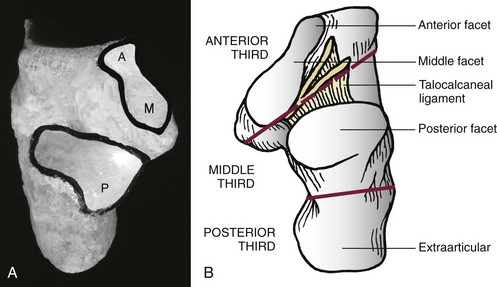
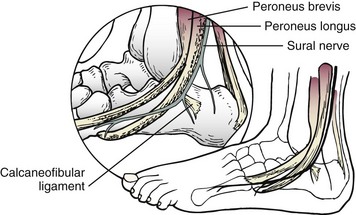
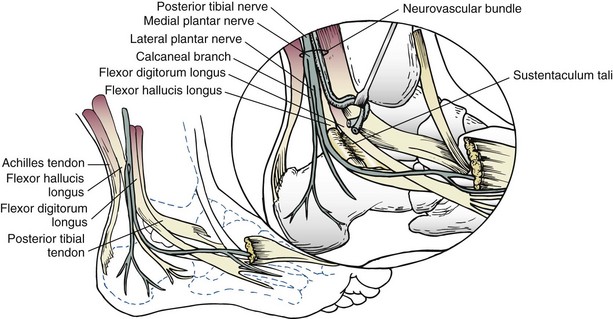
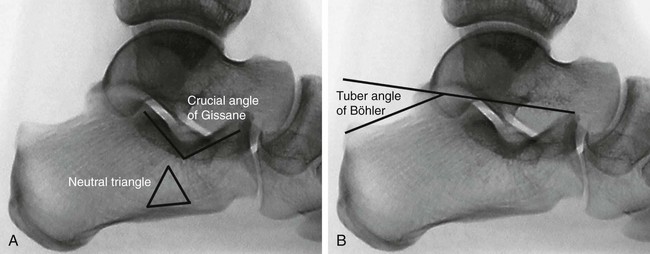
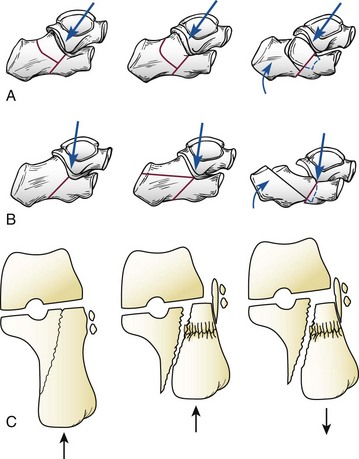
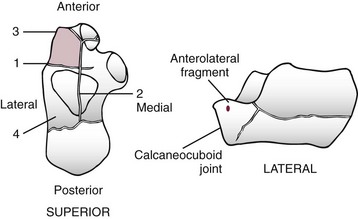
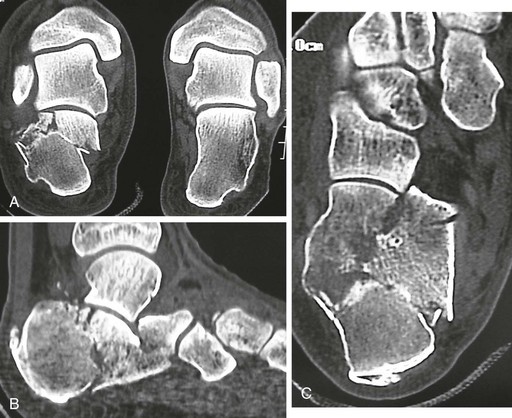
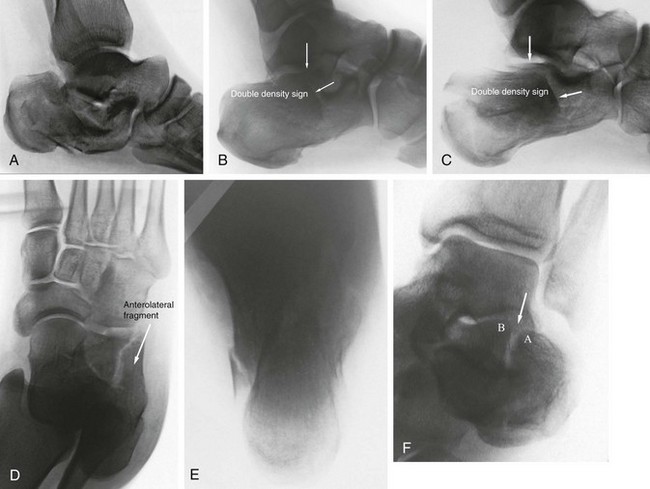
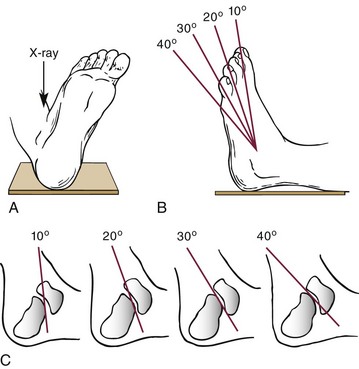
Chapter 38 Fractures of the calcaneus remain among the most challenging fractures for the orthopaedic surgeon to effectively manage. In 1720, Garangeot, Petit, Desault, and Bilgner published case reports on calcaneal fractures and advocated immobilization until solid union.177 Malgaigne, in 1843, first described calcaneal fractures in detail from cadaver specimens93,153; however, these fractures were not consistently diagnosed until the development of plain radiography in the late 1890s.22,48,123 The industrial revolution led to construction of taller buildings and the development of the automobile, so that falls from heights and motor vehicle accidents became increasingly more common263 and remain the most common causes of calcaneal fractures today. Calcaneal fractures are the most common of tarsal bone fractures and currently account for approximately 2% of all fractures.227 Displaced intraarticular fractures represent 60% to 75% of all calcaneal fractures.275 Ten percent of patients with calcaneal fractures have associated spine fractures, and 26% have other extremity injuries.147,194,206 Approximately 90% of calcaneal fractures occur in young men in their working prime, and the majority of these injuries occur in industrial workers.* Several reports have established that patients may be totally incapacitated for up to 3 years and at least partially impaired for up to 5 years after injury.74,147,182,266 Thus the economic implications of these fractures are indeed striking. Early reports on calcaneal fractures reflected the poor functional outcome historically associated with these injuries. Böhler, who provided an in-depth analysis of the pathoanatomic features of calcaneal fractures that is still relevant today, changed his treatment regimen no less than 12 times over a course of 30 years.22,23 Conn,46 in 1935, described calcaneal fractures as “serious and disabling injuries in which the end results are incredibly bad,” and McLaughlin158 compared attempts at maintenance of fracture reduction to “nailing a custard pie to the wall.” Although the development of modern surgical techniques and fixation implants has generally improved the functional outcome after these fractures, controversy continues to surround the management of these highly complex injuries.196 The calcaneus is the largest bone in the foot and plays an integral role in ankle and hindfoot function. Biomechanically, the calcaneus functions as a lever arm for the strong gastrocnemius–soleus complex while supporting the body weight and maintaining length of the lateral column to protect the posterior medial arch contents. The orientation of the calcaneus in the vertical plane has direct implications on the orientation of the talus, which indirectly affects dorsiflexion of the ankle joint. Structurally, the calcaneus has a unique shape and consists of six distinct surfaces.219 The superior surface includes a large extraarticular calcaneal body, the calcaneal tuberosity, which encompasses the posterior half of the bone. Three articular facets (anterior, medial, and posterior) articulate with the corresponding joint surface of the inferior talus and compose the anterior half of the superior surface (Fig. 38-1). The posterior facet is the largest of the facets and functions as the major weight-bearing surface, supporting the talar body. The orientation of the posterior facet includes a marked anterior downslope as well as a slight plantar slope medially. The middle facet sits atop the sustentaculum tali and is separated from the posterior facet by the obliquely oriented calcaneal sulcus, which forms the floor of the tarsal canal. The middle and anterior facets may be distinctly separate, partially conjoined, or fully conjoined into a single articular surface. The latter is the case in 20% to 64% of the population.219,278 The anterior surface features a unique saddle shape, which is convex transversely and concave vertically. It is covered almost entirely with articular cartilage. With the cuboid, it forms the calcaneocuboid joint. The joint is supported by the thick ligaments plantarly and the stout bifurcate ligament superiorly. The bifurcate ligament extends from the anterior process of the calcaneus to the cuboid and navicular. With the talonavicular joint, the calcaneocuboid joint forms the midtarsal (Chopart) joint that has a common axis through the bifurcate ligament. Isolated fractures at the anterior process of the calcaneus should raise the suspicion for a Chopart joint injury.196 The lateral surface includes the peroneal tubercle, an obliquely oriented bony prominence that anchors the inferior peroneal retinaculum. The peroneal tendons course along the lateral wall of the calcaneus, sitting in shallow grooves above (peroneus brevis) and below (peroneus longus) the peroneal tubercle. The origin of the calcaneofibular ligament is found posterior to the peroneal tubercle. The sural nerve lies posterior to the peroneal tendons and courses parallel to them before crossing them superficially at the level of the inferior peroneal retinaculum (Fig. 38-2). The medial surface is markedly stronger than the lateral wall. It includes the sustentaculum tali, which extends anterior medial and slightly superior to the calcaneal body and supports the neck of the talus. The sustentaculum is secured to the talus by the interosseous talocalcaneal ligament within the tarsal canal, the medial talocalcaneal ligament, and the deltoid ligament complex. The tibiocalcaneal portion of the superficial deltoid ligament typically provides stability to the sustentacular fragment in a displaced intraarticular calcaneal fracture. The flexor hallucis longus (FHL) tendon courses beneath the sustentaculum, and the flexor digitorum longus tendon runs directly over the sustentaculum. At this level, the medial plantar artery and nerve, terminal branches of the posterior tibial artery, and tibial nerve, respectively, lie between the abductor hallucis muscle and FHL tendon (Fig. 38-3). The heel pad consists of a highly specialized and condensed collection of adipose tissue, which is contained by fibrous septa. These septa are vertically arranged in spiral fashion to resist torsional forces applied at heel strike of gait. They form chambers that are supported by transversely oriented elastic tissue fibers.100,185,219 This unique arrangement is critical to shock absorption with normal gait. The lateral radiograph of the calcaneus demonstrates its unique topographic features. Compression trabeculae converge to provide support to the articular facets and merge with traction trabeculae radiating from the inferior cortex. This confluence of bony trabeculae forms a condensation of bone radiographically, which is known as the thalamic portion of the calcaneus, as described by Destot in 1911 and later by Soeur and Remy.63,231 The space between these trabeculae is referred to as the neutral triangle (Fig. 38-4A).63,103 The crucial angle of Gissane is formed by the subchondral bone of the posterior facet and middle and anterior facets. The overlying dense cortical bone forms two thick cortical struts, one extending from the lateral margin of the posterior facet and the other extending anteriorly to the calcaneal beak, which combine to form an obtuse angle of 120 to 145 degrees.74,91,219 These struts provide support to the lateral process of the talus, which sits directly above (see Fig. 38-4A). The tuber angle of Böhler23 is formed by the intersection of a line drawn from the highest point of the anterior process of the calcaneus to the highest point of the posterior facet and a line drawn tangent to the superior edge of the calcaneal tuberosity (Fig. 38-4B). The angle varies individually between 20 and 40 degrees.18,186 It is decreased in the event of a calcaneal fracture and may in fact be reversed in severe fractures. A decreased angle suggests collapse of the posterior facet, which shifts the body weight anteriorly; however, because reduction or reversal of the angle reflects only the proximal displacement of the tuberosity relative to the articular surface, the angle may be decreased in both intraarticular and extraarticular fractures.158 Thus the surgeon must bear this in mind in applying its absolute value in the evaluation and management of a calcaneal fracture.240 About 90% of the blood supply to the calcaneus is provided by the posterior tibial artery through medial and lateral calcaneal arteries, with the watershed area between them being in the midline of the calcaneal body. The remaining 10% of the calcaneal body receive vessels from the sinus tarsi artery. The medial and lateral calcaneal arteries form anastomoses with the malleolar network that receives input from the peroneal artery and the anterior tibial artery. The anterior process is supplied by the the dorsalis pedis and medial and lateral tarsal arteries.5 Displaced intraarticular fractures of the calcaneus generally occur in the event of high-energy trauma, such as a fall from a height, where the body weight of the patient is concentrated on the heel at the moment of impact, or a motor vehicle accident, in which case the affected foot is violently impacted by the floorboard or pedal of the car. The pattern of fracture lines and extent of comminution are somewhat variable and are determined by a variety of factors, including the position of the foot at impact, the extent of force involved at impact, and the patient’s overall bone quality. Although controversy remains as to the precise mechanism of injury, there is consensus to some degree among most authors.* Essex-Lopresti74 proposed that the primary fracture line was initiated laterally, with subsequent extension medially. He believed that at the moment of impact, the subtalar joint was forced into eversion such that the lateral process of the talus impacted the calcaneus at the crucial angle of Gissane, dividing the lateral wall and body of the calcaneus. The residual force then dissipated medially into the sustentaculum. With continuation of force, the fracture line extended into the anterior process or calcaneocuboid joint, thus producing an anterolateral fragment. A secondary fracture line then resulted from increased force: With a posteriorly directed force, the fracture line continued into and posterior to the posterior facet, producing a joint-depression fracture; with a more inferiorly directed force, the fracture line extended inferior to the posterior facet, producing a tongue-type fracture (Fig. 38-5). Carr et al37 created intraarticular calcaneal fractures experimentally using cadaveric models and analyzed the resulting pathoanatomy. Two primary fracture lines were consistently identified: One sagittal fracture line sectioned the calcaneus into medial and lateral fragments, whereby the fracture extended anteriorly into either the anterior facet or the calcaneocuboid joint; the coronal primary fracture line sectioned the calcaneus into anterior and posterior fragments, starting laterally at the crucial angle of Gissane and continuing medially, often dividing the middle facet. Laterally, this second primary fracture line often continued either inferiorly or anteriorly, exiting the plantar surface. These primary fracture lines produced a variety of fracture patterns, including joint depression and tongue-type fractures, as well as the commonly observed anterolateral, superolateral, and superomedial fracture fragments, thereby confirming the findings of Essex-Lopresti and others (Fig. 38-6).74,231,277 Because the axis of the calcaneus lies laterally to that of the talus, the tuberosity fragment is sheared off obliquely in a superolateral direction with respect to the fixed sutentacular fragment (see Fig. 38-5C).181 The position of the hindfoot at the time of impact has a direct influence on the fracture pattern.250 With the hindfoot in pronation (valgus), the sagittal primary fracture line runs laterally, creating a large superomedial fragment; with the hindfoot in inversion (varus), the fracture line lies more medially.270 These biomechanical findings may explain the morphology of two-part fracture-dislocations and isolated fractures of the sustentaculum, respectively, and have been confirmed in computed tomography (CT) analyses.168,277 With displaced intraarticular calcaneal fractures, clarification of fragment terminology is necessary to understand the pathoanatomy of these fractures. The anterior main fragment is the large fragment anterior to the primary fracture line, which typically includes the anterior portion of the sustentaculum and anterior process. The anterolateral fragment refers to the lateral wall of the anterior process; this fragment is typically pyramid shaped and can include a portion of the calcaneocuboid articular surface. The anteromedial fragment is usually smaller and contains the anterior facet and the medial portion of the calcaneocuboid articular surface.277 The superomedial fragment is the fragment of variable size found posterior to the primary fracture line; this fragment is also known as the sustentacular or constant fragment because the fragment almost always remains attached to the talus through the deltoid ligament complex and is therefore stable. The superolateral fragment, also referred to as the semilunar or comet fragment, is the lateral portion of the posterior facet that is sheared from the remaining posterior facet in joint depression fractures. The tongue fragment refers to the superolateral fragment that remains attached to a portion of the posterior tuberosity, including the Achilles tendon insertion, and is found in tongue-type fractures. The posterior main fragment represents the posterior tuberosity. In the event of a displaced intraarticular calcaneal fracture, the loss of height through the calcaneus results in a shortened and widened heel, typically with varus malalignment of the tuberosity. This loss of height is reflected in a decreased tuber angle of Böhler such that the normal declination of the talus is diminished, and the talus becomes relatively more horizontal, which leads to secondary loss of ankle dorsiflexion. As the superolateral fragment of the posterior facet is impacted plantarward, the thin lateral wall explodes laterally just posterior to the crucial angle of Gissane. This lateral wall expansion can trap the peroneal tendons against the lateral malleolus and can also affect subtalar motion. In some cases, a violent contracture of the peroneal tendons avulses the tendon sheath from the fibula, resulting in an avulsion fracture of the lateral malleolus and dislocation of the peroneal tendons. The anterior process typically displaces superiorly, which directly limits subtalar joint motion by impinging against the lateral process of the talus (Fig. 38-7) and directly affecting congruity of the calcaneocuboid joint. Four main compartments exist within the foot: medial, lateral, central, and interosseous. The central compartment is further divided by a transverse septum into the superficial compartment, which contains the flexor digitorum brevis muscle, and the deep or calcaneal compartment, which contains the quadratus plantae muscle and lateral plantar nerve and communicates directly with the deep posterior compartment of the lower leg.75,155 The long-term sequelae of an unrecognized compartment syndrome in the foot include claw toe deformities with contracture, weakness, sensory disturbances, painful callus formation, and permanent loss of function. Hence care should be taken to ensure that the extreme pain associated with the fracture is not in fact due to a compartment syndrome, especially in the deep central (calcaneal) compartment. A self-contained needle manometer system (Quikstik; Stryker, Kalamazoo, Mich.) can be used to measure compartment pressures and assist in establishing the diagnosis, especially in unconscious patients. Fasciotomy is generally recommended when compartment pressures are within 10 to 30 mm Hg of the patient’s diastolic blood pressure.75,172,173 Fracture blisters can arise anywhere about the foot in the event of severe swelling.88–90,259 A blister occurs as a result of cleavage at the dermal–epidermal junction, which produces a sterile transudate within the blister. The fluid remains clear if the dermis retains some epidermal cells, but it can become bloody if the dermis is fully devoid of epidermal cells.88 A variety of treatment methods have been described in the management of fracture blisters, including aspirating the blister, unroofing the blister and applying silver sulfadiazine (Silvadene) cream or nonadherent dressing, and leaving the blister intact and covered with loose gauze or exposed to air. Although there is no consensus as to the optimal management of fracture blisters, most authors recommend modification of surgical incisions to avoid areas of blistered skin, particularly blood-filled blisters (Fig. 38-8).88–90,259 Open fractures of the calcaneus comprise up to 17% of all calcaneal fractures and represent distinct injuries requiring different treatment from closed fractures.14,16,49,96 Open injuries are associated with increased treatment costs and time off work.52 They are generally associated with a higher complication rate, including wound complications, deep infection, osteomyelitis, and subsequent need for amputation,* and the incidence of these complications appears to increase with increasing severity of the soft tissue injury. Folk et al79 reported wound complications in 72% of open calcaneal fractures treated operatively in their series, and they estimated that patients with an open fracture were 2.8 times more likely to develop a wound complication than patients with a closed fracture. In other studies, the risk of wound complications and infections were increased up to fivefold compared with closed fractures.4,107,194,234 Siebert et al225 reported a 60% incidence of osteomyelitis in type III open fractures treated with internal fixation. Other more recent reports have emphasized the importance of aggressive, thorough surgical debridement of the open wound, provisional stabilization of the involved limb where necessary, and delayed open reduction and internal fixation (ORIF) of the fracture once the wound is clean and deemed suitable for surgery.4,14,16,107,137 Despite these measures, significant wound complications, deep infection, and osteomyelitis can still develop in up to 19% of cases.4,14,107,267 Even in the absence of these complications, most patients can expect a functional outcome far worse than with closed fractures, particularly for patients with a plantar wound.16 Heier et al107 concluded that the degree of soft tissue injury was the most important factor in predicting outcome. Open fractures of the calcaneus vary from a simple puncture wound medially, such as from a spike of bone from the medial wall of the calcaneus, to a more significant wound with marked soft tissue disruption posteriorly or laterally (Fig. 38-9). In severe cases, the injury can include dislocation of the talonavicular joint, whereby the talar head is driven through the anterior calcaneus and might even exit through the plantar skin.201 In evaluating an open calcaneal fracture, the wound size and location should be assessed, and the injury should be classified using the system of Gustilo and Anderson.96,97 In an analysis of 127 open calcaneal fractures, Wiersema et al266 found medial-based wounds in 54.8% of cases, 64 fractures were graded Gustilo types I or II, and 51 fractures were graded Gustilo type III, among them 5 type IIIC. These factors provide the surgeon perspective for the severity of the injury and thus a realistic prognosis for the patient.4,14,16,107,137 As with all open fractures, initial management includes intravenous antibiotics, thorough surgical debridement and pulsed lavage irrigation of the wound, and provisional stabilization of the limb. Closed reduction and temporary percutaneous fixation may be used where necessary, either with Kirschner wires (K-wires) or with an external fixator construct. Further treatment is dictated by the extent and location of the soft tissue injury, and each open injury should be individualized in formulating a treatment plan. Early, aggressive fracture stabilization should, however, be avoided so as to prevent further trauma to the limb.201 Definitive surgical treatment may need to be delayed for up to 3 months to allow adequate soft tissue healing, in which case the injury is managed as calcaneal malunion. On the other hand, early and stable soft tissue coverage using free microvascular flaps in combination with fracture fixation may reduce the rate of severe complications and improve functional outcome by avoiding excessive scarring in complex injuries.28 This approach requires close collaboration with plastic surgeons from the first day of presentation. Heier et al107 recommended that all open type I fractures and open type II fractures with a medial wound be treated by ORIF with standard techniques once the soft tissue swelling has adequately diminished. External fixation or limited percutaneous fixation is used for open type II injuries with nonmedial wounds and all open type IIIA wounds. Delayed or late reconstruction is reserved for all open type IIIB wounds and for injuries resulting from penetrating trauma. Recently, Mehta et al161 saw only one low superficial and one deep infection (7.1%) in a series of 14 type II or IIIA medially open calcaneal fractures with a staged protocol of debridement, irrigation and percutaneous fixation within 8 hours, and definite lateral plate fixation via an extensile laterally based approach within 18 days. For select open fractures with a medial wound and limited articular damage even acute fixation via a lateral approach appears feasible.150 Associated injuries, including lumbar spine fractures or other lower extremity fractures, have historically occurred in up to 50% of patients with calcaneal fractures.40,74,278 More recent estimates suggest that up to 10% of patients with calcaneal fractures have lumbar spine fractures, and approximately 25% have other associated lower extremity injuries.152,196,241,256 These associated injuries are more common with higher-energy calcaneal fractures, and the surgeon must maintain a high index of suspicion. Thorough radiographic evaluation should be performed where indicated.108 In multiply injured or polytraumatized patients, closed calcaneal fractures might go unnoticed because of more obvious or even life-threatening injuries. However, if the patients survive the critical period, foot injuries make up for most of the permanent diability.196,241,256 The initial radiographic evaluation of a patient with a suspected calcaneal fracture includes plain radiographs of the involved foot and ankle, including a lateral view of the hindfoot, an anteroposterior (AP) view of the foot, an axial view of the heel,120 and a mortise view of the ankle. This combination should reveal almost any fracture, dislocation, or subluxation in the hindfoot. Plain radiographs of the lumbar spine are also routinely obtained in light of the association between lumbar spine injuries and calcaneal fractures, particularly those involving a fall from a height. Typically, the lateral view of the hindfoot most readily demonstrates a fracture of the calcaneus, and with an intraarticular fracture, the lateral view shows whether the fracture is a joint depression or tongue-type fracture according to the classification of Essex-Lopresti.74 A loss of height in the posterior facet is another feature of these fractures: the articular surface is impacted within the body of the calcaneus and usually rotated anteriorly up to 90 degrees relative to the remaining subtalar joint. A decreased tuber angle of Böhler and an increased crucial angle of Gissane are seen in fracture patterns where the entire posterior facet is separated from the sustentaculum and depressed (Fig. 38-10A). If only the lateral portion of the posterior facet is involved, the split in the articular surface is manifest as a double density,212 in which case the tuber angle of Böhler and crucial angle of Gissane can remain normal (Fig. 38-10B and C). If a calcaneal fracture is obvious in the lateral view, no further plain radiographs are needed, and CT scanning should be done to reveal the exact size and location of the main fragments as well as joint involvement. The AP view of the foot usually reveals extension of fracture lines into the calcaneocuboid joint, and it can also demonstrate anterolateral fragments and expansion of the lateral calcaneal wall. This view otherwise offers only limited information and can be omitted in most cases (Fig. 38-10D). The non–weight-bearing axial view of the heel shows a loss of calcaneal height, increased width and (typically) varus angulation of the tuberosity fragment, and visualization of the articular surface. Because of the pain of acute fractures, a weight-bearing (Harris) axial view is difficult to obtain (Fig. 38-10E). A mortise view of the ankle usually demonstrates involvement of the posterior facet, broadening of the lateral wall, and abutment of the lateral malleolus with fracture-dislocations (Fig. 38-10F). A specialized view of the ankle, known as a Brodén view or Brodén projection I, more effectively reveals the posterior facet articular surface.7,29 The view is obtained with the patient supine and the x-ray cassette under the ankle, the foot positioned in neutral flexion, and the leg internally rotated 30 to 40 degrees. The x-ray beam is centered over the lateral malleolus, and four views are obtained with the tube angled at 10, 20, 30, and 40 degrees, respectively, toward the head of the patient. These views then demonstrate the posterior facet, working from posterior to anterior: the 10-degree view shows the posterior portion of the facet, and the 40-degree view shows the anterior portion (Fig. 38-11). Although these images can be difficult to reproduce in an emergency room or office setting, this view should be used intraoperatively because it is invaluable in verifying reduction of the posterior facet articular surface.133
Fractures of the Calcaneus
Anatomy
Intraarticular Fractures
Mechanism of Injury
Clinical Evaluation
Compartment Syndrome
Skin Blisters
Open Fractures
Associated Injuries
Radiologic Evaluation
Plain Radiography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fractures of the Calcaneus