament, bifurcate ligament, dorsal talonavicular ligament, dorsal calcaneocuboid ligament, dorsal cuboideonavicular ligament, and long plantar ligament (Fig. 41.2).
Mechanism of Injury
High-energy trauma: This is most common and may result from direct impact from a motor vehicle accident or a combination of axial loading and torsion, such as during impact from a fall or jump from a height.
Low-energy injuries: This may result in a sprain during athletic or dance activities.
Clinical Evaluation
Patient presentation is variable, ranging from a limp with swelling and tenderness on the dorsum of the midfoot to nonambulatory status with significant pain, gross swelling, ecchymosis, and variable deformity.
Stress maneuvers consist of forefoot abduction, adduction, flexion, and extension and may result in reproduction of pain and instability.
Plantar ecchymosis is usually indicative of midfoot injury.
A careful neurovascular examination should be performed. In cases of extreme pain and swelling, serial examinations may be warranted to evaluate the possibility of foot compartment syndrome.
Radiographic Evaluation
Anteroposterior (AP), lateral, and oblique radiographs of the foot should be obtained.
Stress views or weight-bearing x-rays may help to delineate subtle injuries.
Computed tomography (CT) may be helpful in characterizing fracturedislocation injuries with articular comminution.
Magnetic resonance imaging (MRI) may be used to evaluate ligamentous injury and/or more subtle injuries.
Classification
Medial Stress Injury
Inversion injury occurs with adduction of the midfoot on the hindfoot.
Flake fractures of the dorsal margin of the talus or navicular and of the lateral margin of the calcaneus or the cuboid may indicate a sprain.
In more severe injuries, the midfoot may be completely dislocated, or there may be an isolated talonavicular dislocation. A medial swivel dislocation is one in which the talonavicular joint is dislocated, the subtalar joint is subluxed, and the calcaneocuboid joint is intact.
Longitudinal Stress Injury
Force is transmitted through the metatarsal heads proximally along the rays with resultant compression of the midfoot between the metatarsals and the talus with the foot plantarflexed.
Longitudinal forces pass between the cuneiforms and fracture the navicular typically in a vertical pattern.
Lateral Stress Injury
“Nutcracker fracture”: This is the characteristic fracture of the cuboid as the forefoot is driven laterally, crushing the cuboid between the calcaneus and the fourth and fifth metatarsal bases.
Most commonly, this is an avulsion fracture of the navicular with a comminuted compression fracture of the cuboid.
In more severe trauma, the talonavicular joint subluxes laterally, and the lateral column of the foot collapses because of comminution of the calcaneocuboid joint.
Plantar Stress Injury
Forces directed at the plantar region may result in sprains to the midtarsal region with avulsion fractures of the dorsal lip of the navicular, talus, or anterior process of the calcaneus.
Treatment
Nonoperative
Operative
High-energy mechanisms resulting in displaced fracture patterns often require open reduction and internal fixation (ORIF; e.g., with Kirschner wires or screws) and/or external fixation.
Prognosis is guarded, depending on the degree of articular incongruity.
Bone grafting of the cuboid may be necessary following reduction of lateral stress injuries.
Severe crush injuries with extensive comminution may require arthrodesis to restore the longitudinal arch of the foot.
Complications
Posttraumatic osteoarthritis may occur as a result of residual articular incongruity or chondral injury at the time of trauma. If severe and debilitating, it may require arthrodesis for adequate relief of symptoms.
TARSAL NAVICULAR
Epidemiology
Isolated fractures of the navicular are rare and should be diagnosed only after ruling out concomitant injuries to the midtarsal joint complex.
Anatomy
The navicular is the keystone of the medial longitudinal arch of the foot.
It is wider on its dorsal and medial aspect than on its plantar and lateral aspect.
The medial prominence known as the navicular tuberosity provides the attachment point for the posterior tibialis on its medial inferior surface.
An accessory navicular may be present in 4% to 12% of patients and should not be confused with an acute fracture.
Proximally, the articular surface is concave and articulates with the talus. This joint enjoys a significant arc of motion and transmits the motion of the subtalar joint to the forefoot. It is the point from which forefoot inversion and eversion are initiated.
The distal articular surface of the navicular has three separate broad facets that articulate with each of the three cuneiforms. These joints provide little motion; they mainly dissipate loading stresses.
Laterally, the navicular rests on the dorsal medial aspect of the cuboid with a variable articular surface.
Thick ligaments on its plantar and dorsal aspect support the navicular cuneiform joints. The spring ligament and superficial deltoid provide strong support to the plantar and medial aspects of the talonavicular joint.
Anatomic variants to be aware of when viewing the navicular involve the shape of the tuberosity and the presence of an accessory navicular (os tibiale externum). They are present up to 15% of the time, and bilateral 70% to 90%.
Mechanism of Injury
Direct blow, although uncommon, can cause avulsions to the periphery or crush injury in the dorsal plantar plane.
More often, indirect forces of axial loading either directly along the long axis of the foot or obliquely cause navicular injury.
Injury may result from a fall from a height or a motor vehicle accident. Stress fractures may occur in running and jumping athletes, with increased risk in patients with a cavus foot or calcaneal navicular coalition.
Clinical Evaluation
Patients typically present with a painful foot and dorsomedial swelling and tenderness.
Physical examination should include assessment of the ipsilateral ankle and foot, with careful palpation of all bony structures to rule out associated injuries.
Radiographic Evaluation
AP, lateral, medial oblique, and lateral oblique views should be obtained to ascertain the extent of injury to the navicular as well as to detect associated injuries.
If possible, the initial films should be weight bearing to detect ligamentous instability.
Medial and lateral oblique x-rays of the midfoot will aid in assessing the lateral pole of the navicular as well as the medial tuberosity.
CT may be obtained to better characterize the fracture.
MRI or technetium scan may be obtained if a fracture is suspected but not apparent by plain radiography.
Classification
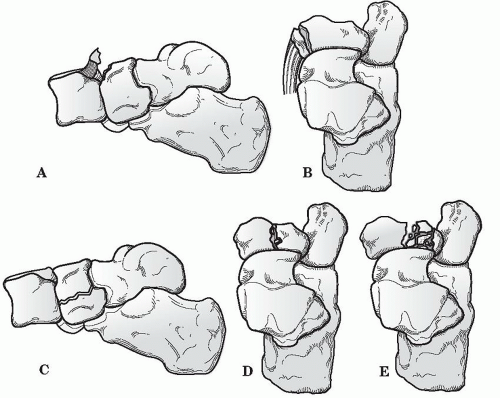
The most commonly used classification of navicular fractures is composed of three basic types with a subclassification for body fractures (Sangeorzan) (Fig. 41.3).
Avulsion-type fracture can involve either the talonavicular or naviculocuneiform ligaments.
Tuberosity fractures are usually traction-type injuries with disruption of the tibialis posterior insertion without joint surface disruption.
Type I body fracture splits the navicular into dorsal and plantar segments.
Type II body fractures cleave into medial and lateral segments. The location of the split usually follows either of the two intercuneiform joint lines. Stress fractures can usually be included in this group.
Type III body fractures are distinguished by comminution of the fragments and significant displacement of the medial and lateral poles.
Orthopaedic Trauma Association Classification of Navicular Fractures
See Fracture and Dislocation Classification Compendium at http://www.ota.org/compendium/compendium.html.
Anatomic Classification
Cortical Avulsion Fractures (Up to 50%)
Excessive flexion or eversion of midfoot results in a dorsal lip avulsion of the navicular by the talonavicular capsule and the anterior fibers of the deltoid ligament. This is seen as a part of ankle sprain continuum.
Symptomatic, small, nonarticular fragments may be excised. Large fragments (>25% articular surface) may be reattached with a lag screw.
Body Fractures (30%)
TUBEROSITY FRACTURES (20% TO 25%)
Forced eversion injury causes avulsion of the tuberosity by the posterior tibial tendon insertion or deltoid ligament.
This is often part of the “nutcracker fracture,” so concomitant midtarsal injury must be excluded.
One must rule out the presence of an accessory navicular, which is bilateral in 70% to 90% of cases.
If symptomatic, small fragments can be excised and the posterior tibial tendon reattached; larger fragments require ORIF with lag screw fixation, especially if posterior tibial tendon function is compromised.
Stress Fractures
These occur primarily in young athletes.
They frequently require bone scan or MRI for diagnosis.
The fracture line is usually sagittally oriented in the middle third and may be complete or incomplete.
Owing to increased incidence of persistent problems with pain and healing, screw fixation with autologous bone grafting should be used with comminuted fractures.
Treatment
The two most important criteria in obtaining a satisfactory outcome are maintenance or restoration of the medial column length and articular congruity of the talonavicular joint.
Nonoperative
Nondisplaced fractures of the navicular should be treated in a short leg cast or fracture brace with restricted weight bearing for 6 to 8 weeks.
Repeat radiographs should be obtained at 10 to 14 days after the initial injury to confirm the absence of bony or soft tissue instability.
If instability appears or other injuries become apparent, appropriate surgical intervention should be considered.
Operative
Surgical indications
Any unstable injury or fracture resulting in loss of position or articular congruity should be treated surgically.
Because the joint is concave, a 2-mm separation in any plane is considered incongruent. Most authors agree these injuries need to be managed aggressively with operative reduction.
Cortical avulsion fractures found to involve a significant portion of the dorsal anterior surface should be considered for operative treatment.
Surgical management
Individual fragments are stabilized using K-wires or mini-fragment screws.
Bone graft should be considered for crushed areas requiring elevation.
If anatomic restoration of 60% or more of the talonavicular surface can be achieved, an effort should be made to salvage the joint.
If more than 40% of the articular surface cannot be reconstructed, an acute talonavicular fusion should be considered.
Postoperative management
Cast or brace immobilization with non-weight bearing is recommended for 12 weeks.
Complications
These include nonunion, arthritic degeneration, late instability, loss of normal foot alignment through bony resorption or collapse, and osteonecrosis.
Osteonecrosis: The risk is increased with significantly displaced, markedly comminuted fractures. It may result in collapse of the navicular, with need for bone grafting and internal fixation.
Posttraumatic osteoarthritis may occur as a result of articular incongruity, chondral damage, or free osteochondral fragments.
NAVICULAR DISLOCATION
Isolated dislocation or subluxation of the navicular is rare.
The mechanism is hyperplantar flexion of the forefoot with subsequent axial loading.
Open reduction is usually necessary to restore both navicular position and articular congruity.
CUBOID FRACTURES
Epidemiology
Injury to the cuboid can occur as an isolated entity but is usually seen in association with injuries to the talonavicular joint or other midfoot structures or in conjunction with Lisfranc injuries.
Anatomy
The cuboid is part of the lateral support column of the foot.
The cuboid articulates with the calcaneus proximally, the navicular and lateral cuneiform medially, and the lateral two metatarsals distally.
Its plantar aspect forms a portion of the roof of the peroneal groove through which the peroneus longus tendon runs; scarring and irregularity of the peroneal groove caused by cuboid fracture may compromise function of peroneus longus tendon.
Mechanism of Injury
Direct: This is uncommon; trauma to the dorsolateral aspect of the foot may result in fractures of the cuboid.
Indirect: This accounts for most cuboid fractures.
“Nutcracker injury”: Torsional stress or forefoot abduction may result in impaction of the cuboid between the calcaneus and the lateral metatarsals.
Extreme plantar flexion may cause isolated sprain or dislocation of calcaneocuboid joint in high-velocity trauma, dance injuries, or patients with Ehlers-Danlos syndrome.
Stress fractures may occur in athletic individuals.
Clinical Evaluation
Patients typically present with pain, swelling, and tenderness to palpation at the dorsolateral aspect of the foot.
Palpation of all bony structures of the foot should be performed to rule out associated injuries.
Pain on the lateral aspect of the foot may be confused with symptoms of peroneal tendonitis in cases of stress fractures of the cuboid.
Radiographic Evaluation
AP, lateral, and oblique views of the foot should be obtained.
Multiple medial oblique radiographic views may be needed to see the articular outlines of both the calcaneocuboid and cuboid metatarsal joints.
As with other potential midfoot problems, weight-bearing or stress views should be obtained to rule out interosseus instability of surrounding structures.
A small medial or dorsal avulsion fracture of the navicular is considered a sign of possible cuboid injury.
A CT scan may be necessary to assess the extent of injury and instability.
An MRI or bone scan may be used for diagnosing a stress fracture.