Forearm Fractures: Open Reduction Internal Fixation
Steven J. Morgan
INTRODUCTION
Fractures of the diaphyseal portion of the forearm usually result from a fall on an outstretched arm or an axially directed force from higher energy injuries such as motor vehicle or motorcycle accidents. The forces generated can result in a fracture in either both bones of the forearm or an isolated fracture of the radius or ulna. Fractures in the distal one-third of the radius with disruption of the interosseous membrane leading to subluxation or dislocation of the distal radioulnar joint (DRUJ) are commonly known as Galeazzi fractures. Fractures in the proximal one-third of the ulna with an associated radial head dislocation are known as Monteggia fractures. These injuries lead to instability of the wrist or elbow joint that can only be resolved by anatomic reduction and stable internal fixation of either the radius or ulna.
Direct trauma to the forearm can also result in extra-articular fractures of the radius or ulna. With this mechanism of injury, the interosseous membrane is not grossly disrupted allowing a small number of these patients to be managed nonoperatively. With higher energy trauma, substantial fracture displacement and disruption of the soft tissues can lead to a compartment syndrome. In general, diaphyseal fractures of the forearm can be classified as a both-bone fracture, an isolated fracture of the radius or ulna, or complex injuries such as Galeazzi or Monteggia fractures. These broad descriptive terms can be further codified more scientifically using the AO/OTA Comprehensive fracture classification for descriptive and research purposes (Fig. 12.1).
The vast majority of diaphyseal fractures of the forearm require surgery because they are very difficult to reduce and maintain through healing in a cast. Strong deforming forces often lead to loss of reduction, and slow consolidation in diaphyseal bone requires prolonged immobilization. This often leads to loss of motion in the elbow, forearm, and wrist joints. Internal fixation avoids these issues allowing restoration of length and alignment and allows early functional motion of the extremity. However, even with properly done surgery, some residual deficits and functional disability may occur. Many patients lose some strength and forearm rotation. DASH scores and general health assessments reflect these deficits (1,2).
INDICATIONS AND CONTRAINDICATIONS
The radius and the ulna form a complex articulation. Loss of normal alignment results in a loss of forearm supination and pronation (3,4). Open reduction internal fixation of displaced forearm fractures in the skeletally mature patient remains the standard treatment for this injury. Internal fixation restores length, alignment, and rotation while allowing early functional range of motion of the extremity. Multiple studies have documented excellent outcomes with this method of treatment (5, 6, 7, 8, 9 and 10).
On the other hand, in a small number of patients with isolated fractures of the ulna resulting from a direct blow, nonoperative treatment can be successful. The “night stick” fracture, as it is commonly referred to, does not have the degree of soft-tissue injury that is seen in other fractures of the forearm decreasing the likelihood of associated instability of the distal or proximal radioulnar articulations. Isolated fractures involving the distal one-third of the ulna can usually be managed in a cast or brace if angulation is <10 degrees and there is no significant translation or shortening that can result in significant functional impairment at the DRUJ.
Internal fixation of isolated ulna fractures, regardless of injury mechanism, is recommended in open fractures, injuries with angulation >10 degrees, and in fractures with significant comminution or shortening (11).
Internal fixation of isolated ulna fractures, regardless of injury mechanism, is recommended in open fractures, injuries with angulation >10 degrees, and in fractures with significant comminution or shortening (11).
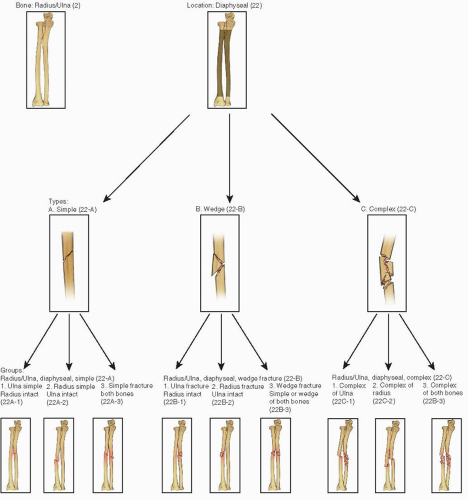 FIGURE 12.1 AO/OTA fracture classification. (Reprinted from J Orthop Trauma 2007;21(10 suppl), with permission.) |
Preoperative Planning
History and Physical Examination
A thorough history and physical examination and high-quality radiographs of the forearm, elbow, and wrist are necessary to develop a treatment plan. The history should provide information as to the mechanism of injury, hand dominance, occupation, previous injury, and associated medical problems. The entire extremity should be examined for associated injuries. Circumferential inspection of the extremity is necessary to identify the presence of an open fracture as well as to assess the extent
and severity of the soft-tissue injury. Any violation of the skin in proximity to the fracture site should be considered an open fracture until proven otherwise. Ecchymosis, fracture blisters, and swelling suggest significant soft-tissue injury and the index of suspicion for compartment syndrome should be high. The forearm should be palpated for tenderness, and the elbow, wrist, and carpus should receive special attention as injuries to these anatomic structures are not uncommon. The neurologic examination should document the integrity of the motor and sensory status of the radial, posterior interosseous, ulnar, and median nerves. Vascular examination should focus on limb perfusion, and the brachial, radial, and ulnar pulses must be assessed.
and severity of the soft-tissue injury. Any violation of the skin in proximity to the fracture site should be considered an open fracture until proven otherwise. Ecchymosis, fracture blisters, and swelling suggest significant soft-tissue injury and the index of suspicion for compartment syndrome should be high. The forearm should be palpated for tenderness, and the elbow, wrist, and carpus should receive special attention as injuries to these anatomic structures are not uncommon. The neurologic examination should document the integrity of the motor and sensory status of the radial, posterior interosseous, ulnar, and median nerves. Vascular examination should focus on limb perfusion, and the brachial, radial, and ulnar pulses must be assessed.
Imaging Studies
Full-length anterior posterior and lateral radiographs of the forearm that include the elbow and wrist should be obtained. Dedicated x-rays of the elbow or wrist joints may be necessary based on the clinical exam or preliminary x-rays. In the multiply injured patient, or in patients with severe soft-tissue injury or neurologic or vascular compromise, a provisional reduction and splint should be applied prior to obtaining radiographs. In comminuted fractures, traction x-rays can be very helpful to better define the extent of injury. Difficult to obtain without adequate analgesia, these radiographs are best obtained in the operating room following induction of anesthesia prior to surgery. Occasionally, stress x-rays of the elbow or wrist can reveal subtle or gross instability that may influence treatment.
Timing of Surgery
Surgical timing is largely dependent on the condition of the soft tissues and the general condition of the patient. For most isolated closed fractures without neurovascular compromise, internal fixation should be done within 24 to 48 hours of injury. In patients with a compartment syndrome, I favor immediate internal fixation following fasciotomy with few exceptions. Other indications for emergent surgery are widely displaced Galeazzi or Monteggia fractures or patients with acute carpal tunnel syndrome. For most Grade I, II, and IIIA open fractures, thorough irrigation and debridement with immediate fracture stabilization has been shown to be safe and effective. For some Grade IIIA and Grade IIIB high-energy open fractures, particularly in the multiply injured patients, irrigation and debridement and delayed internal fixation are warranted. In these cases, simple temporary spanning external fixation can be helpful.
In the emergency room, a coaptation or long arm splint is applied. Temporary immobilization of the fracture controls pain and restores gross alignment to prevent further soft-tissue injury while awaiting definitive fracture fixation. In a Monteggia fracture with a radial head dislocation, gentle traction and supination using conscious sedation or regional anesthesia (bier block) will often reduce the dislocation, allowing splint application of the extremity. Following any manipulation of the forearm, the neurologic and vascular status of the extremity should be reevaluated and documented.
Surgical Tactic
A thorough understanding of the soft-tissue injury and fracture pattern is necessary to make a surgical plan. This is based on the overall condition of the patient, the location of an open wound (if present), the degree of fracture comminution, and the quality of the bone. The location of an open wound will influence the surgical approach. We frequently incorporate the traumatic wound into the surgical exposure for internal fixation and thoroughly debride the wound in the zone of injury. For example, a large dorsally based wound over the radius may dictate a dorsal (Thompson) exposure as opposed to the more familiar volar approaches. Certainly not every open fracture lends itself to a surgical approach that allows wound debridement and internal fixation with one incision. In open fractures where both the radius and ulna are involved, the sequence of the surgical approach is determined by which bone is associated with the open wound. Once the fracture site and soft-tissue injury are debrided, the order of fixation is based on the fracture pattern rather than the open injury.
Internal fixation of a forearm fracture should restore length, rotation, and alignment using implants that provide stable fixation that allows early functional rehabilitation. When length is reestablished in one of the two bones, the other bone is often indirectly reduced by the surgical actions taken on the first, simplifying the second reduction. With noncomminuted fractures of the forearm, I prefer to fix the radius first. This tactic is selected because it allows the arm to remain extended on the arm table and facilitates exposure and reduction of the radius. Once the radius is fixed, the elbow can be flexed facilitating exposure and fixation of the ulna.
In the situation where there is comminution of one fracture and a simple fracture pattern exists in the other bone, the noncomminuted fracture should be reduced and fixed first. This helps to reestablish the correct length of the more comminuted fracture indirectly. When both bones are comminuted, the least comminuted fracture is approached first. If there is no significant difference in the two bones, the radius is generally approached first for the reasons previously stated.
The surgical exposure, reduction, and fixation of each bone are performed sequentially. Exposing both of the bones of the forearm prior to reduction and internal fixation is indicated only in cases where surgery has been delayed (3 weeks). However, the incisions should not be closed until the fracture reduction and fixation of both bones are satisfactory. By leaving the wounds open and closing both at the end of the case, access to both sites is available if difficulty is encountered.
In open fractures, irrigation and debridement with immediate plate fixation has been shown to be both safe and effective (8,12). In the critically ill multiply injured patient with an open forearm fracture, temporary external fixation following irrigation and debridement with delayed internal fixation can be helpful. In comminuted
fracture patterns, the use of bone graft at the completion of the procedure remains controversial. If indirect reduction techniques with bridge plating are utilized, then bone grafting is not necessary. However with Grade III open fractures, bone loss, or long zones of comminution where the fracture site is dissected, bone grafting is strongly recommended. Autogenous bone grafts or bone graft substitutes should be used on an individualized basis.
fracture patterns, the use of bone graft at the completion of the procedure remains controversial. If indirect reduction techniques with bridge plating are utilized, then bone grafting is not necessary. However with Grade III open fractures, bone loss, or long zones of comminution where the fracture site is dissected, bone grafting is strongly recommended. Autogenous bone grafts or bone graft substitutes should be used on an individualized basis.
Implant Selection
The implant of choice for virtually all diaphyseal forearm fractures in adults is a 3.5-mm dynamic compression plate and is available in full contact and limited contact design in either titanium or stainless steel. In theory, a limited contact dynamic compression (LCDC) decreases devitalization of the underlying bone, and titanium implants may decrease stress shielding. In practice, excellent results can be achieved with either implants and carefully executed surgery. Plates with locking screw options have become available in the past decade; however, the indications for its use remain undefined. Most authors recommend its use in elderly patients with osteoporosis and selected metadiaphyseal fractures (13,14).
Implant selection and plate length should be determined preoperatively. Overlay implant templates are available and should be part of the surgical tactic. Digital PACS templating has become more common, and the technology continues to evolve. In noncomminuted fractures, a minimum of six cortices in each fragment are recommended. For comminuted fractures, six to eight cortices of fixation in each fragment should be employed. In these cases, one or more holes in the zone of comminution are left empty. If locking screws are utilized, bicortical fixation significantly improves mechanical strength. The ideal plate length and construct stiffness for optimal fracture healing remain unknown. The use of longer plates, spaced screws, and a combination of conventional and locking screws may influence fracture healing.
SURGICAL TECHNIQUE
The patient is positioned in the supine position, and the extremity is supported on a hand table. A nonsterile tourniquet is applied to the upper arm. C-arm access is often facilitated by rotating the table 45 or 90 degrees so the operative extremity is centered in the room. The image intensifier is brought in from the end of the hand table obviating the need for the surgeon or his or her assistant to move (Fig. 12.2). Cefazolin 1 to 2 g should be administered at the beginning of the case. Patients with a penicillin allergy or a history of MRSA are given vancomycin as an alternative. In closed fractures, patients receive one or two additional doses of antibiotics postoperatively. In open fractures, the duration of antibiotics is individualized based on the severity of the wound and the degree of contamination.
Surgery can be performed using general or regional anesthetic techniques. Regional anesthesia with long-acting pharmacologic agents is contraindicated in most patients with diaphyseal forearm fractures due to the risk of masking a postoperative compartment syndrome (15).
In comminuted diaphyseal fracture patterns, if there is any question regarding the fracture geometry or morphology, traction radiographs should be obtained under anesthesia prior to prepping and draping. The extremity is prepped and draped from fingertips to the tourniquet. In patients with open fractures, the tourniquet is not inflated, to prevent further ischemic injury to the traumatized soft tissue. In closed fractures, surgery is routinely performed under tourniquet control. In large or swollen arms, the C-arm is used to identify the location of the surgical incisions that are drawn on the extremity using a sterile marking pen. Loop magnification is recommended to improve visualization and dissection and to control bleeding. Bipolar cautery and small ligature clips are utilized liberally during the dissection.
 FIGURE 12.2 The surgeon and assistant are seated on either side of the hand table, and the C-arm is brought directly in line with the extremity. |
SURGICAL APPROACHES
Flexor Carpi Radialis Approach
For fractures involving the distal one-fourth of the radius, a volar approach based on the flexor carpi radialis (FCR) muscle and tendon is utilized. A skin incision of appropriate length is made just radial to the tendon (Fig. 12.3). Following the skin incision, the FCR tendon sheath is split longitudinally and the FCR tendon is retracted ulnarly. The floor of the tendon sheath is then incised. The flexor pollicis longus (FPL) is identified and retracted ulnarly, which protects the median nerve. The pronator quadratus is elevated from the radius and retracted ulnarly exposing the distal one-fourth of the radius (Fig. 12.4). This exposure avoids a direct dissection of the radial artery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








