CHAPTER 15 Fractures, Dislocations, and Acquired Problems of the Shoulder in Children
FRACTURES OF THE PROXIMAL HUMERUS
Anatomy
Embryology and Development
The formation of the humerus begins with the appearance of the cartilage anlage, which is present by the fifth week. The primary ossification center for the humerus appears at about the sixth week.1 By birth the entire humeral shaft is completely ossified.
The proximal humerus is primarily cartilaginous at birth; however, the ossification centers can be detected through ultrasonography as early as the 38th week of gestation and are generally present between the 38th and 42nd week of gestation.2,3
The three proximal humeral ossification centers consist of the greater and lesser tuberosities and the humeral head. The ossification center for the humeral head is usually present at birth; the one for the greater tuberosity appears by 1 to 3 years of age, and the lesser tuberosity ossification center appears by 5 years of age.4–6 These ossification centers fuse by 5 to 7 years of age to form the head of the humerus. The proximal humeral ossification center fuses with the humeral shaft by 14 to 17 years of age in girls and 16 to 18 years in boys.4,7–9
Humeral retroversion likewise gradually develops over time. The normal adult value for humeral retroversion is highly variable based on anatomic and imaging studies.10–16 Humeral retroversion averages 65 degrees in infants and young children and gradually decreases, approaching adult values by 11 years of age.17
At birth, the body or shaft of the humerus is completely ossified.4 The proximal and distal ends allow longitudinal growth of the humerus. Eighty percent of humeral growth is secondary to the proximal humeral physis, accounting for approximately 40% of growth of the entire upper extremity.9,18 Growth derived from the proximal humerus likewise varies with age: less than 75% of growth occurs before 2 years of age and more than 85% occurs by age 8 years.7–9 This growth continues until physeal closure, which occurs at 14 years of age in girls and 17 years of age in boys.
Surgical Anatomy
The capsule of the glenohumeral joint extends from the glenoid rim, progressing laterally toward the surgical neck of the humerus and blending with the tendons of the rotator cuff musculature, where it surrounds the articular surface of the proximal humerus. The posterior medial metaphysis, a portion of the physis, and the epiphysis are intracapsular. A large portion of the physis is extracapsular, making it susceptible to injury. The proximal humeral physis is irregularly shaped, with its apex located on the posteromedial portion of the proximal humerus. The periosteum is also thicker in the posteromedial portion of the proximal humerus as opposed to the anterolateral portion, which is quite thin.19 The posteromedial periosteum is stronger compared to the anterolateral periosteum; hence, the tendency for the fracture to penetrate the periosteum anterolaterally.
The proximal humerus is also the insertion site for numerous muscles around the shoulder girdle; this anatomic fact greatly influences the fracture configuration due to the forces exerted on the humerus both proximally and distally. The muscles of the rotator cuff, which act as stabilizers of the shoulder, run transverse, anterior, superior, and posterior to the glenohumeral joint.20–23 The subscapularis, which originates from the undersurface of the scapula, inserts into the lesser tuberosity. The greater tuberosity provides attachment superiorly and posteriorly for the supraspinatus, the infraspinatus, and teres minor, all of which originate from the posterior portion of the scapula. The deltoids, which act as flexors and abductors, run from the clavicle and acromion inserting into the lateral portion of the upper third of the humeral shaft. Other muscles of importance include the pectoralis major, which inserts into the lateral lip of the bicipital groove.
Important neurovascular structures also course through the glenohumeral joint and the proximal humerus. The proximal humerus receives its blood supply from the axillary artery. The anterior and posterior humeral circumflex arteries supply the proximal humerus. The arcuate artery, which ascends from the anterior humeral circumflex artery, supplies the humeral head.24–27 The subscapular artery also branches from the axillary artery, which supplies the rotator cuff muscles. Close proximity of the proximal humerus to the brachial plexus makes the brachial plexus prone to injury when the proximal humerus is injured in dislocations or fractures. The axillary nerve in particular passes inferior to the glenohumeral joint and posterior to the proximal humerus.28–31
Incidence
Fractures of the proximal humerus have been reported to be about 5% of all children’s fractures.32–36 The incidence of fractures of the proximal humerus show a linear increase with age, with Salter–Harris type I fractures predominating in younger children, metaphyseal fractures more common in children 5 to 11 years, and Salter–Harris type II fractures in children older than 11 years. Fractures of the proximal humeral epiphysis represent 2% to 7% of all growth plate injuries in children.37–39
Mechanism of Injury
Shoulder dystocia is an infrequent cause of birth injuries in children. Shoulder dystocia is usually associated with conditions such as maternal diabetes, macrosomia, post-term pregnancy, and a previous history of shoulder dystocia. Gherman and colleagues reported on the incidence of birth injuries and found the incidence of birth injuries associated with shoulder dystocia to be 24.9%, with a 4.2% incidence of proximal humeral fractures.40 The mechanism of injury is also related to arm position during delivery. Abnormal positions implicated in birth fractures, such as separation of the proximal humeral physis, include hyperextension and external rotation of the humerus.41–44
In the older child, both direct and indirect trauma to the proximal humerus has been implicated. Injuries from sports, vehicular or traffic accidents, and falls are the most common cause of proximal humerus fractures in children.45 Six mechanisms of injury have been reported by Williams: forced extension, forced flexion, flexion with lateral rotation or with medial rotation, and forced extension with lateral rotation or with medial rotation.46
Repetitive injury can also cause damage to the proximal humeral physis (Fig. 15-1). Slipping of the proximal humeral growth plate has been reported to occur in gymnasts.47 Stress-related injuries have likewise been reported secondary to gymnastics, baseball pitching, and various sporting activities, causing stress secondary to upper extremity loading.48–55
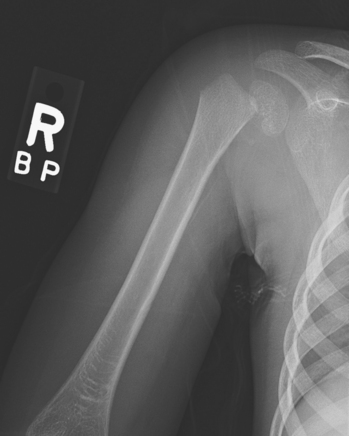
Pathologic fractures occurring through benign lesions have been reported infrequently (Fig. 15-2), particularly common benign lesions causing pathologic fractures through the proximal humerus, including aneurysmal and unicameral bone cysts.56–59 Malignant lesions have been reported to cause pathologic fractures through the proximal humerus.59–62
Metabolic conditions such as pituitary gigantism can cause weakening of the growth plate, leading to development of deformity.63 Underlying neuromuscular conditions such as Arnold–Chiari malformation, syringomyelia, myelomeningocele, and cerebral palsy have been identified as risk factors or etiologic agents in the development of growth plate injuries and fractures about the proximal humerus.64–67
Nonaccidental injury should also be considered when children present with the proximal humerus fracture, particularly if the underlying cause is unclear and multiple injuries are noted.68–72
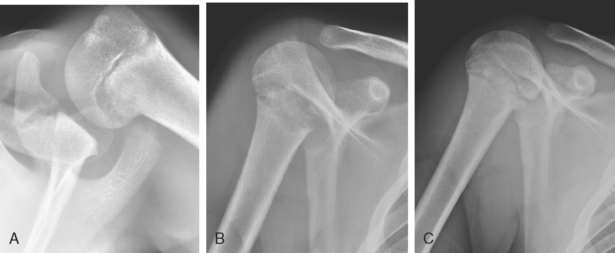
Classification
Fractures of the proximal humerus in children may be classified according to the location of the injury. Growth plate injuries in children are classified according to the Salter–Harris classification.18 In younger children (<5 years), Salter–Harris type I injuries predominate (Fig. 15-3). In children older than 11 years, Salter–Harris type II fracture patterns predominate (Fig. 15-4).39 The other three types Salter–Harris—types III, IV, and V—are very rare, particularly in the proximal humerus. However, cases of Salter–Harris type III injuries have been reported in the literature.73
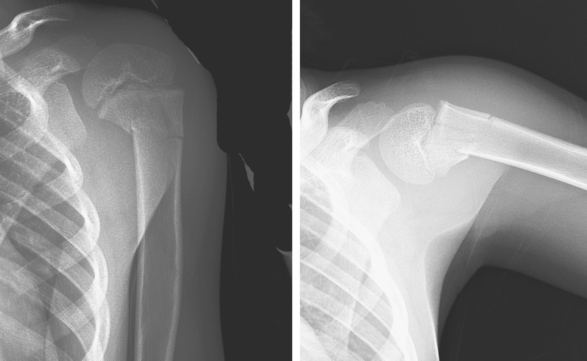
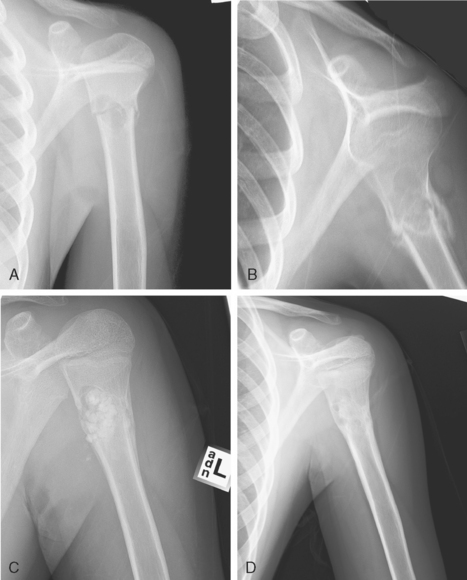
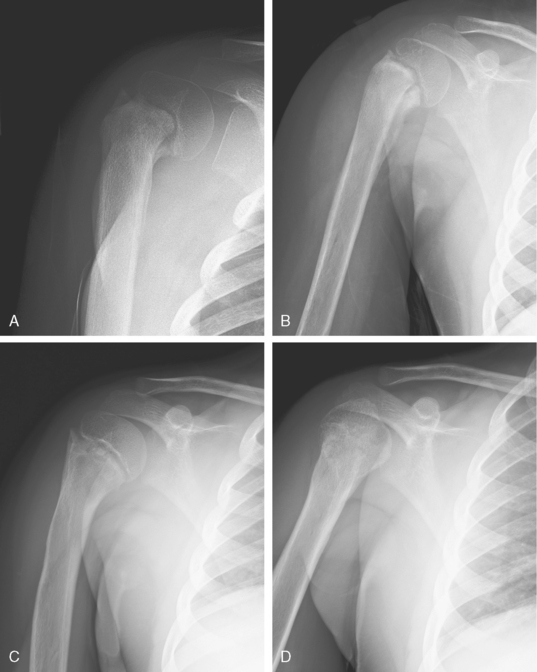
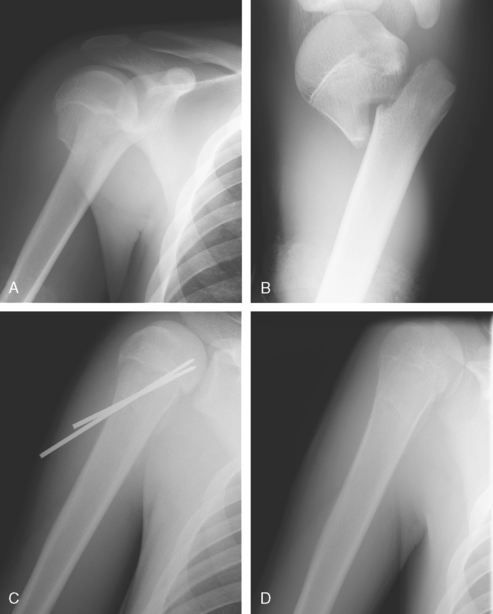
FIGURE 15-4 Radiographs of an 8 year old who sustained a Salter–Harris type II growth plate injury secondary to a fall.
The location of the fracture may also be used to define the fracture. This is a broad categorization, dividing the fractures according to area of involvement, such as the proximal humeral metaphysis (Fig. 15-5), growth plate, and lesser and greater tuberosities. Fractures can also be classified based on the degree of deformity as well as the degree of displacement. Neer and Horwitz classified proximal humeral fractures according to degree of displacement.74 They divided the fractures into four types based on degree of displacement:
Open fractures of the proximal humerus, although uncommon, also occur and can be classified using the Gustilo–Anderson classification for open fractures.75,76
Signs and Symptoms
In the older child, a history consistent with a traumatic event can usually be elicited. The most common presentation is limited ROM of the shoulder, with abnormal fullness or deformity of the affected shoulder as compared to the contralateral extremity. Depending on the degree of trauma, other signs of injury are likewise present, including soft tissue injuries, ecchymosis, and swelling. The affected extremity is usually carried in an internally rotated posture. In posterior fracture-dislocations there is painful limited external rotation of the shoulder. In lesser tuberosity fractures there is limited abduction and external rotation of the shoulder.77–79 Greater tuberosity fractures manifest with luxatio erecta.80–82 The shoulder is in abduction with the elbow flexed and the hand above the head.
Radiographic Evaluation
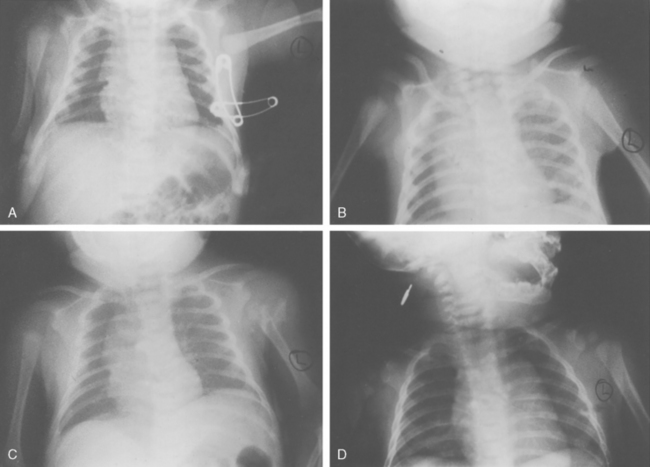
Imaging of the proximal humerus can be challenging in neonates and infants because the proximal humerus is primarily cartilaginous. Generally, in neonates and infants with a suspected fracture of the proximal humerus or proximal humeral growth plate, a single anteroposterior (AP) view of the chest and upper extremities may be used to screen for injuries. On plain radiographs, the relationship of the proximal humeral metaphysis, scapula, and acromion are evaluated. These structures are compared with the contralateral side (Fig. 15-6). The abnormal relationship of the scapula and humerus has been described to denote a proximal humeral physeal injury with a posteriorly displaced proximal humeral fragment. This has been termed the vanishing epiphysis sign.44,83 Ultrasound examination may be a valuable imaging tool.84–88 Ultrasonography is quick and noninvasive, and the injury may be directly visualized, with the contralateral side serving as a comparison. Arthrography can also be valuable.89,90 Computed tomography (CT) may also be useful in evaluating the shoulder injuries missed at birth, particularly those with posterior dislocation.91
Plain radiographs are still the mainstay in the initial evaluation of shoulder injuries in older children. Well-performed radiographs obtained in orthogonal views should be adequate in providing information on the pathology. A true AP and lateral view of the shoulder are usually sufficient for assessing the injury. A true AP image of the shoulder is taken in the scapular plane with the beam parallel to the glenohumeral joint. The axillary lateral view is preferred, although it may be difficult to obtain in the setting of an acutely injured child. In lieu of the axillary lateral view, alternative views such as the transthoracic axillary view or the scapular Y view may be obtained. The apical oblique view is also valuable in some cases.
Treatment
The treatment of fractures of the proximal humerus generally depends on the age of the patient and on the fracture type and location. In general, the prognosis for most proximal humerus fractures in children is good, with the vast majority amenable to nonoperative management. Because the proximal humeral physis contributes the most growth of the upper extremity and closes late, there is tremendous remodeling potential for the proximal humerus (Fig. 15-7). The location of the fracture likewise exerts a great influence on the management, whether the fracture involves the growth plate or extends through the metaphysis.
In neonates with birth injuries, the prognosis is generally good; only the most severely displaced fractures require any attempt at reduction. If reduction is performed, gentle maneuvers without anesthesia generally work well. These maneuvers may be monitored using ultrasonography. In the vast majority of cases, the shoulder can be immobilized efficiently by pinning the shirt sleeve or soft dressing to the shirt. These fractures heal very quickly, usually within 2 to 3 weeks.19,43
In general, fracture treatment is determined by the degree of displacement and the amount of remodeling potential. Beaty recommended treatment guidelines based on the patient’s age (Table 15-1).92 In young children, excellent outcomes have been reported with nonoperative management.19,74,93 In older children, nonoperative management has been reported to have good results, particularly in Neer type 1 and type 2 cases. Reduction, however, was required more often in Neer type 3 and 4 fractures.19,74,93,94
TABLE 15-1 Guidelines for Reduction
| Age | Acceptable Angulation | Acceptable Displacement |
|---|---|---|
| <5yr | 70 degrees | 100% |
| 5-12yr | 40-70 degrees | — |
| >12yr | 40 degrees | 50% |
Based on Beaty JH: Fractures of the proximal humerus and shaft in children. Instr Course Lect 41:369-372, 1992.
Reduction
In general, reduction is reserved for severely displaced or angulated fractures in older children. Potential barriers to reduction include periosteum, capsule, and biceps tendon.92,95–97 Numerous reduction maneuvers have been recommended. Most fractures can be treated with gentle traction coupled with abduction, external rotation, and flexion of the shoulder. Neer and Horwitz recommended reduction with 90 degrees of forward flexion, abduction, and external rotation.74 Others recommend reduction with 135 degrees of abduction and 30 degrees of flexion and external rotation; the fracture is manipulated directly to obtain reduction.98,99
Once acceptable or adequate reduction is obtained, any of several immobilization techniques may be used. Immobilization methods described in the literature include sling and swathe (Fig. 15-8), two-prong splint, thoracobrachial bandage, shoulder spica cast, Statue of Liberty cast, and hanging arm cast.19,74,93,100,101 It is important for the surgeon and family to understand that very displaced proximal humerus fractures in older children are generally quite unstable. Some loss of reduction is common if internal fixation is not used.
Operative Treatment
There are numerous options for internal fixation of proximal humerus fractures. Displaced fractures may be treated with closed reduction and percutaneous techniques or open reduction and internal fixation.102–104
Percutaneous pin fixation may be performed once adequate reduction has been obtained (Fig. 15-9).105,106 Percutaneous pinning can be done under image intensification. The patient is placed supine on the operating table. A closed reduction is performed under image intensification. Once adequate reduction has been obtained, the pins are inserted laterally through the metaphysis, in an inferior-to-superior fashion. The surgeon should be careful to avoid the axillary nerve laterally and anteriorly, as well as the other neurovascular structures more medially. The pinning technique can be challenging because the optimal trajectory is quite steep and the cortex of the proximal humerus can be very hard. Smooth pins can be used, or the small external fix-it or pins with threaded tips can be used instead, if there are concerns about pin migration.
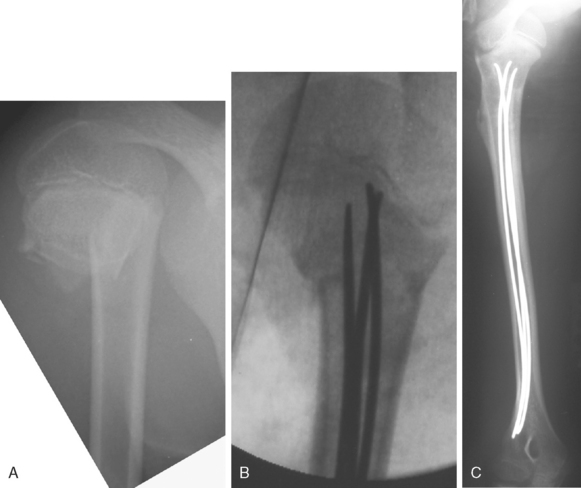
Flexible intramedullary nails have also been used to manage proximal humerus fractures in children (Fig. 15-10).107
Treatments for Specific Fracture Patterns
The lesser tuberosity is the site of the insertion of the subscapularis. Good results have been reported with nonoperative management of lesser tuberosity fractures.77,79,108 However, several authors advocate open reduction and internal fixation in acute fractures.78,109,110 Ogawa and Takahashi reported better results with operative management of lesser tuberosity fractures.111 Options for fracture fixation depend on the size of the avulsed fragment. In most cases suture fixation is adequate. Screw fixation may be performed in fractures with larger fragments. Good results have been reported after arthroscopic treatment.112
Fracture-dislocations of the proximal humerus are not very common injuries. Proper treatment of the injury consists of stabilizing the fracture and reducing the glenohumeral joint.113,114
Authors’ Preferred Treatment
Nonoperative
Most proximal humerus fractures, including physeal fractures, can be managed nonoperatively. Our preferred method for treatment depends on the age of the patient. In the neonate and infant, we manage most fractures with simple immobilization often by safety-pinning the shirtsleeve to the front of the shirt. In the older child with a proximal humerus fracture, we follow the displacement guidelines of Beaty (see Table 15-1). Most fractures can be treated with immobilization alone. We usually start with a coaptation splint and an elastic (Ace) wrap, then, at 10 to 14 days after injury, change to a shoulder immobilizer or hanging cast once the child is more comfortable (see Fig. 15-8).
Operative
Once adequate reduction is achieved, percutaneous pins are inserted through the lateral cortex. We prefer the small external fixator or pins with a threaded tip to minimize the risk of migration. These pins are directed across the fracture site and into the head of the humerus, stopping short of the subchondral bone. Two or three pins are inserted until the fracture has been satisfactorily stabilized (Fig. 15-11). In older children (perhaps 13 years old and older), it is best to cut the pins and bury them beneath the skin, because fracture healing can take 4 to 6 weeks. The pins are cut to appropriate length. The extremity is placed in a shoulder immobilizer for 2 to 3 weeks.
Complications
Proximal humerus fracture complications may be divided into early and late. Early complications result directly from the fracture. These complications can be serious and develop into potentially limb-threatening injuries. Neurologic injuries have been reported to occur with proximal humerus fractures.115–118 Typically, these are injuries to the brachial plexus from fracture dislocation. They can often be diagnosed early after injury, with loss of strength and sensation in the nerve distribution. Most of these injuries are neurapraxias that recover within 4 to 6 months. If no sign of recovery is noted, an EMG study is warranted to document whether there is actual improvement in the status of the nerve palsy. No improvement at this time is an indication for surgical exploration and possible repair or nerve grafting of the involved structure.115
Vascular injuries are uncommon but have been reported.119–121 Implant-related complications such as hardware migration have also been reported after internal fixation of proximal humerus fractures.107,122–124 Loss of motion is also another complication that is seen, particularly in patients who were treated surgically.
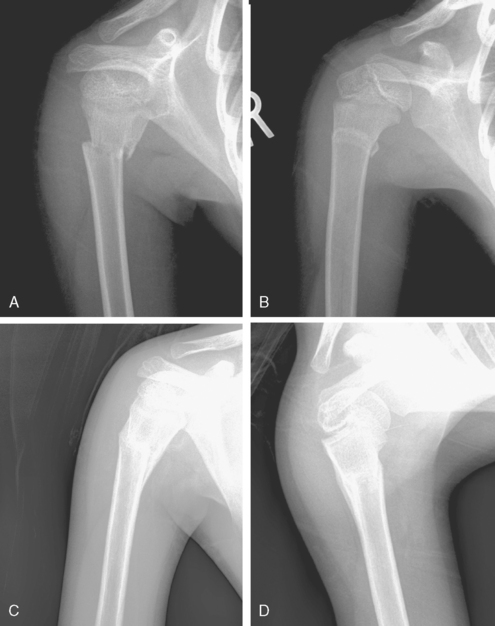
Late complications are often sequelae of the original injury. Humerus varus usually occurs in children and neonates after a history of trauma, infection, or metabolic or hematologic conditions (Fig. 15-12).125–130 This usually results in a decrease in the humeral neck-shaft angle accompanied by shortening of the humerus. The deformity results in slight limitation of ROM and often does not require surgical intervention. However, in some cases surgical management is needed to properly realign the humerus.121,127,130–132
FIGURE 15-12 Proximal humeral varus resulting from an infection at 11.5 years of age. A, Marked shortening (arrow). B, Varus.
(From Rockwood CA, Wilkins KE, Beaty J [eds]: Fractures in Children. Philadelphia: JB Lippincott, 1996.)
Growth arrest has been reported in children who have growth plate fractures and in some pathologic conditions that cross the physis, such as chondroblastomas and bone cysts.45,133–139 Complete physeal arrest has been reported but is relatively rare. More often these cases do not produce any functional deficit, and most children do not need any form of surgical intervention.
Hypertrophic scar formation is a complication seen after surgical management.19,140,141 To avoid this, some authors have reported a more cosmetic axillary approach for treatment of these injuries.142 Osteonecrosis of the humeral head is a rare complication; however, even with osteonecrosis, good outcomes have been reported.143 Glenohumeral subluxation has also been reported in children with proximal humerus fractures.73,114 These often respond well to a period of nonoperative management, which includes supporting the extremity in a sling and instituting early rehabilitation.
FRACTURES OF THE CLAVICLE
Anatomy
Embryology and Development
The clavicle is one of the first bones to ossify. The clavicle begins ossification from two primary ossification centers (medial and lateral) by 5 to 6 weeks of gestation. By 7 to 8 weeks of gestation, the clavicle already has assumed its overall contour and typical S shape. Most growth (80%) occurs from the medial physis. Despite its early appearance, the clavicle is one of the last bones to complete ossification. The lateral epiphysis forms and fuses in a remarkably short time around 18 to 19 years of age. The medial epiphysis is the last in the body to ossify, at age 18 to 20 years, and the last to complete ossification, at age 23 to 25 years of age.144,145
Relevant Anatomy
The clavicle is an S-shaped bone that articulates medially with the sternum and laterally with the scapula at the acromion process. Through the sternoclavicular and acromioclavicular joints, the clavicle functionally links the axial skeleton and upper extremity. The medial two thirds of the bone is round and tubular; the lateral third is flat. The anterosuperior aspect of the clavicle is subcutaneous. The subclavian vessels and brachial plexus lie posterior to the clavicle near the junction of the medial two thirds and lateral one third (Fig. 15-13).
FIGURE 15-13 Relationship of the clavicle and scapula to the brachial plexus and subclavian artery.
(From Sarwark JF, King EC, Luhmann SJ: Proximal humerus, scapula, and clavicle. In Beaty JH, Kasser JR [eds]: Fractures in Children, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006, pp 703-771.)
Numerous muscles and ligaments attach to the clavicle. Anteriorly, the pectoralis major originates on the medial two thirds of the clavicle and the deltoid on the lateral third. Posteriorly, the trapezius muscle inserts on to the lateral third of the clavicle. The clavicular head of the sternocleidomastoid muscle originates on the superior surface. The subclavius muscle and enveloping clavipectoral fascia attach to the inferior surface.
By providing these muscular and ligamentous attachment sites, in particular to the principal mobilizers of the upper arm, the pectoralis major and deltoid muscles, the clavicle plays a significant part in overall motion and function of the upper extremity. In addition, through the sternoclavicular joint, the clavicle itself is responsible for limited motion.146–148 Upward elevation of the clavicle approximately 30 to 35 degrees contributes to shoulder abduction. The clavicle can also protract and retract approximately 35 degrees in the anterior-to-posterior plane. Lastly, the clavicle can rotate 45 to 50 degrees about the long axis of the clavicle.
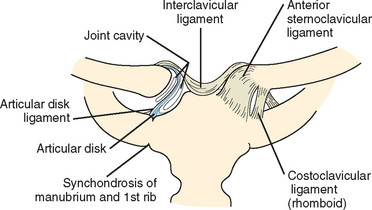
Medially, the clavicle articulates with the manubrium of the sternum and the first rib through the sternoclavicular joint. The sternoclavicular joint is also diarthrodial, and similar to the acromioclavicular joint, it lacks inherent structural stability. The joint is stabilized by a group of ligaments, including the intra-articular disk ligament, the anterior and posterior capsular ligaments, the interclavicular ligament, and the costoclavicular ligament (Fig. 15-14). The anterior portion of the capsular ligament is heavier and stronger than the posterior portion.149 The capsular ligaments attach mainly to the epiphysis of the medial clavicle; therefore, the physis is extra-articular and susceptible during injuries to the medial clavicle. The sternoclavicular joint lies anterior to many important mediastinal structures such as the great vessels, the vagus and phrenic nerves, and the trachea and esophagus.
Incidence
Fractures of the clavicle occur in 1% to 13% of all births.150 The clavicle is also commonly injured during childhood, and clavicle fractures represent between 8% and 15.5% of all pediatric fractures.151 Most fractures of the clavicle involve the middle third (76%-85%). The lateral third is second most commonly involved (10%-21%); the incidence of lateral fractures increases with age. Fractures in the medial third are less common and account for only 1% to 5% of clavicle injuries in children.
Mechanism of Injury
The clavicle is the most commonly fractured bone during childbirth. The risk of birth-related clavicle fractures is increased for infants of larger birth weight (>4500 g), increased height (>52 cm), and shoulder dystocia.152 However, the majority of birth-related clavicle fractures occur in uneventful deliveries of average-birth-weight infants.
In children, falls, especially onto the shoulder, are the most common cause of fractures of the clavicle.151 Fractures of the clavicle can also occur in motor vehicle accidents and secondary to direct trauma sustained in sports such as football. Nonaccidental trauma can also be a cause. Stress fractures are rare but do occur.
Associated Injuries
Fractures involving the clavicle are at risk for serious vascular injuries, including subclavian and axillary artery disruption; subclavian vessel compression, thrombosis, and pseudoaneurysm; and arteriovenous fistulas.153–155 Brachial plexus neuropathy has also been reported in association with injuries to the clavicle.156–158 Thorough neurovascular examination of the upper extremity is warranted. Onset of neurologic deficits related to brachial plexus neuropathy can be early or late. Open reduction and stabilization of the fractured clavicle may be required.
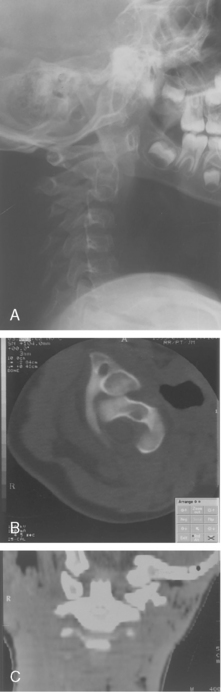
Posterior displaced fractures of the medial clavicle and posterior dislocations of the sternoclavicular joint are at particular risk for concomitant injury to the retrosternal structures in the mediastinum, including the great vessels, the esophagus, and the trachea.159–165 The index of suspicion should be raised in children who are choking or having difficulty with speaking, breathing, or swallowing. Signs of venous congestion and diminished distal pulses can also suggest associated injury. These associated injuries can be life threatening. Associated injury to the brachial plexus can also occur.
Fractures of the clavicle are rarely associated with atlantoaxial (C1-C2) rotatory subluxation (Fig. 15-15).166,167 Clinically, the head is tilted laterally toward and rotated away from the fractured clavicle. The diagnosis of C1-C2 rotatory subluxation is difficult because of the masking of the torticollis by the acute symptoms of the fractured clavicle, but it should be suspected by asymmetrical ROM. The diagnosis is best confirmed by dynamic CT.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree