CHAPTER 11 Fractures of the Clavicle
Although fractures of the clavicle typically do not pose a significant diagnostic dilemma, there have been few injuries with as much controversy in regard to treatment as this fracture. This clinical relevance is underscored when one considers that the clavicle is the most common fracture site in children,1,2 that an estimated 1 in 20 fractures involves the clavicle,3 and that fractures of the clavicle constitute as much as 44% of shoulder girdle injuries.4 Furthermore, it appears that the pattern of these fractures is changing, with fractures of much higher energy now being seen. Possibly as a consequence of this changing pattern, recent studies have shown poorer results with nonoperative treatment than with surgical intervention. There also seems to be a trend to recommend operative treatment for these more-displaced fractures.
HISTORICAL REVIEW
They act imprudently who think to depress the projecting end of the bone. But it is clear that the underpart ought to be brought to the upper, for the former is the movable part, and that which has been displaced from its natural position.5
A fractured clavicle, like all other spongy bone, gets speedily united; for all such bone forms callus in a short time. When, then, a fracture has recently taken place, the patients attach much importance to it, as supposing the mischief greater than it really is; but, in a little time, the patients having no pain, nor finding any impediment to their walking or eating, become negligent, and the physician, finding they cannot make the parts look well, take themselves off, and are not sorry at the neglect of the patients, and in the mean time the callus is quickly formed.5
Thou shouldst place him prostrate on his back with something folded between his shoulder blades, thou shouldst spread out with his two shoulders in order to stretch apart his collar bone until that break falls into place.1,3,6
Paul of Aegina, a 17th century Byzantine, reported that all that could ever be written about fractures of the clavicle had been written and that treatment included the supine position and the application of potions of olive oil, pigeon dung, snake oil, and other essences.3
Some of the earliest documented cases resulted from reports of riding accidents. William III in 1702 died of a fracture of the clavicle 3 days after falling when his horse shied at a molehill. Sir Benjamin Brodie described a “diffuse false venous aneurysm” that complicated a fracture of the clavicle in the case of Sir Robert Peel, who fell from his horse in 1850 on the way to Parliament. As Peel lapsed into unconsciousness, a pulsatile swelling rapidly developed behind the fracture, and his arm was paralyzed. The Lancet defended the physician’s handling of the case even though many skeptics doubted that death could occur from a clavicle fracture.7–9
In 1839, Dupuytren, a keen, though controversial anatomist and observer, noted that the cumbersome devices of his day used to hold the reduction were often unnecessary; he advocated simply placing the arm on a pillow until union occurred. Several devices at that time often appeared to aggravate the difficulty created by the fracture or seemed to engender new problems. Dupuytren described a case in which bleeding could not be arrested: “When I was summoned I merely removed the apparatus (the pressure of which was the cause of the mischief) and placed the arm on a pillow. The bleeding immediately ceased.”9,10 He railed against cumbersome and painful treatment methods.
In the late 1860s, the current ambulatory treatment (early mobilization of the patient) was described by Lucas Championniere, who advocated a figure-of-eight dressing and suggested that recumbency, a popular treatment method of his day, be abandoned.11 In 1871, Sayre, recognizing the difficulty in maintaining the reduction, advocated a method of ambulatory treatment involving a rigid dressing to maintain the reduction and support the extremity, a method that was echoed and taught in the textbooks of his time and still has many advocates.12
But while for a century and a half we see the most celebrated surgeons striving to prefer, or perhaps more strictly to complicate, the contrivances for treating fractured clavicle we may follow parallel to them another series of no less estimable surgeons, who disbelieving in these so-called improvements, return to the simplest means, as to Hippocrates before them. If now we seek to judge of all these contrivances by their results we see that most of them are extolled as producing cures without deformity; but we see also that subsequent experience has always falsified these promises. I therefore regard the thing (absence of deformity) as not impossible, although for my own part I have never seen such an instance.13
This quotation well summarizes the results of most conservative methods of treatment of the fractured clavicle—that is, most fractures unite by various treatment methods. However, many patients are left with residual deformity, some shortening, and a lump. Interference with function, cosmesis, activity level, and satisfaction used to be considered minimal, but more-recent studies have suggested that the satisfaction patients achieve after treatment of fractures of the clavicle might not be as high as we previously thought.14–16 In fact, Jesse Jupiter probably best summarized these shortcomings when he noted that “we are not meeting our patient expectations with current non-operative treatment.”17
Although ambulatory treatment of fractures of the clavicle with support of the arm remains the mainstay of care today, there are few other fractures in humans where as much deformity, angulation, and shortening are accepted as the standard of care. Recent studies have shown that nonoperative treatment of clavicle fractures has been associated with chronic pain, weakness, and overall dissatisfaction on the part of the patients.18,19 In a multicenter, prospective study, patients who were treated nonoperatively did significantly worse in terms of DASH (disabilities of the arm, shoulder, and hand) and Constant scores than those treated operatively.20 Moreover, the patients treated nonoperatively had a more than threefold increase in the rate of nonunion than the operative patients, and the nonoperative patients had a significant risk of malunion and significantly longer time to radiographic healing.20 Another study showed significant functional deficits in terms of DASH and Constant scores, with a strength deficit of 20% to 30% at an average follow-up of 55 months after conservative treatment of a clavicle shaft fracture.18 Although some of these deficits in patients with malunions and nonunions improved with delayed treatment, there were still significant deficits as compared to patients who were treated acutely.21 Other studies showed that displacement of more than one bone width was the most significant predictor of poor outcome in nonoperatively treated clavicle fractures,22 and less than half of the patients returned to their previous recreational and professional activities after a clavicle fracture.23
ANATOMY
Development
The embryology of the clavicle is unique in that it is the first bone in the body to ossify (fifth week of fetal life) and is the only long bone to ossify by intramembranous ossification without going through a cartilaginous stage.24–27 The ossification center begins in the central portion of the clavicle; this area is responsible for growth of the clavicle up to about 5 years of age.1,28 Epiphyseal growth plates develop at both the medial and lateral ends of the clavicle, but only the sternal ossification center is present radiographically.1,29 This medial growth plate of the clavicle is responsible for the majority of its longitudinal growth and probably contributes as much as 80% of the length of the clavicle.30 The sternal ossification center appears and fuses relatively late in life, with ossification occurring between the ages of 12 and 19 years and fusion to the clavicle occurring at 22 to 25 years of age.31,32 Thus, many of the so-called sternoclavicular dislocations in young adults are, in fact, epiphyseal fractures and are a potential source of confusion unless the late sternoclavicular epiphyseal closure is remembered.
MORPHOLOGY AND FUNCTION
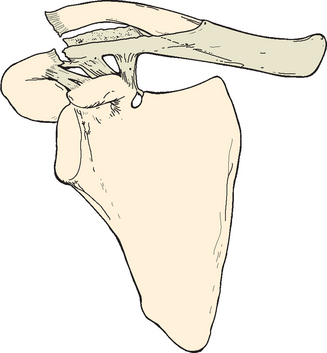
The superior surface of the clavicle is essentially subcutaneous over its course, with only the thin platysma providing any muscular coverage and then only to the inner two thirds of the bone. The supraclavicular nerves, which provide sensation to the overlying skin, are consistently found just deep to the platysma muscle layer. These nerves have been known to cause painful neuromas when damaged by fracture shards or iatrogenic injury (Fig. 11-1).33 The clavicle is the sole bone strut connecting the trunk to the shoulder girdle and arm, and it is the only bone of the shoulder girdle that forms a synovial joint with the trunk.34 Its name is derived from the Latin word clavis (key), the diminutive of which is clavicula, a reference to the musical symbol of similar shape.26
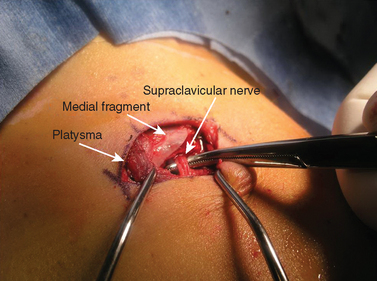
FIGURE 11-1 Surgical view of the middle branch of the supraclavicular nerve entrapped in the fracture site.
The shape and configuration of the clavicle are not only important for its function but also provide an explanation for the pattern of fractures encountered in this bone. In 1993, Harrington and colleagues35 described an image-processing system that was used to evaluate the histomorphometric properties of 15 adult male and female human clavicles. Variations in porosity, cross-sectional area, and anatomic and principal moments of inertia were assessed at 2.5% to 5% increments along the length of the bones. The clavicle’s biomechanical behavior (axial, flexural, and proportional rigidity and the critical forceful buckling) was modeled from these data by using beam theory. More than threefold variations in porosity and moments of inertia were found along the length of the S-shaped clavicle, with the greatest porosity and moments of inertia being located in the variably shaped sternal and acromial thirds of the bone as opposed to the denser, smaller, and more circular central third of the bone.
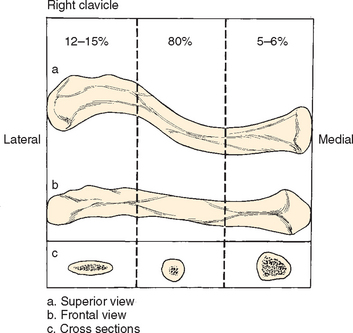
An analysis by Euler predicted a minimal critical force for buckling during axial loading of about two to three body weights for an average adult. Thus, buckling, or a combination of axial loading and bending or proportional loading, must be considered as a possible failure mechanism for this commonly injured bone.35 Although it appears almost straight when viewed from the front, when viewed from above, the clavicle appears as an S-shaped double curve that is concave ventrally on its outer half and convex ventrally on its medial half (Fig. 11-2). Even though some reports have noted differences in the shape and size of the clavicle in male and female subjects and in the dominant and nondominant arm, others have not found such to be the case or have discounted their clinical significance.30,34,36,37
DePalma found that the outer third of the clavicle exhibited varying degrees of anterior torsion and suggested that changes in torsion might be responsible for the altered stresses that lead to primary degenerative changes in the acromioclavicular joint.36 The cross section of the clavicle differs in shape along its length: It varies from flat along its outer third to prismatic along its inner third. The exact curvature of the clavicle and its thickness, to a high degree, vary according to the attachments of muscles and ligaments.34 The flat outer third is most compatible with pull from muscles and ligaments, whereas the tubular medial third is a shape consistent with axial pressure or pull. The junction between the two cross sections varies with regard to its precise location in the middle third of the clavicle. This junction is a weak spot, particularly with axial loading,34 which may be one of several reasons why fractures occur so commonly at the middle third. Another reason may be that it is an area not reinforced by muscles and ligaments and that it is just distal to the subclavius insertion.3,38,39 It is curious that nature has strengthened, through ligaments or muscular reinforcement, every part of the clavicle except the end of the outer part of the middle third, which is the thinnest part of the bone.40
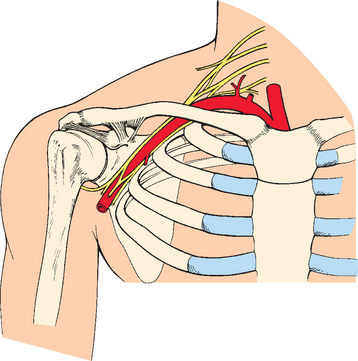
The clavicle articulates with the sternum through the sternoclavicular joint, which has little actual articular contact but surprisingly strong ligamentous attachments. The medial end of the clavicle is moored firmly against the first rib by the intra-articular sternoclavicular joint cartilage (which functions as a ligament), the oblique fibers of the costoclavicular ligaments, and to a lesser degree, the subclavius muscle.36 The scapula and clavicle are bound securely by both the acromioclavicular and coracoclavicular ligaments, the mechanism and function of which have been reported extensively, and these ligaments contribute significantly to movement and stability of the entire upper extremity (Fig. 11-3).41 The tubular third of the clavicle, which is thicker in cross section, offers protection for the important neurovascular structures that pass beneath the medial third of the clavicle. The intimate relationship between these structures and the clavicle assumes great importance both in acute fractures, in which direct injury can occur, and in the unusual fracture sequelae of malunion, nonunion, or production of excessive callus, in which compression of these structures can lead to late symptoms.
The brachial plexus, at the level at which it crosses beneath the clavicle, consists of three main branches (see Fig. 11-3). Of these branches, two are anterior. One (lateral) branch originates from the fifth, sixth, and seventh cervical roots and forms the musculocutaneous nerve and a branch of the median nerve; the other (medial) originates from the eighth cervical and first thoracic roots and forms another branch of the median nerve, the entire ulnar nerve, and the medial cutaneous nerve. The posterior branch of the plexus forms the axillary and radial nerves. The cord of the brachial plexus, which contains the first components of the ulnar nerve, crosses the first rib directly under the medial third of the clavicle. The other two cords are farther to the lateral side and posterior. Therefore, the ulnar nerve is more often involved in complications arising from fractures of the medial third of the clavicle.
The space between the clavicle and the first rib has been called the costoclavicular space. This space has been measured in gross anatomic studies and often appears to be quite adequate. However, it is not as large in a living subject as in a cadaver, possibly because in a living subject the vessels are distended and the dimensions of the cords of the brachial plexus are larger than in a cadaver. In addition, in a living subject the space is diminished as the first rib elevates because of contraction of the scalenus anticus. Hence, when the inner end of the outer fragment of the fractured clavicle is depressed, there is much less space between the first rib and the clavicle; the result is that the vessels (especially the subclavian and axillary vessels) and nerves (especially the ulnar nerve) are potentially subject to injury, pressure, or irritation.40 The internal jugular, which is adjacent to the sternoclavicular joint (see Fig. 11-3), is not usually injured with middle third fractures but has the potential for injury in more medial trauma involving the sternum and sternoclavicular joint. The subclavian vessels, because of their relative proximity to the medial third of the clavicle, can also be injured during operative treatment of clavicle fractures.42
The clavicle also appears to be unique as a long bone in that it has only a periosteal blood supply and little, if any, intramedullary or nutrient arterial blood supply. More importantly, the periosteal blood supply has been found to be primarily on the anterior and superior surface of the clavicle. This blood supply, coupled with the poor soft tissue coverage of the clavicle, may be an important consideration in fixation of the clavicle, particularly when significant soft tissue stripping is necessary.35,43
Surgical Anatomy
The surgical anatomy relative to the fascial arrangements about the clavicle has been extensively described by Abbott and Lucas.44 Such knowledge will reduce the risk of damage to neurovascular structures during surgical dissection.45 It is useful to divide these structures into areas above, below, and behind the clavicle.
Below the Clavicle
At the lower border of the subclavius, the two fascial layers join to form the costocoracoid membrane. This membrane fills a space between the subclavius above and the pectoralis minor below and is attached medially to the first costal cartilage and laterally to the coracoid process. Below, it splits into two layers that ensheathe the pectoralis minor. The costocoracoid membrane is pierced by the cephalic vein, the lateral pectoral nerve, and the thoracoacromial artery and vein.44
Behind the Clavicle
A continuous myofascial layer, which has not been commonly appreciated in surgical anatomy, lies in front of the large vessels and nerves as they pass from the root of the neck to the axilla. From above to below, this layer consists of the omohyoid fascia enclosing the omohyoid muscle and the clavipectoral fascia enclosing the pectoralis minor and subclavius muscles.44 Behind the medial part of the clavicle and the sternoclavicular joint, the internal jugular and subclavian veins join to form the innominate vein. These veins are covered by the omohyoid fascia and by its extension medially over the sternohyoid and sternothyroid muscles. Behind the clavicle, at the junction between the middle and medial thirds, the junction of the subclavian and axillary veins lies very close to the clavicle and is also protected by this myofascial layer.
Between the omohyoid fascia posteriorly and the investing layer of cervical fascia anteriorly is a space, described by Grant, in which the external jugular vein usually joins the subclavian vein at its confluence with the internal jugular vein.46 Before this junction, the external jugular is joined on its lateral aspect by the transverse cervical and scapular veins and on its medial aspect by the anterior jugular vein. This anastomosis usually lies just behind the fascial envelope and the angle formed by the posterior border of the sternocleidomastoid muscle and clavicle.2
FUNCTION
[W]e are proud that our brains are more developed than the animals: we might also boast of our clavicles. It seems to me that the clavicle is one of man’s greatest skeletal inheritances, for he depends to a greater extent than most animals, except the apes and monkeys, on the use of his hands and arms.47
Mammals that depend on swimming, running, or grazing have no clavicles, whereas species with clavicles appear to be predominantly fliers or climbers. Codman theorized that animals with strong clavicles needed to use their arms more in adduction and abduction. The long clavicle may facilitate placement of the shoulder in a more lateral position so that the hand can be positioned more effectively to deal with the three-dimensional environment.48
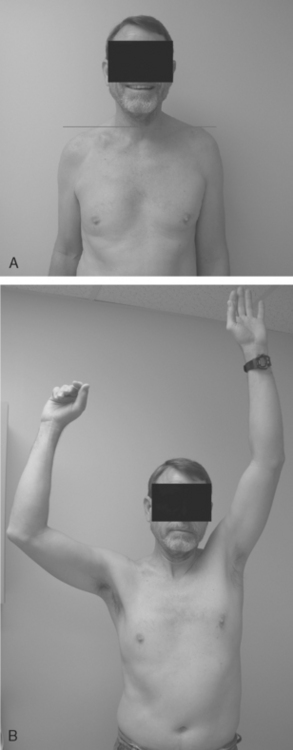
The teleologic role of the clavicle has been disputed, however, because of reports of entirely normal function of the upper limb after complete excision of the clavicle.49–51 These reports, combined with observations in patients with congenital absence of the clavicle (cleidocranial dysostosis) who do not appear to have any impairment in limb function, are probably responsible for the often-stated belief that this bone is a surplus part that can be excised without any disturbance in function. However, others have noted drooping of the shoulder, weakness, and loss of motion after excision of the clavicle and have used these observations to attribute to the clavicle its important role in normal function of the extremity (Figs. 11-4 and 11-5).52,53
Power and Stability of the Arm
The clavicle, by serving as a bony link from the thorax to the shoulder girdle, provides a stable linkage of the arm–trunk mechanism and contributes significantly to the power and stability of the arm and shoulder girdle, especially in movement above shoulder level.27 It transmits the support and force of the trapezius muscle to the scapula and arm via the coracoclavicular ligaments.
Although patients with cleidocranial dysostosis and absence of the clavicle do not appear to have significantly decreased range of motion and can, in fact, have an increase in protraction and retraction of the scapula (because of absence of the clavicle), they can exhibit some weakness in supporting a load overhead. This limitation further suggests that the clavicle adds stability to the extremity under load in extreme ranges of motion.51
The clavicle is predominantly supported and stabilized by passive structures,34 particularly the sternoclavicular ligaments.54,55 Although evidence of trapezius muscle activity at rest has been demonstrated electromyographically, thus suggesting a role for that muscle in support of the clavicle,54 other authors have not been able to demonstrate that muscle activity plays any role in supporting the clavicle.
Motion of the Shoulder Girdle
When the arm is elevated 180 degrees, the clavicle angles upward 30 degrees and backward 35 degrees at the sternoclavicular joint. It also rotates upward on its longitudinal axis approximately 50 degrees. During combined glenohumeral, acromioclavicular, and sternoclavicular movement, the humerus moves approximately 120 degrees at the glenohumeral joint and the scapula moves along the chest wall approximately 60 degrees. These complex and combined simultaneous movements of the joints and their articulating bony structures (scapula, humerus, and clavicle) seem to imply an important role for the clavicle in range of motion of the arm. This role is debatable, however, because it has been observed by some that loss of the clavicle does not in fact impair abduction of the arm at all44,56 and that excision of the clavicle can permit range of motion just as well. However, Rockwood has observed loss of the clavicle to result in disabling loss of function, weakness, drooping of the arm, and pain secondary to irritation of the brachial plexus (see Figs. 11-4 and 11-5).52
It has been stated that its contribution to motion may be the most important function of the clavicle and that this role is related to its curvature, especially its lateral curvature. The 50-degree rotation of the clavicle on its axis appears to be important for free elevation of the extremity. In fact, a direct relationship has been found among the line of attachment of the coracoclavicular ligaments, the amount of clavicular rotation, the extent and relative lengthening of the ligaments, and scapula rotation itself. Of the total 60 degrees of scapular rotation, the first 30 degrees is due to elevation of the clavicle as a whole by movement of the sternoclavicular joint, and the second 30 degrees is permitted through the acromioclavicular joint by clavicular rotation and elongation of the coracoclavicular ligaments. Thus, the lateral curvature of the clavicle permits it to act as a crankshaft, effectively allowing half of scapular movement.57
The smooth, rhythmic movement of the shoulder girdle is a complex interaction of muscle groups acting on joints and both the subacromial and scapulothoracic spaces. Although it is difficult to break down all the contributions of the clavicle to total motion of the shoulder, it appears that its geometric and kinematic design, by permitting rotation, maximizes the stability of the upper limb against the trunk while permitting mobility, particularly of the scapula along the chest wall. The practical result is that the glenoid fossa continually moves, facing and contacting the humeral head as the arm is used overhead.51
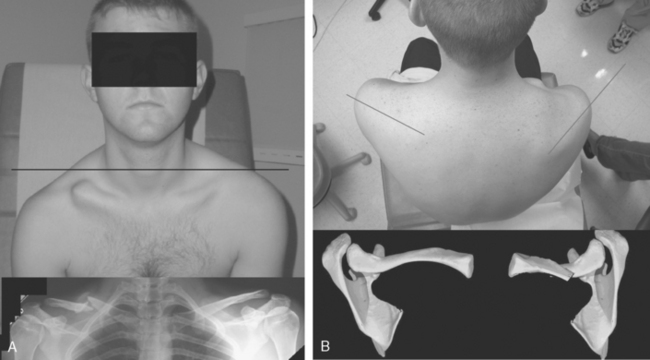
Nonunion and malunion can cause significant alterations in orientation of the scapula and glenohumeral joint58,59 (Figs. 11-6 and 11-7). This altered orientation is typically an anteromedial and inferior rotatory deformity. Malunion represents a fixed or static change in orientation of the scapula, whereas nonunion is a dynamic deformity, much as one would see in a significant acromioclavicular separation (Figs. 11-8 and 11-9). This change in orientation of the scapula results in a change in the resting length of the muscles about the shoulder. Basamania60 and McKee16 found significant weakness in the affected limbs of patients with clavicle malunion, regardless of the time since their injury. This weakness corrected with return of the clavicle to its normal length in spite of no formal physical therapy.
Muscle Attachments
The clavicle also acts as a bony framework for muscle origin and insertion. The upper third of the trapezius inserts on the superior surface of the outer third of the clavicle, opposite the site of origin of the clavicular head of the deltoid along its anterior edge. The clavicular head of the sternocleidomastoid muscle arises from the posterior edge of the inner third of the clavicle. The clavicular head of the pectoralis major muscle arises from the anterior edge of the clavicle. During active elevation of the arm, these muscles contract simultaneously. It has been suggested that in theory, the muscles above the clavicle could be directly attached to the muscles below the clavicle as a continuous muscular layer without an interposed bony attachment,44 but the stable bony framework clearly provides the advantage of a solid foundation for muscle attachment.
Protection of Neurovascular Structures
The clavicle also provides skeletal protection for adjacent neurovascular structures and the superior aspect of the lung. The subclavian and axillary vessels, the brachial plexus, and the lung are directly behind the medial third of the clavicle. The tubular cross section of the medial third of the clavicle increases its strength and adds to its protective function at this level. The anterior curve of the medial two thirds of the clavicle provides a rigid arch beneath which the great vessels pass as they move from the mediastinum and thoracic outlet to the axilla. It has been shown that during elevation of the arm, the clavicle, as it rotates upward, also moves backward, with the curvature providing increased clearance for the vessels.61 Loss of the clavicle eliminates this bony barrier against external trauma.62 In addition, loss of the clavicle can cause exacerbation of thoracic outlet symptoms because of drooping of the shoulder and resultant draping of the brachial plexus over the first rib (see Figs. 11-3 and 11-4).
Respiratory Function
Elevation of the lateral part of the clavicle results in increased pull on the costoclavicular ligament and subclavius muscle. Because of the connection between the clavicle and the first rib and between the first rib and the sternum, elevation of the shoulder girdle brings about a cephalad motion of the thorax corresponding to an inspiration. This relationship is used in some breathing exercises and in some forms of artificial respiration.44
Cosmesis
By providing a graceful curve to the base of the neck, the smooth, subcutaneous bony clavicle serves a cosmetic function. After surgical excision of the clavicle, the upper limb in some patients falls downward and forward and gives a foreshortened appearance to this area. Female patients have complained of difficulty keeping their bra strap on their affected shoulder because of this drooping (see Figs. 11-4 and 11-5). The cosmetic function of the clavicle is noted by many patients who are concerned by excessive formation of callus after a clavicle fracture or by deformity after clavicular malunion (see Fig. 11-9).62
CLASSIFICATION OF CLAVICLE FRACTURES
To be effective, a classification system should be accurate in terms of identifying the pathologic anatomy, and it should be able to predict outcome, thereby serving as a basis for deciding on proper treatment. Ideally, a classification system should also be sufficiently straightforward that it is easily reproducible with good intraobserver and interobserver reliability. Unfortunately, most clavicle fracture classification systems are merely descriptive and give no guidance in terms of prognosis. Although clavicle fractures have been classified by fracture configuration (e.g., greenstick, oblique, transverse, comminuted),63 the usual classification is by location of the fracture because location appears to better compartmentalize our understanding of fracture anatomy, mechanism of injury, clinical findings, and alternative methods of treatment.64–68 One of the early classifications of clavicle fractures was Allman’s classification. He divided these fractures into three groups64:
Group I: Fractures of the middle third
Group II: Fractures of the distal third
Group III: Fractures of the medial third
Neer3,67,69,70 and Jager and Breitner71 devised a specific classification for fractures of the distal third of the clavicle.
Craig’s Classification
In 1990, Craig72 introduced a more detailed classification of clavicle fractures that was based on the variable fracture patterns seen within the three broad groups of Allman’s clavicle fracture classification (Box 11-1).
BOX 11-1 Craig’s Classification of Clavicle Fractures
Group II: Fracture of the Distal Third
Type I: Minimal displacement (interligamentous)
Type II: Displaced secondary to a fracture medial to the coracoclavicular ligaments
Type III: Fractures of the articular surface
Type IV: Ligaments intact to the periosteum (children), with displacement of the proximal fragment
Group I Fractures
Group I fractures, or fractures of the middle third, are the most common fractures seen in adults and children. They occur at the point at which the clavicle changes to a flattened cross section from a prismatic cross section. The force of the traumatic impact follows the curve of the clavicle and disperses on reaching the lateral curve.73–76 In addition, the proximal and distal segments of the clavicle are mechanically secured by ligamentous structures and muscular attachments, whereas the central segment is relatively free. This fracture accounts for 80% of clavicle fractures.3,4
Group II Fractures
Group II fractures account for 12% to 15% of all clavicle fractures and are subclassified according to the location of the coracoclavicular ligaments relative to the fracture fragments.77 Neer first pointed out the importance of this fracture while subdividing it into four types.
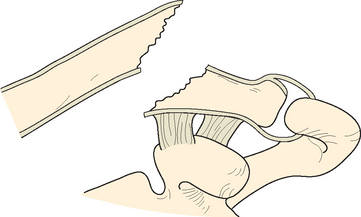
Type I fractures are the most common by a ratio of 4 : 1. In this fracture, the ligaments remain intact to hold the fragments together and prevent rotation, tilting, or significant displacement. This fracture is an interligamentous fracture that occurs between the conoid and the trapezoid or between the coracoclavicular and acromioclavicular ligaments (Figs. 11-10 and 11-11).70
FIGURE 11-10 Type I fracture of the distal end of the clavicle (group II). The intact ligaments hold the fragments in place.
(From Rockwood CA, Green DP [eds]: Fractures [3 vols], 2nd ed. Philadelphia: JB Lippincott, 1984.)
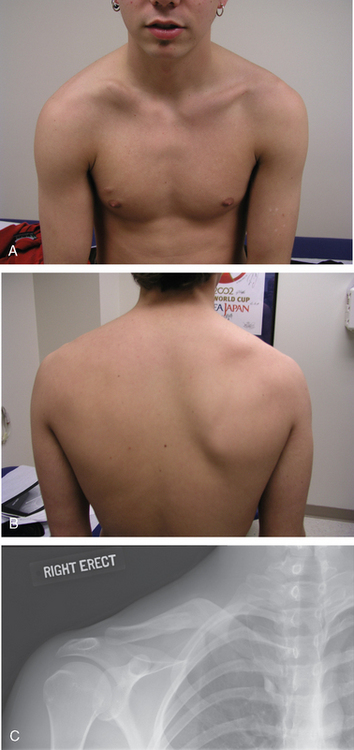
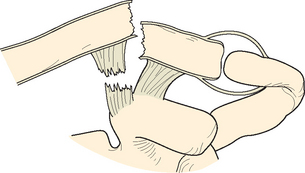
In type II distal clavicle fractures, the coracoclavicular ligaments are detached from the medial segment. Both the conoid and trapezoid may be on the distal fragment (IIA) (Fig. 11-12), or the conoid ligament may be ruptured while the trapezoid ligament remains attached to the distal segment (IIB) (Fig. 11-13).1 There is really no functional difference between these two fractures. The high rate of nonunion in these fractures may be secondary to excessive motion at the fracture site. These fractures are equivalent to a serious acromioclavicular separation in which the normal constraints to anteromedial rotation of the scapula relative to the clavicle are lost.
Four forces that may impair healing and may be contributing factors to the reported high incidence of nonunion act on this fracture: When the patient is erect, the outer fragment, which retains the attachment of the trapezoid ligament to the scapula through the intact acromioclavicular ligaments, is pulled downward and forward by the weight of the arm; the pectoralis major, pectoralis minor, and latissimus dorsi draw the distal segment downward and medially, thereby causing overriding; the scapula might rotate the distal segment as the arm is moved; and the trapezius muscle attaches to the entire outer two thirds of the clavicle, whereas the sternocleidomastoid muscle attaches to the medial third, and these muscles act to draw the clavicular segment superiorly and posteriorly, often into the substance of the trapezius muscle.67
Type III distal clavicle fractures involve the articular surface of the acromioclavicular joint alone. Although type II fractures can have intra-articular extension, type III fractures are characterized by a break in the articular surface without a ligamentous injury. A type III injury may be subtle, may be confused with a first-degree acromioclavicular separation, and can require special views to visualize. In fact, it may be manifested as late degenerative joint arthrosis of the acromioclavicular joint. In addition, it has been suggested that weightlifter’s clavicle, or resorption of the distal end of the clavicle, might occur from increased vascularity secondary to the microtrauma or microfractures that lead to such resorption.3,78–80
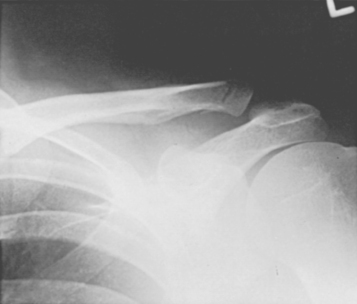
Type IV fractures occur in children and may be confused with complete acromioclavicular separation (Fig. 11-14). Called pseudodislocation of the acromioclavicular joint, these fractures typically occur in children younger than 16 years.81 The distal end of the clavicle is fractured, and the acromioclavicular joint remains intact. In children and young adults, the attachment between bone and the periosteum is relatively loose. The proximal fragment ruptures through the thin periosteum and may be displaced upward by muscular forces. The coracoclavicular ligaments remain attached to the periosteum or may be avulsed with a small piece of bone.65,66,81
Group III Fractures
Group III fractures, or fractures of the inner third of the clavicle, constitute 5% to 6% of clavicle fractures. As with distal clavicle fractures, they can be subdivided according to the integrity of the ligamentous structures. If the costoclavicular ligaments remain intact and attached to the outer fragment, little or no displacement develops.64,82 When these lesions occur in children, they are usually epiphyseal fractures.83 In adults, articular surface injuries can also lead to degenerative changes.3,84
Panclavicular dislocation, or a traumatic floating clavicle, is neither a clavicle fracture nor an isolated sternoclavicular or acromioclavicular separation.85–89 In this injury, both sternoclavicular ligaments and the coracoclavicular and the acromioclavicular ligamentous structures are disrupted.
Rockwood’s Classification
Clinically and radiographically, it may be impossible to distinguish between grade III acromioclavicular separations, type II fractures of the distal end of the clavicle, and type IV fractures involving rupture of the periosteum.3,67,70 Rockwood has classified these fractures in a manner that is roughly analogous to his classification system for acromioclavicular joint injuries in adults (Fig 11-15) (see Chapter 12). This system is based on the amount of energy imparted to the distal part of the clavicle, which determines the degree of displacement, and the direction of the applied force, which determines the direction of the displacement. The subtypes are based on the position of the distal end of the clavicle relative to the periosteal tube.81
Type I is a minor strain of the acromioclavicular ligaments without disruption of the periosteal sleeve of the clavicle. A patient with this injury might have tenderness to palpation of the acromioclavicular joint but no significant side-to-side radiographic changes.
Type V is essentially a severe type III injury with complete disruption of the dorsal periosteal tube and significant superior displacement of the distal part of the clavicle relative to the acromion. This injury is presumably due to the additional disruption of the deltotrapezial fascia. Again, the distal end of the clavicle really stays in its anatomic position but the scapula drops away. The coracoclavicular interval is typically increased more than 100%. In type V fractures in adults, neither of the main fracture fragments has a functional coracoclavicular ligament. These fracture fragments are displaced by the deforming muscles as in type I distal clavicle fractures, but the coracoclavicular ligaments are intact and remain attached to a small, third comminuted intermediary segment.68 This fracture is thought to be more unstable than type II distal clavicle fractures.
Robinson’s Classification
The classification proposed by Robinson (Fig. 11-16) is perhaps the only validated classification system in terms of correlating the type of fracture with the typical outcome.45 His system was based on the observation of 1000 adult clavicle fractures and takes into account the anatomic site, extent of displacement, comminution, and articular extension and stability of the fracture.
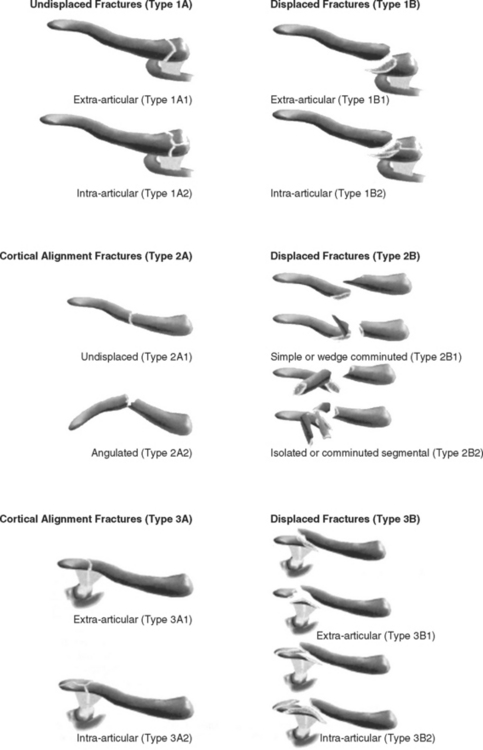
FIGURE 11-16 Robinson classification of clavicle fractures.
(From Robinson CM: Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 80:476-484, 1998.)
Much like Allman’s classification, the primary anatomic sites are medial (type 1), middle (type 2), and lateral (type 3). Displacement further subdivides these primary groups if they are displaced less than 100% (subgroup A) or more than 100% (subgroup B). Type 1 and 3 fractures are subdivided with regard to their articular involvement, with subgroup 1 being no intra-articular involvement and subgroup 2 having intra-articular extension. Type 2 fractures are subdivided with regard to their comminution. Simple or wedge comminution is subgroup 1, and segmental or comminuted fractures are subgroup 2.
By combining these groups and subgroups, virtually all fractures can be described. For example, a comminuted, displaced midshaft fracture is described as a type 2B2 fracture, and a nondisplaced intra-articular lateral clavicle fracture is a type 3A2. Robinson found that both displacement and comminution were associated with an increased risk of delayed union or nonunion.45
MECHANISM OF INJURY
Because the clavicle is the bone that is most often fractured, numerous causes of fracture of the clavicle, both traumatic and nontraumatic, have been reported.90
Trauma in Children
Birth Fractures
In 15,000 deliveries from 1954 to 1959, Rubin found that fractures of the clavicle were the most common injury at birth.91 Although it has been stated that intrapartum traumatic injuries are decreasing as a result of improvements in obstetric care,41,92–95 the incidence of clavicle fracture remains quite high, and in infants it might actually be increasing.96 Moir and Myerscough found an incidence of clavicle fractures of 5 per 1000 vertex births, which increased to 160 per 1000 with a breech presentation.97 The mechanism of injury in a full-term newborn infant delivered vaginally, when the baby is in a cephalic presentation, is compression of the leading clavicle against the maternal symphysis pubis.98,99 In a breech delivery, direct traction can occur and produce the same bone injury as the obstetrician tries to depress the shoulders and free the arm during delivery of the head.100,101
The overall incidence of fracture of the clavicle during birth is approximately 0.5 to 7.2 per 1000 births. In addition to the presentation of the infant, several factors appear to be involved. Birth weight clearly plays a role because the incidence of fractures of the clavicle increases with increasing birth weight and in larger babies.102,103 Babies who weigh 3800 to 4000 g or measure 52 cm or longer seem to be at higher risk for fracture. Increased maternal age has likewise been shown to be a risk factor for birth fracture.104 The experience of the physician is probably also related. Cohen and Otto reported an increased incidence of fractures of the clavicle when babies were delivered by less-experienced residents, and a decrease in incidence was noted for each year of obstetrics experience.105 This statistic certainly merits consideration in obstetrics house staff training. The method of delivery is also important because of an increase in the risk of fracture with midforceps deliveries, which calls into question the wisdom of this obstetric maneuver. On the other hand, Balata and coworkers noted no fractures in babies delivered by cesarean section.96
Fracture of the clavicle does not seem to be related to the type of anesthesia, length of active labor, length of second-stage labor, Apgar score, or parity of the mother. The exact anatomy of fractures that occur during delivery varies, and incomplete, greenstick, and bicortical disruptions with or without displacement have all been reported.2 In one study, boys were more commonly affected than girls, and the right clavicle was fractured more often than the left clavicle.96 In 1992, a study suggested a relationship between fractures of the clavicle and mothers with a second childbirth.106
Injuries in Infancy and Childhood
Fractures of the clavicle are particularly common in childhood, and almost half occur in children younger than 7 years.107 Fractures commonly result from a fall on the point of the shoulder or on an outstretched hand. In younger children, such a fall is not uncommonly from a highchair, bed, or changing table. The fracture is occasionally caused by a direct violent force applied from the front of the clavicle; like other fractures of long bones, fractures of the clavicle may be one of several signs of trauma in a physically abused child.
Unlike the situation in adults, direct and indirect trauma to a child’s clavicle can result in incomplete or greenstick fractures rather than displaced fractures.75 In addition, trauma to a child’s clavicle can result in plastic bowing alone without evident cortical disruption. Despite an initial appearance of only bowing, on later examination these fractures usually show evidence of gross healing of complete fractures, with obvious callus visible on radiographs.108,109
Trauma in Adults
The incidence of fractures of the clavicle in adults appears to be increasing because of several factors, including the occurrence of many more high-velocity vehicular injuries and the increase in popularity of contact sports.36 The mechanism of injury of fractures of the clavicle in adults has been widely reported to consist of either direct or indirect force. It has generally been assumed that the most common mechanism of fractures in adults is a fall onto the outstretched hand.36 Allman, in dividing fractures of the clavicle into three groups, proposed different mechanisms of injury for each group.64 He thought that in group I (fractures of the middle third), the most common mechanism of injury is a fall onto an outstretched hand, with the force being transmitted up the arm and across the glenohumeral joint and dispersing along the clavicle. Group II fractures, those distal to the coracoclavicular ligaments, occur from a fall on the lateral aspect of the shoulder that drives the shoulder and scapula downward. Group III fractures, or proximal clavicle fractures, are usually due to direct violence caused by a force applied from the lateral side.
In 1994, Nordqvist and Petersson investigated the incidence of fractures of the clavicle. They reviewed 2035 fractures that occurred between 1952 and 1987.110 The fractures were classified into three groups according to the Allman system.64 Each group was further divided into nondisplaced fracture subgroups, with an extra subgroup of comminuted midclavicle fractures in group I. Of the fractures, 76% were classified as Allman group I. The median age of patients in this group was 13 years. Significant differences in age- and gender-specific incidence were noted between the nondisplaced, displaced, and comminuted fracture subgroups. Allman group II accounted for 21% of fractures. The median age of these patients was 47 years, and no difference in age was found between the subgroups with nondisplaced and displaced fractures. Three percent of the fractures were classified as Allman group III, and the median age of patients in this group was 59 years. All three groups were characterized by a significant preponderance of male patients.
A study by Nowak in 2000 showed that the incidence of clavicle fractures in Uppsala, Sweden, was 50 per 100,000 population; however, the incidence in male patients was 71 per 100,000, and the incidence in female patients was 30 per 100,000.111,112 Bicycle accidents were the most common cause of injury, and male patients tended to be younger and to have more comminuted, high-energy injuries. Most (75%) of the injuries were midshaft fractures, and the nonunion rate was 5%.
In 1962, Fowler113 pointed out that all clavicular injuries almost always follow a fall or a blow on the point of the shoulder, whereas a blow on the bone itself is rarely a cause (although a direct blow has certainly been recognized in sports, particularly in stick sports such as lacrosse and hockey114). In a large series of fractures of the clavicle (342 patients) studied by Sankarankutty and Turner, 91% sustained a fall or blow to the point of the shoulder, whereas only 1% had a fall onto the outstretched hand.115
More recently, Stanley and colleagues studied a consecutive series of 150 patients with fractures of the clavicle; 81% of the patients described information about the mechanism of injury.116 The researchers found that 94% had fractured the clavicle from a direct blow on the shoulder, whereas only 6% had fallen onto an outstretched hand. Further biomechanical analysis of the force involved in fracture of the clavicle by this group revealed that direct injury produces a critical buckling load that is exceeded at a compression force equivalent to body weight and thereby results in fracture of the bone. When force is applied along the axis of the arm, the buckling force is rarely reached in the clavicle. These investigators recorded fractures at every site along the clavicle with a direct injury to the point of the shoulder and found little support for Allman’s concept that fractures at different anatomic sites have different mechanisms of injury. In addition, they theorized that a direct blow to the shoulder might even be the mechanism of injury in those who described a fall on the outstretched hand: as the hand makes contact with the ground, the patient’s body weight and falling velocity are such that the fall continues, with the shoulder becoming the upper limb’s next point of contact with the ground.
Harnroongroj and coworkers found that when clavicles were axially loaded, they tended to fracture at the middle third of the clavicle in the region where the curve of the lateral aspect of the clavicle changes to the curve of the medial aspect of the clavicle.117 The force required to fracture the clavicle was 1526.19 N. The ratio of the lateral fragment to the total length of the clavicle was 0.49.
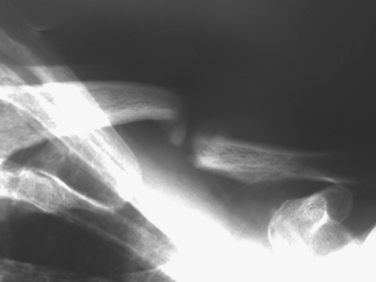
Another indirect mechanism of fracture of the clavicle is a direct force applied to the top of the shoulder; the clavicle is forced against the first rib, and a spiral fracture of the middle third is often produced.36 Another variation of this mechanism is what we refer to as seat-belt fractures. The shoulder strap from the seat belt acts as a fulcrum, typically at the midpoint of the clavicle, and the forward force of the clavicle against this fulcrum causes the clavicle to fracture in a transverse or oblique pattern with little or no comminution. Although we cannot explain why, it appears that this fracture is more prone to nonunion than a more typical fracture is (Fig 11-17). It may be because the amount of energy required to cause a transverse fracture is more than that required to cause a fracture as one sees with an axial load.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree