Fixation of Posterior Plateau Fractures via Posterior Approaches
Erik Noble Kubiak
DEFINITION
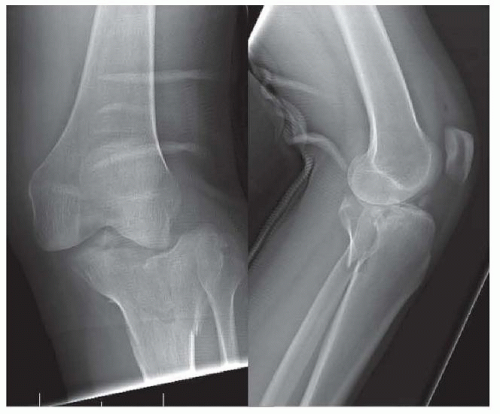
A direct approach with the patient in a prone position to the posterior aspect of the tibial plateau for reduction and stable fixation of tibial plateau fractures which are hard to visualize from conventional anterolateral or extensile medial approaches. Most applicable to fracture-dislocations of the knee (FIG 1).
The approach to the posterior aspect of the proximal tibia was originally described in the French surgical literature by Cadenat3 in 1933. Later, the approach was further described in the English literature by Darrach5 in 1945 and Harmon7 in 1945. Kaplan9 in 1946 provided an excellent description of the anatomy of the approach, although none of these authors described the use of the posterior approach to the proximal tibia for fracture fixation.
More recently, Lobenhoffer et al10 in 2004 described a limited posterior approach for tibial plateau fracture fixation that has been popularized by subsequent authors that uses the medial aspect and dissection of the extensile approach for the treatment of posteromedial tibial plateau fractures. This can be combined with anterolateral approach for bicondylar tibial plateau fractures during staged management, but it is hard to perform concurrently with an anterolateral tibial plateau approach. Carlson4 added the posterolateral incision and dissection for the treatment of posterior dominant bicondylar fractures.
Further modification of the posterolateral approach by adding an osteotomy of the proximal fibula has been described Yu et al15 to improve exposure to the proximal posterolateral tibial plateau. In some circumstances, the fibular osteotomy comes as part of the fracture and this can be exploited to improve fracture visualization.
ANATOMY
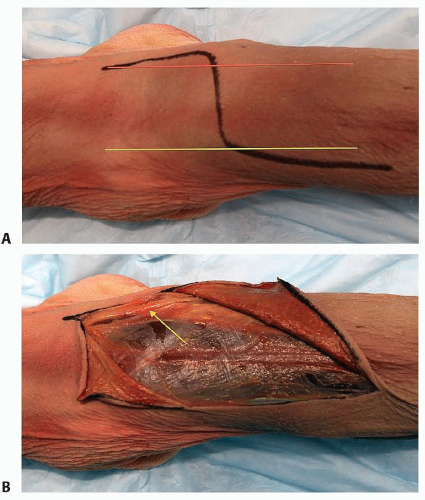
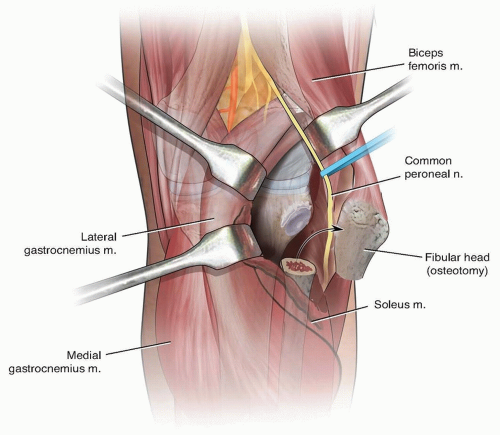
Dissection and approach to the posterior aspect of the proximal tibia is performed primarily through three tissue planes: medial, middle, and lateral, all of which are part of the extensile posterior approach (FIG 2A,B).
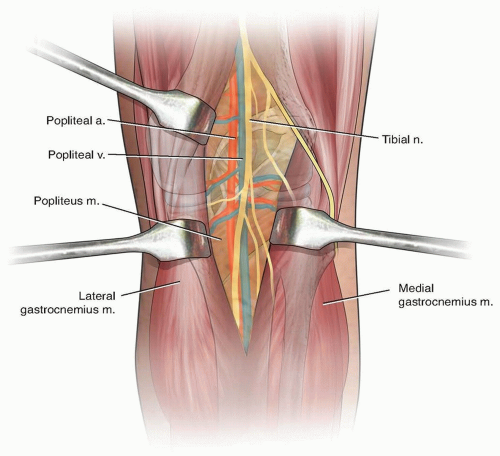
The medial tissue plane is bounded superiorly by the semimembranosus muscle, the medial head of the gastrocnemius laterally, and the soleus and popliteus inferiorly. The inferior medial geniculate neurovascular bundle is at risk during this dissection if not disrupted by fracture displacement (FIG 3).
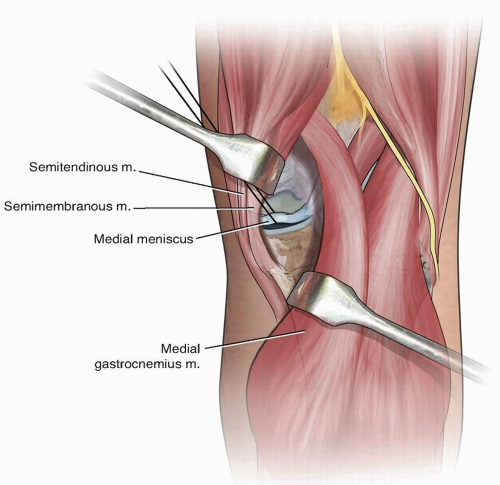
FIG 3 • Posteromedial tibial plateau approach described by Lobenhoffer10 and popularized by Smith et al. The posteromedial approach offers easy access to the posterior aspect of the medial tibial plateau. Reduction and application of buttress fixation of the medial coronal plane splits in the medial plateau are facilitated by this exposure which is posterior to the hamstring tendons and the medial collateral ligament. Visualization of the concave surface of the medial tibial plateau is difficult. Reduction is provisionally performed via cortical reads, and the reduction of the articular surface is confirmed radiographically.
The middle tissue dissection is bounded medially by the medial head of the gastrocnemius, laterally by the lateral head of the gastrocnemius, and inferiorly by the popliteus muscle. The posterior tibial nerve, artery, and venous drainage are at greatest risk during this approach. The rich venous return coming from the gastrocnemius heads is tedious to dissect during this approach plane (FIG 4).
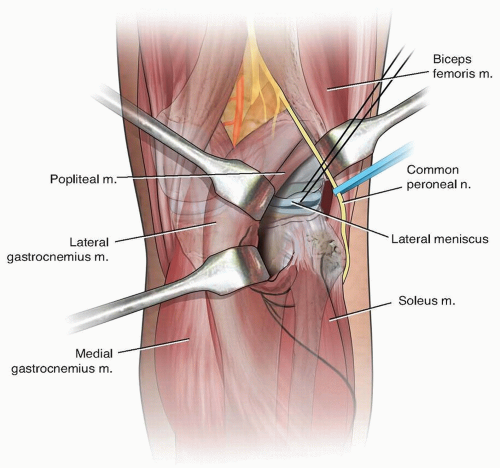
The lateral dissection is bounded superiorly by the popliteus muscle, medially by the lateral head of gastrocnemius, laterally by the posterior aspect of the fibula and the common peroneal nerve, and inferiorly by the soleus. The common peroneal nerve and popliteal artery and nerve are at risk (FIG 5). Proximal fibular osteotomy can be used to improve exposure (FIG 6).
PATHOGENESIS
Direct posterior approaches to the tibial plateau are indicated for reduction and stabilization of fractures of the posterior aspect of the tibial plateau that can either be isolated to a single condyle or bicondylar in nature.
The posterior fracture of the tibial plateau is most commonly associated with fracture-dislocation injuries of the knee wherein the tibia subluxates anteriorly and the femoral condyles impact the posterior aspect of the proximal tibia. Rotation and degree of knee flexion at the time of injury determine condylar involvement, whereas degree of axial loading drives the amount of joint impaction.
Most common in Moore types 1 and 2 fracture-dislocations of the knee
We see this most commonly in skiers who sustain Schatzker 4 injuries as described by Potocnik et al.11
Occasionally, Schatzker 2 split depression injuries involve the posterior aspect of the lateral tibial plateau and are amenable to a direct posterolateral approach.
NATURAL HISTORY
Most high-energy periarticular injuries are treated in a staged manner wherein the knee is initially stabilized in an external fixator (see Chap. 47), allowing the soft tissue envelope to evolve to the point that swelling is resolving and any fracture blisters have reepithelialized.
The decision to proceed with open reduction and internal fixation can been made once the soft tissue envelope is no longer being actively damaged and has moved past the acute inflammatory phase (generally >5 days).
Healing of metaphyseal fractures generally occurs slowly by creeping substitution and therefore requires prolonged periods of protected weight bearing (10 to 12 weeks).
PATIENT HISTORY AND PHYSICAL FINDINGS
Advanced trauma life support (ATLS) guidelines. Comprehensive physical examination to determine all associated injuries.
Examination of the affected lower leg. Documenting the neurovascular status of the limb. Ankle-brachial indices should be obtained; values less than 0.9 should trigger a vascular consult.
Soft tissue injuries should be documented as well as previous scars.
A high index of suspicion should be maintained for compartment syndrome before and after placement of external fixation, if used.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Orthogonal radiographs of the knee to include anteroposterior (AP) and lateral images.
Contralateral knee orthogonal images: AP and lateral. The author’s preference is to control for subtle anatomic differences between individuals. The contralateral radiographs allow the surgeon to reconstruct the fractured knee in the mirror image of its uninjured partner.
A computed tomography (CT) of the knee is invaluable in determining the exact location of the articular injury to the tibial plateau (FIG 7). This includes the location of the impaction that needs to be elevated. The CT scan should be obtained after spanning external fixation when a staged operative approach is selected. Sagittal and coronal reconstructions may also be helpful.
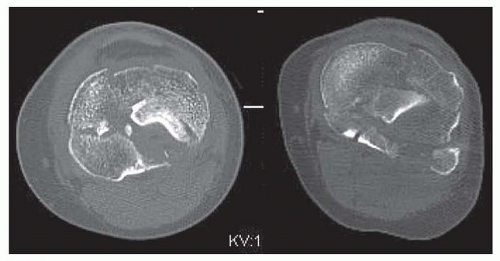
FIG 7 • Axial CT clearly demonstrates the position of articular impaction of the posterolateral tibial plateau. Direct visualization and reduction of the articular surface is possible via a posterolateral approach.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access