Fig. 15.1
First ray osteomyelitis is most commonly associated with contiguous spread of infection from adjacent neuropathic ulcers. Neuropathic ulcers are classically located over points of boney prominence or excessive pressure including (a) the plantar aspect of the first metatarsal head and sesamoids, (b, c) distally at the tip of the first toe or dorsally over the first interphalangeal joint associated with hallux hammertoe, (d, e) along the medial first metatarsal head associated with hallux valgus, and (f) plantar to the first interphalangeal joint associated with hallux rigidus, hallux valgus, or hallux interphalangeus
Osteomyelitis along the medial column is a frequently encountered problem in the diabetic foot which directly correlates with the high incidence of hallux ulceration [1, 2]. Although neuropathy is the leading risk factor for first ray ulceration, other factors play a role in the etiology of tissue breakdown including deformity and poor circulation. Abnormal mechanics and structural deformities cause pathologic stress on the local tissues and significantly influence ulcer location, propensity for poor healing, and ultimately the development of osteomyelitis [3, 4]. Foot and ankle deformities including hallux limitus, hallux valgus, hallux hammertoe, and ankle equinus are known risk factors for first ray ulceration [3]. Although not as common, nonstructural etiologies such as gout, gangrene, septic joint, toenail trauma, puncture wounds, and open fractures can also lead to the formation of osteomyelitis (Fig. 15.2).
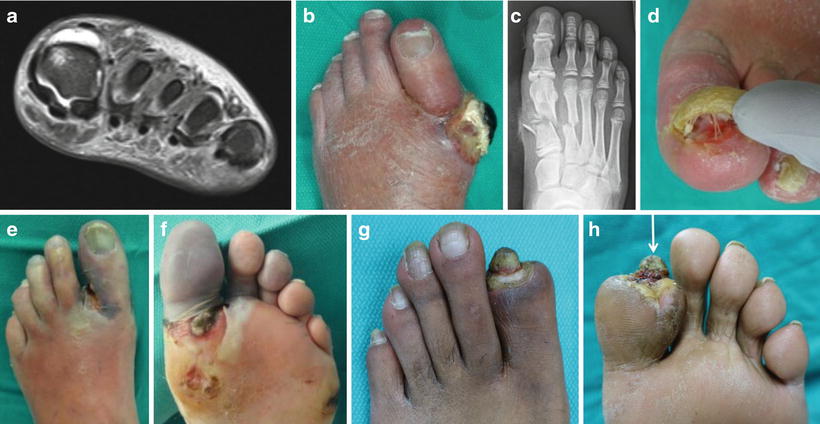
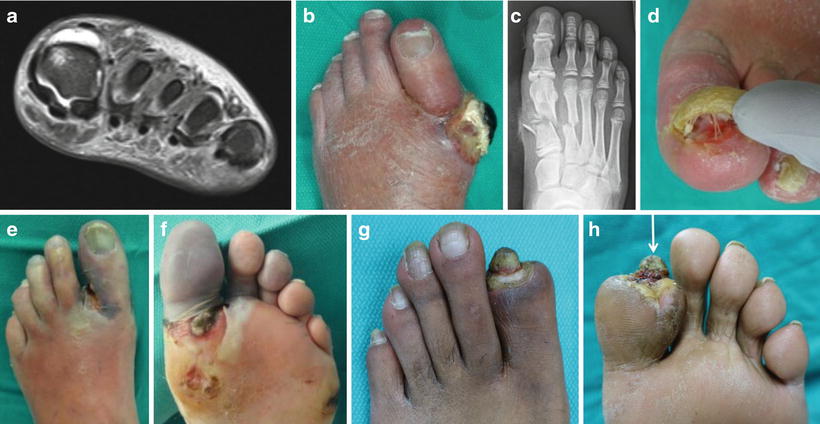
Fig. 15.2
Non-neuropathic ulcer related first ray osteomyelitis. (a) First ray osteomyelitis is rarely associated with hematogenous osteomyelitis although the first metatarsal phalangeal joint can develop hematogenous joint sepsis with secondary adjacent osteomyelitis seen here on MRI. (b) Ulcerated tophaceous gout commonly leads to contiguous spread of infection. (c) Direct inoculation may occur through puncture wound or open fractures. (d) Toenail-related infections and nail bed wounds can lead to osteomyelitis of the distal phalanx. (e, f) Infected gangrene commonly results in osteomyelitis. (g, h) Autoamputation of full thickness dry gangrene will commonly lead to bone exposure and secondary osteomyelitis (note exposed bone at tip of arrow)
A combined medical and surgical treatment protocol is generally preferred for first ray osteomyelitis in an effort to address not only bone infection but also the soft tissue wound defect and underlying mechanical or structural issues. The ideal surgical plan should also attempt to preserve the important weight bearing function of the first ray when possible. Incision and drainage of infection, excision of the ulcer, conservative bone resection or amputation, implantation of antibiotic beads, immediate or delayed wound closure, and antibiotic therapy are commonly incorporated to provide a global approach to this potentially limb-threatening condition. Staged surgery and integration of rotational flaps are common in the surgical treatment of first ray osteomyelitis since continued bone exposure at the site of a nonhealing wound often leads to persistent or recurrent osteomyelitis despite long-term postoperative antibiotic therapy. Failure to address the source of abnormal pressure predisposes to the dilemma of recurrent wound breakdown which is detrimental to the pursuit of a clinical cure of osteomyelitis. Conservative bone resection at the site of osteomyelitis allows removal of the nidus of infection, provides specimen for bone biopsy, and has the potential to address the source of bone prominence or abnormal mechanics [5]. A biomechanically sound procedure could actually improve the function of the first ray or at least decrease the likelihood of recurrent ulceration which goes against the commonly held belief that surgery should be a last resort option.
Some degree of first ray amputation is commonly performed for osteomyelitis and ranges from partial hallux amputation to complete first ray amputation. Compared with amputation of other toes, there are added undesirable consequences associated with first ray amputation including transfer ulcers at adjacent areas leading to repeat infection and further amputation [6, 7]. Reconstructive podiatric procedures are oftentimes appropriate for nonhealing wounds with suspected osteomyelitis provided that surgery is performed early while the local soft tissues remain viable. Reconstructive approaches commonly involve limited bone resection which allows early bone biopsy and creates laxity in the tissue allowing use of a rotational flap to close the wound. Amputation is more likely in the setting of tissue necrosis, extensive bone infection, severe deformity, and failed prior procedures. This may be the consequence of waiting too long to address a seemingly stable first ray ulcer. Amputation may be prevented by an early decision to pursue elective surgical treatment after a reasonable period of conservative wound management has been unsuccessful due to underlying mechanical issues. The surgeon ultimately needs to decide what is best for an individual patient based on his or her unique set of circumstances.
The extent and location of both the wound and the osteomyelitis are important factors when selecting the ideal surgical treatment plan. The bone immediately adjacent to the ulcer is most prone to contiguous spread of infection. Neuropathic ulcers frequently develop over joints which predisposes to infection from contiguous spread to one or both of the adjacent bones. Common first ray wound locations include the tip of the hallux, the dorsal IPJ, the plantar IPJ, the medial MPJ, and the plantar MPJ. Figure 15.3 is a flowchart of common first ray surgical treatment pathways based on location of the wound and expectation of osteomyelitis based on clinical, laboratory, and radiographic workup. Elective procedure pathways are also provided for nonhealing wounds with low likelihood of bone infection or early and localized osteomyelitis. Early intervention with elective, reconstructive wound surgery provides bone biopsy and may allow resolution of the wound prior to the onset of osteomyelitis. Short first ray resection near the metatarsal base has a significant impact on foot stability, medial column function, and second ray overload. Resection near the base may also add risk for future conversion to transmetatarsal amputation (TMA) and is avoided when possible. Procedure and patient selection criteria including surgical technique and staging pearls are detailed below.
Fig. 15.3
Procedure selection flowchart for first ray osteomyelitis. This flowchart outlines common first ray surgical treatment pathways based on location of the wound, expectation of osteomyelitis, and underlying biomechanical deformity. Elective procedure pathways are also provided for nonhealing wounds with low likelihood of bone infection or early and localized osteomyelitis. The ideal procedure for a given patient should address abnormal mechanics and structural deformities yet minimize the potential for transfer ulcers
Reconstructive Procedures
Hallux Hammertoe Procedures
Hallux hammertoe deformity is frequently associated with tip-of-toe ulcers, dorsal IPJ ulcers, and plantar MPJ ulcers. It is reasonable to pursue elective hammertoe surgery in an attempt to address the underlying structural deformity before osteomyelitis develops, which puts the toe at risk for amputation. The open wound would ideally be healed prior to elective surgery, but this is not always practical as deformity correction may be necessary to resolve the wound. Hallux hammertoe repair typically consists of flexor hallucis longus (FHL) tenotomy, IPJ fusion, or IPJ arthroplasty. Extensor hallucis longus (EHL) lengthening or transfer to the first metatarsal head is added if the EHL is a contributing deforming force. Ideal procedure selection depends on the flexibility of IPJ and MPJ deformity, location and depth of the ulcer, and suspicion for osteomyelitis. Elective surgery frequently allows procurement of bone for biopsy and primary or flap closure of the wound. The simplest approach is an office-based FHL tenotomy which is indicated for reducible IPJ contracture without bone or soft tissue infection, as shown in case 1 (Figs. 15.4, 15.5, 15.6, and 15.7). This ambulatory procedure is highly amenable to the office setting in patients with neuropathy, and there is no need to hold anticoagulation therapy as bleeding is minimal. Immediate weight bearing is preferred to promote stretch after tendon and joint release. Deep and complicated tip-of-toe ulceration is often best treated with hallux distal Symes amputation as described later.


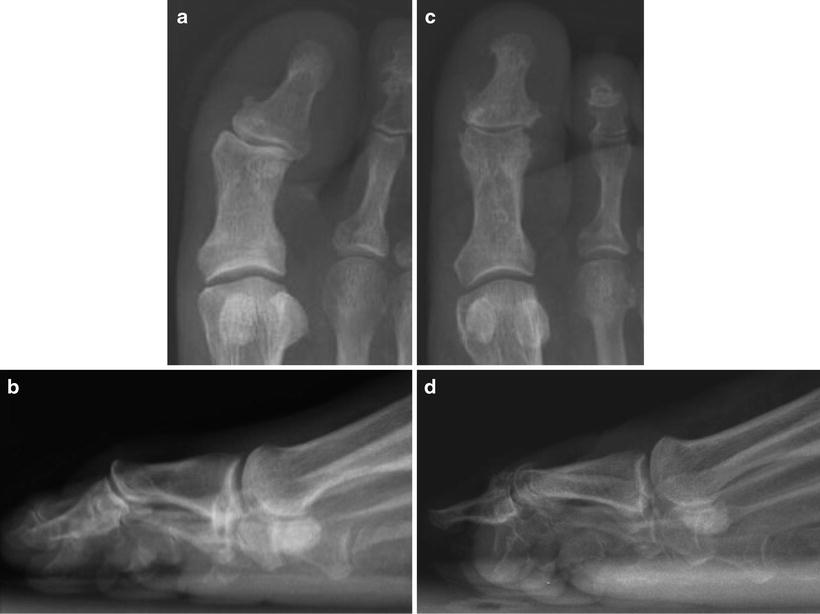


Fig. 15.4
Case 1: Tip-of-toe hallux ulceration associated with hammertoe contracture. (a, b) A contracted first toe placed substantial pressure at the tip of the toe where the distal phalanx is fairly superficial. Neuropathic ulcers related to hammertoe deformity tend to become chronic and eventually deepen which results in osteomyelitis and loss of the toe. Early intervention to address the deformity may allow prompt wound healing and preservation of the digit. Consideration was given to interphalangeal joint arthroplasty or fusion although FHL tendon release was performed since the contracture was flexible. Reconstructive procedures are best performed prior to the onset of osteomyelitis or soft tissue infection. A course of orthotic treatment and wound care is reasonable, but significant deformity may be best treated with surgery. Note that longer shoes do not solve ulcers caused by hammertoe contracture and tenotomy may make the toe longer

Fig. 15.5
Flexor hallucis longus tenotomy was performed through a percutaneous plantar incision in case 1. The plantar incision was placed approximately mid-proximal phalanx where the FHL tendon (linear line) is subcutaneous, narrow, and easily accessible. A more distal IPJ incision is possible, but the tendon widens at the insertion point on the base of the distal phalanx. The transverse incision (dotted line) was within the skin lines which healed within 1 week and no suture was required
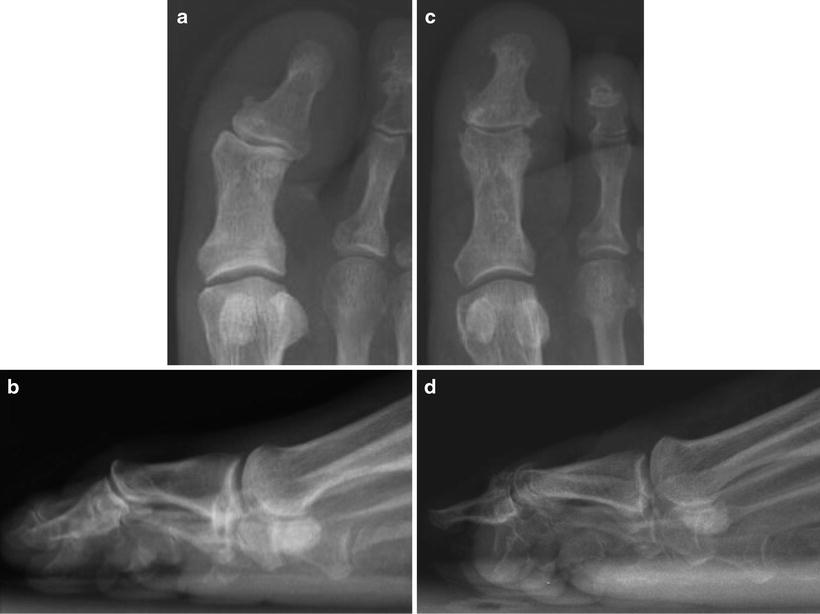
Fig. 15.6
Preoperative and post-FHL tenotomy radiographs involving tip of hallux ulceration in case 1. (a, b) Preoperative AP and lateral weight bearing radiographs show contracture deformity at the hallux interphalangeal joint (IPJ). No signs of osteomyelitis were seen at the tip of the distal phalanx. (c, d) Postoperative AP and lateral weight bearing radiographs show fairly normal positioning of the IPJ with pressure now applied to the plantar digital pulp which is well padded

Fig. 15.7
Clinical appearance 4 weeks after flexor hallucis longus tenotomy in case 1. (a, b) Weight bearing clinical photos show a straight first toe that no longer placed pressure on the distal tip of the hallux. Note that the second toe had contracted slightly which is commonly seen and thought to be related to interconnection between the flexor hallucis longus and flexor digitorum longus at the master knot of Henry. Prophylactic lengthening of the second toe is common to avoid transfer lesions. (c) The tip of the toe hallux ulcer was nearly healed at 4 weeks postoperatively despite full weight bearing which helped to stretch the lengthened tendon
Rigid deformity of the IPJ is generally treated with joint fusion or arthroplasty (Fig. 15.8). Interphalangeal joint fusion requires internal fixation or pin fixation which is less practical in patients with open wounds or suspected osteomyelitis. If uncomplicated wounds can be healed preoperatively and the risk of osteomyelitis is low, elective hallux fusion is preferred. This approach leads to a more stable and functional toe. A staged approach is also possible with initial FHL tenotomy followed by delayed fusion once the distal ulcer heals.


Fig. 15.8
Hallux IPJ fusion or arthroplasty for hallux hammertoe deformity. (a, b) Joint fusion requires internal fixation or percutaneous pins, which is not always practical in patients with complicated wounds or suspected osteomyelitis. Uncomplicated wounds can oftentimes be healed preoperatively allowing successful fusion. Infection can also be ruled out preoperatively with bone biopsy or advanced imaging including bone scan or MRI. (c) Hallux IPJ arthroplasty involves removal of the head of the proximal phalanx. This releases contracted soft tissues to reduce pressure dorsal, plantar, or medially at the IPJ and at the tip of the toe
Hallux IPJ Arthroplasty with Unilobed Rotational Plantar Flap
A primary indication for hallux IPJ arthroplasty is a nonhealing IPJ plantar ulceration with suspected or imminent osteomyelitis within the head of the proximal phalanx, as demonstrated in case 2 (Figs. 15.9, 15.10, 15.11, 15.12, 15.13, 15.14, 15.15, 15.16, 15.17, 15.18, and 15.19). We commonly incorporate a unilobed flap with or without a secondary dorsal incision for bone resection [8]. A dorsal incision is helpful when patients present with cellulitis and inflammation on the dorsum of the hallux despite the wound being plantar as these clinical signs likely indicate violation of the joint capsule. Since infection most commonly spreads from an area of higher pressure (plantar foot) to an area of lower pressure (dorsal foot), the spread of infection to the dorsum of the foot is common once the joint capsule is compromised [9]. A course of conservative wound treatment is warranted but often ineffective for IPJ ulcer treatment due to abnormal biomechanical forces. Surgical intervention would ideally be implemented before cellulitis or osteomyelitis develops, but a staged approach is common with acute infection.




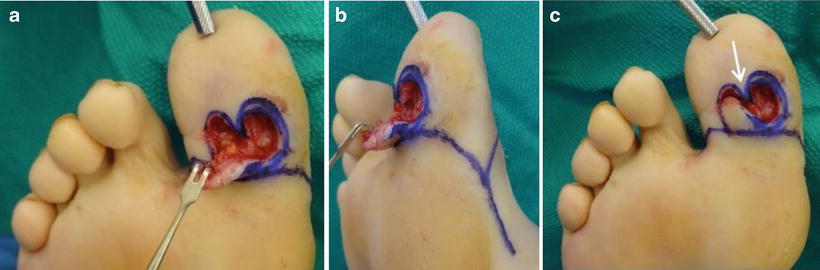

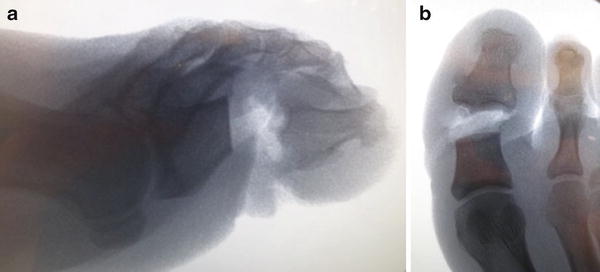

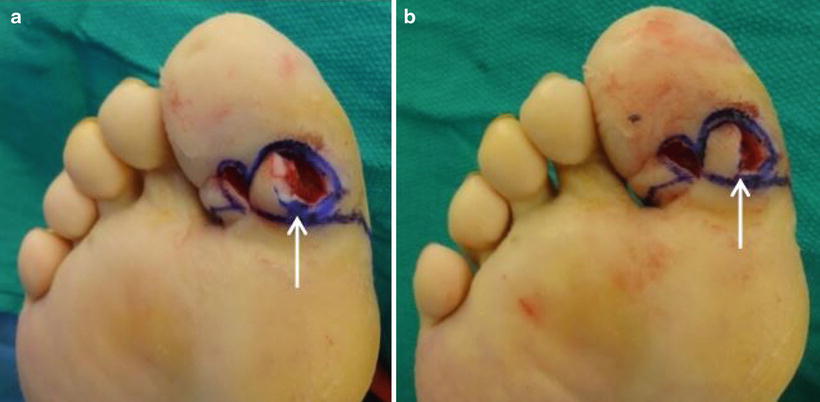



Fig. 15.9
Case 2: Hallux IPJ plantar ulcer. (a) A typical nonhealing plantar medial hallux IPJ neuropathic ulcer is shown. (b, c) Slight valgus deformity of the toe and functional hallux limitus contributed to excessive pressure and wound formation. Note low-grade, but persistent, erythema to the dorsal IPJ area despite the plantar wound location raising suspicion for joint infection and osteomyelitis

Fig. 15.10
Preoperative imaging in case 2. (a, b) X-rays were fairly unremarkable with the exception of lateral deformity at the IPJ. Radiographic changes consistent with osteomyelitis are a relatively delayed finding. Early diagnosis of osteomyelitis requires clinical suspicion based on the nonhealing nature of the wound, local soft tissue infection, positive probe to bone, laboratory workup including infection marker labs, and advanced imaging. X-rays are useful to evaluate for structural deformity such as hallux interphalangeus, interphalangeal joint sesamoid bone, hallux limitus, hallux valgus, bone spurs, malaligned fractures, and degenerative joint disease. Early radiographs also serve as a baseline for later comparison

Fig. 15.11
Incision plan for hallux IPJ arthroplasty and unilobed rotational flap in case 2. (a, b) The incision for hallux amputation was drawn prior to making the flap incision. This ensures that the flap donor site does not compromise later conversion to hallux amputation as this is the fallback procedure depending on intraoperative findings or postoperative healing process. (c) The unilobed flap was then drawn lateral to the plantar medial IPJ ulcer. The length and width of the flap should roughly match the size of the wound defect left after excision of the ulcer but can be approximately 25 % smaller in both dimensions due to secondary movement of the surrounding tissues upon flap rotation and closure of the donor site

Fig. 15.12
Wound excision technique in case 2. The wound was excised full depth with a no-touch technique. The flexor hallucis longus tendon is preserved if it appears healthy and functional. Gloves were changed at this point and the wound was re-prepped prior to raising the flap
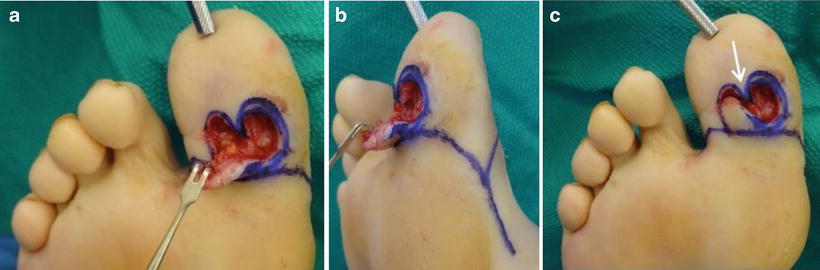
Fig. 15.13
Raising the unilobe flap in case 2. (a, b) The flap is incised and raised full thickness using a skin hook for a no-touch technique. (c) It is important to preserve the central frenulum (arrow) as this will help with closure of the flap donor site. Bone resection can be performed through the plantar wound, but a secondary dorsal approach is common with smaller flaps

Fig. 15.14
IPJ arthroplasty through a secondary dorsal incision in case 2. (a) A lazy S-type transverse dorsal incision was made over the IPJ. Note how the incision did not compromise the dorsal flap should conversion to toe amputation becomes necessary. (b) The EHL tendon was cut transversely and repaired after bone resection. (c) A sagittal saw was utilized for bone resection, and (d) the head of the proximal phalanx (arrow) was removed
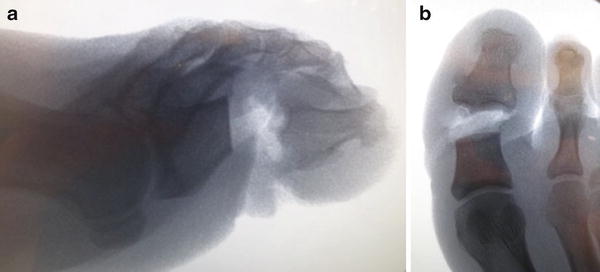
Fig. 15.15
Intraoperative imaging to confirm adequate bone resection in case 2. (a, b) Intraoperative imaging is helpful to ensure adequate resection proximal to the metaphyseal flare on the proximal phalanx. Inadequate bone resection increases the risk of re-ulceration, especially if the plantar flare remains. Excessive bone resection leads to instability and loss of function of the distal toe

Fig. 15.16
Removal of the IPJ sesamoid bone in case 2. An IPJ sesamoid bone is almost always located beneath the head of the proximal phalanx at the IPJ which likely contributes to plantar prominence. This may or may not be visible on X-ray depending on imaging technique and degree of ossification. The IPJ sesamoid was resected, taking care not to disrupt the long flexor tendon
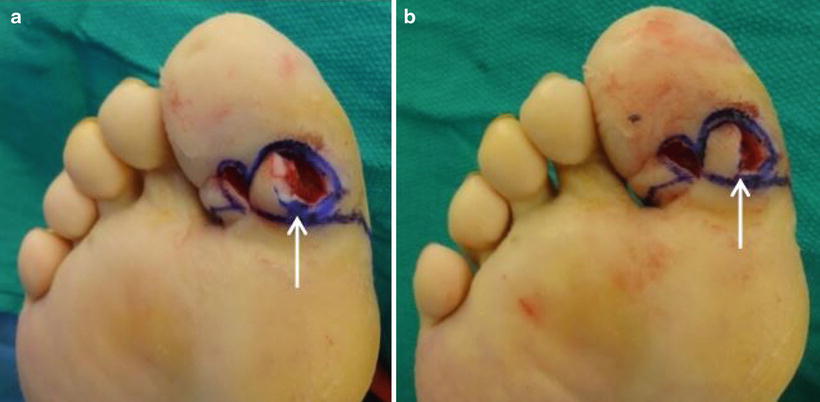
Fig. 15.17
Rotation of the unilobed flap into wound defect in case 2. (a) Using a minimal touch technique, the unilobe flap was rotated medially into the wound defect. Note that a curved point of rotation creates a dog ear (arrow). (b) The flap rotated without creating a dog ear after the point of rotation (arrow) was converted to a 90° angle

Fig. 15.18
Unilobed rotational flap closure in case 2. (a–c) The plantar flap, donor site, and dorsal incisions were closed with simple interrupted sutures. Dorsal sutures are removed at 2 weeks, but plantar sutures are typically removed at 4–6 weeks depending on healing

Fig. 15.19
Postoperative results after IPJ arthroplasty and unilobed rotational flap in case 2. (a, b) Ten week postoperative clinical presentation and (c, d) X-rays with apparent resolution of osteomyelitis and chronic ulceration based on clinical, laboratory, and radiographic evaluation. Osteomyelitis was confirmed on microbiologic and pathologic biopsy, but no clean margin was taken. Inflammatory marker labs had returned to normal. Concomitant gastrocnemius recession was performed to reduce the risk of recurrent ulceration. (e, f) Six-month postoperative clinical presentation
The benefits of this digital salvage procedure include complete ulcer excision, early bone resection and biopsy, flap coverage with viable soft tissue, and offloading of mechanical pressure at the plantar hallux IPJ. Care is taken to select patients with adequate MPJ dorsiflexion and healthy surrounding soft tissue which is more likely with early intervention before the onset of extensive soft tissue or bone infection. Clinical exam of patients with ulcers at the plantar IPJ location commonly identifies hyperextension of the IPJ associated with functional hallux limitus. Plantar IPJ bone prominence is also common along with ankle equinus deformity. A weight bearing stress dorsiflexion lateral hallux view is helpful to assess for functional MPJ range of motion [10]. Standard weight bearing X-rays are also useful to evaluate for osteomyelitis, a prominent plantar IPJ sesamoid, or other causes of excessive plantar pressure at the IPJ. MRI may also help determine the extent of osteomyelitis to assess whether the toe is amenable to IPJ arthroplasty. If osteomyelitis extends throughout the entire proximal phalanx or both the proximal and distal phalanges, hallux amputation may be a better option. Excessive bone debridement for necrosis or digital deformity causes instability of the tip of the toe and thus does not preserve digital function or cosmetic appearance. A Schrudde Type 1 unilobed rotational flap design is used with the size of the flap being approximately 75 % of the total soft tissue defect after wound excision (Fig. 15.11c) [11]. This is typically a single-stage outpatient procedure that is performed supine without the use of a tourniquet. Staged surgery is possible with initial excision of the wound followed by debridement and biopsy of the proximal phalanx. Final bone resection and delayed flap closure of the wound is performed once cellulitis and abscess resolve. Persistent infection despite initial bone resection could always be converted to hallux amputation, especially if the soft tissues remain compromised by infection or poor circulation. Staged surgery also allows time for vascular intervention if indicated.
Sesamoidectomy with O-to-Z Flap or Bilobed Flap Closure of Plantar MPJ Ulceration
Plantar first MPJ ulcers are difficult to heal due to significant stress applied during gait. This stress is amplified in patients with diabetic peripheral neuropathy combined with certain biomechanical alterations that contribute to plantar MPJ ulcer formation. A recent study found that diabetics with peripheral neuropathy and foot ulcer formation demonstrated a significantly lower range of motion at the hips, knees, ankles, and first MPJ compared to diabetics without ulcer formation [12]. Previous studies have shown abnormally high pressure under the metatarsal heads in diabetic patients with peripheral neuropathy. Patry also reported that forefoot pressure was 2.3 times higher than rearfoot pressure in those patients [13]. These findings help explain why ulcers at this location are common and difficult to heal with propensity to progress to the point of osteomyelitis.
Chronic wounds under the first MPJ frequently develop osteomyelitis of the sesamoid bones prior to extension of infection into the MPJ and the adjacent metatarsal and proximal phalanx (Fig. 15.20). Early surgical intervention with sesamoidectomy for nonhealing or recurrent wounds can be effective to avoid partial first ray amputation which is often necessary once the joint becomes exposed. The procedure is most effective when performed early before the onset of soft tissue infection. Our typical approach is to employ standard wound healing measures until the point when the wound probes to bone, which is the primary indication for surgery. It is important to evaluate patients with chronic or recurrent plantar first MPJ ulcers for related deformities including ankle equinus, plantar displacement of the first metatarsal, or hallux hammertoe contracture. These deformities can be addressed surgically prior to onset of infection.


Fig. 15.20




Case 3: Chronic full thickness plantar neuropathic ulceration at the first metatarsophalangeal joint. Nonhealing neuropathic ulcers of the first metatarsophalangeal joint (MPJ) with persistent sesamoid bone exposure commonly results in osteomyelitis of the sesamoids, first metatarsal, or proximal phalanx. First MPJ joint sepsis is also a common sequela. Removal of the sesamoids is possible; however, this size and location of wound defect is not very amenable to primary wound closure. Leaving the plantar metatarsal head exposed after sesamoid excision will almost certainly result in bone or joint infection. Note poor quality tissue at the base of the wound. Probe to bone test was positive
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








