CHAPTER 6 ![]() Findings and pathology associated with anterior shoulder instability
Findings and pathology associated with anterior shoulder instability
 The inferior glenohumeral ligament (IGHL) is the most important capsular stabilizer of the glenohumeral joint (anterior band for anterior stability; posterior band for posterior stability).
The inferior glenohumeral ligament (IGHL) is the most important capsular stabilizer of the glenohumeral joint (anterior band for anterior stability; posterior band for posterior stability). The Bankart lesion (tear of the anterior capsulolabral structures off the glenoid) is present after nearly all anterior instability injuries and can be soft tissue only (labral tear with capsular stretch), bony (bony Bankart or anterior glenoid “fracture”), or a combination thereof.
The Bankart lesion (tear of the anterior capsulolabral structures off the glenoid) is present after nearly all anterior instability injuries and can be soft tissue only (labral tear with capsular stretch), bony (bony Bankart or anterior glenoid “fracture”), or a combination thereof. The anterior labral periosteal sleeve avulsion (ALPSA) represents a labrum that has torn off the glenoid and healed medially down the neck.
The anterior labral periosteal sleeve avulsion (ALPSA) represents a labrum that has torn off the glenoid and healed medially down the neck. The humeral avulsion of the glenohumeral ligament (HAGL) is a rarer variant of instability pathology in which the capsule is torn off the humerus.
The humeral avulsion of the glenohumeral ligament (HAGL) is a rarer variant of instability pathology in which the capsule is torn off the humerus. The glenolabral articular disruption (GLAD) lesion represents an injury to the articular surface of the glenoid, usually after a recurrent instability event.
The glenolabral articular disruption (GLAD) lesion represents an injury to the articular surface of the glenoid, usually after a recurrent instability event.Introduction
The shoulder provides the greatest range of motion of all the joints in the body. As such, it has an amazing capacity to dislocate, with the overall population incidence of 1.7%.1 Younger patients appear to have more recurrent dislocations than older patients, and patients younger than 20, may have a chance of recurrence as high as 90%.2 Unfortunately, after shoulder dislocation, injuries occur to the surrounding ligaments, labrum, capsule, and osteochondral surfaces, leading Hovelius et al to find moderate to severe arthritis in 26% of patients treated nonoperatively at 25 years.3 In this chapter, we discuss the radiographic and arthroscopic findings associated with anterior instability of the shoulder.
Anatomy and biomechanics
Figure 6-1, A demonstrates the anatomic restraints to anterior shoulder dislocation. At the periphery of the glenoid, the fibrocartilaginous labrum, and long head of the biceps deepen the socket and provide additional stability. A study by Halder et al demonstrated that resection of the glenoid labrum resulted in diminished stability to the glenohumeral joint via the concavity-compression mechanism.4 The capsule is a thin layer of fibrous tissue that contains thickenings known as the glenohumeral ligaments. The rotator interval is a triangular area of tissue whose borders are the supraspinatus anteriorly and the subscapularis inferiorly. It contains two important ligaments: the coracohumeral ligament (CHL) and the superior glenohumeral ligament (SGHL). The stronger CHL proceeds in a distal-lateral direction from the base of the coracoid, inserting on the greater and lesser tuberosities. The coracohumeral ligament contains two layers as it splits to envelop the biceps tendon and eventually proceeds to its lateral insertion site.5,6
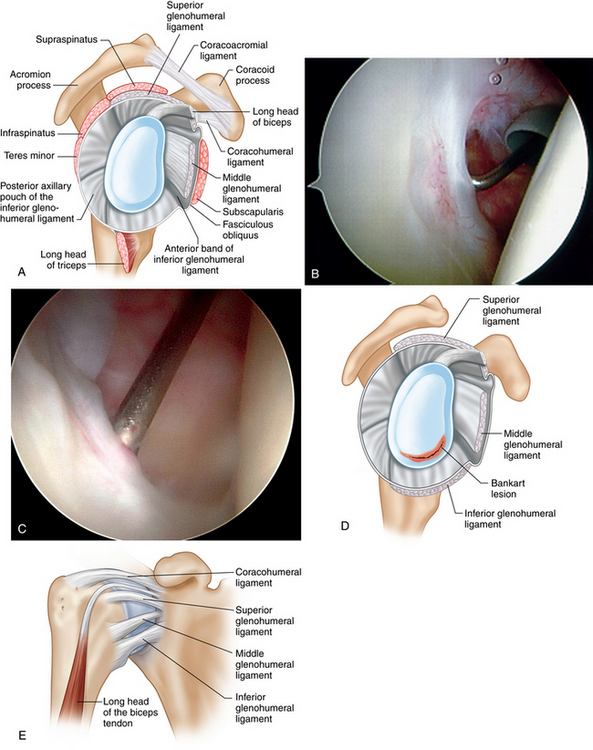
FIGURE 6-1 A, Schematic representation of the glenohumeral capsule and ligaments. B, Arthroscopic view of the middle glenohumeral ligament (MGHL) passing perpendicularly (right shoulder, beach chair position; posterior viewing portal). C, Arthroscopic view of the inferior glenohumeral ligament (IGHL) (right shoulder, beach chair position; posterior viewing portal). D, Sagittal view of the glenohumeral ligaments. E, Graphic representation of anterior ligaments of the shoulder complex.
(B and C courtesy of Center for Shoulder, Elbow and Sports Medicine, Columbia University. D from Reider B, et al: Operative techniques: Sports medicine surgery, Philadelphia, 2010, Saunders Elsevier.)
The SGHL originates from the 1 o’clock position at the supraglenoid tubercle just anterior to the biceps tendon and inserts at the tip of the greater tuberosity.6 The SGHL and joint capsule make up the deep layer of the medial rotator interval, and the superficial CHL makes up the more superficial layer. The functions of the CHL and SGHL are threefold: to provide a sling for the biceps, to limit external rotation when the arm is at the side, and to resist inferior translation of the arm in adduction. While the CHL is a consistent finding, the SGHL is absent 6% of the time.7
The middle glenohumeral ligament (MGHL) has more anatomic variation than all of the glenohumeral ligaments. Like the SGHL, it originates from the supraglenoid tubercle. Its point of origin, however, is slightly more variable than the SGHL, and can originate as far as 3 o’clock on the glenoid rim.6 Some fibers of the MGHL insert on the subscapularis muscle approximately 2 cm medial to the muscle’s insertion.8 The MGHL may be wide and thin or cordlike, and can have varying degrees of confluence with the inferior glenohumeral ligament (IGHL) (Fig. 6-1, B). The function of the MGHL is to limit external rotation of the arm with the arm in 45 degrees of abduction. The MGHL is a variable structure and can present between 65% and 85% of the time.6,7
The IGHL is the most important stabilizer of the glenohumeral joint (Fig. 6-1, C). The anterior band is the thickest and strongest of all of the capsular thickenings in the shoulder. In a study by Bigliani et al, the stress at failure of the IGHL, which is commonly injured in an anterior shoulder dislocation, is 5.5 MPa.9 The IGHL originates from the 2 o’clock to 5 o’clock position on the glenoid and labrum.7 The posterior band takes its origin between the 7 o’clock and 9 o’clock position. The anterior band is almost always present, but the posterior band is only present 60% of the time. The anterior IGHL serves as the primary static restraint to anterior instability at 90 degrees of abduction.
Because of its direct connection to the superior labrum, the long head of the biceps also may play a role in stabilizing the glenohumeral joint. A study by Rodosky et al showed that in late cocking, the long head of the biceps was found to contribute to the torsional stability of the humerus. Further, after sectioning of the long head of the biceps, the anterior/inferior structures demonstrated more strain.10 Loading of the biceps also demonstrates decreased anterior/posterior translation of the humerus.11 Therefore, it is clear that the long head of the biceps also plays a role in anterior stability.
Anatomic variants
Anatomic variants in the shoulder are common and must be recognized to prevent inadvertent repair of normal structures. One of the anatomic variants commonly found is the sublabral foramen, or sublabral hole, occurring in 12% of patients.12 A sublabral foramen occurs between the 9 and 12 o’clock positions (left shoulder) and must be distinguished from an anterosuperior labral tear. Typically, it can be recognized by its smooth transition from labrum to foramen and the absence of any trauma to the adjacent labrum, cartilage, or capsule (Fig. 6-2). A cordlike MGHL is found in 9% of patients and commonly is associated with a sublabral foramen (Fig. 6-3). Finally, a less frequently occurring anatomic variant is the Buford complex, found in 1.5% of shoulders. Williams et al first described this variant as a cordlike MGHL found concurrently with an absent anterosuperior labrum. Failure to recognize any of these normal anatomic variants will lead to inappropriate surgical repair that can result in pain and loss of external rotation.12
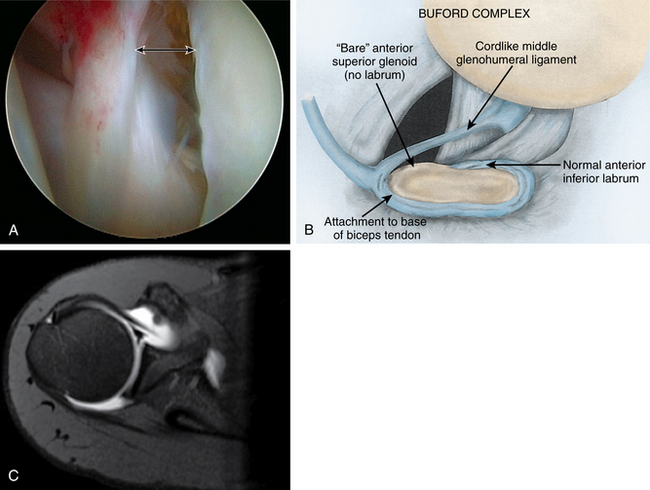
(A courtesy of Center for Shoulder, Elbow and Sports Medicine, Columbia University. B from Williams SM, et al: The Buford complex—the “cord-like” middle glenohumeral ligament and absent centrosuperior labrum: A normal anatomic capsulolabral variant. Arthroscopy 10:244–245, 1994.)
Lesions of the glenoid labrum and ligamentous attachments
Bankart lesion
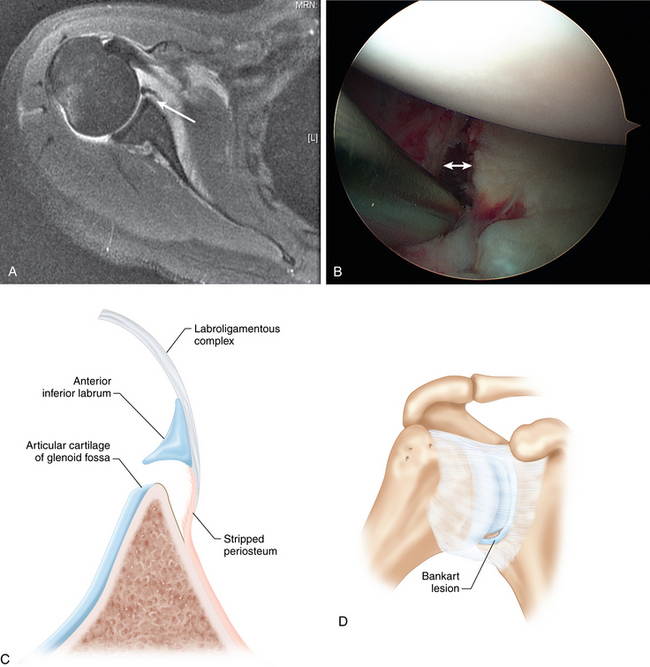
The Bankart lesion is an avulsion of the anterior labroligamentous structures from the anterior glenoid rim. Bankart described it as the “lesion of necessity” in anterior shoulder instability and believed that it occurred in 100% of all dislocations.13 Modern studies estimate that approximately 90% of all anterior dislocations have Bankart lesions.14 The anterior scapular periosteum is disrupted, and the labrum and attached ligaments are typically found anterior to the glenoid rim. Therefore, the anterior band of the inferior glenohumeral ligament or middle glenohumeral ligament cannot perform their stabilizing functions at the end ranges of motion. In addition, the labrum does not function to deepen or stabilize the glenoid socket. With the labrum removed, the force required to translate the shoulder anteriorly is reduced by 50%.15
After appropriate history and physical examination, magnetic resonance imaging (MRI) with intra-articular gadolinium is often obtained to confirm the pathologic findings. The Bankart lesion is usually found on the axial cut of the MRI, in the anteroinferior aspect of the glenoid. Gadolinium is visualized between the anterior labrum and glenoid (Fig. 6-4, A).
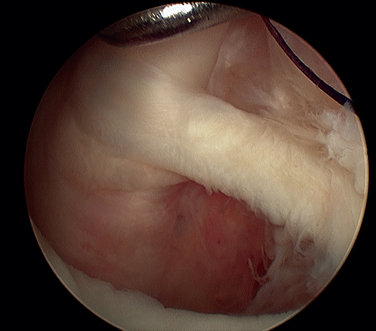
During arthroscopic evaluation, an abnormal separation between the labrum and glenoid is often present (Fig. 6-4, B). There will occasionally be hemorrhage signifying injury, but because of the poor vascularity of the glenoid, this is not a reliable finding. A probe can be used to identify the labral tear, confirming the preoperative examination and imaging studies.
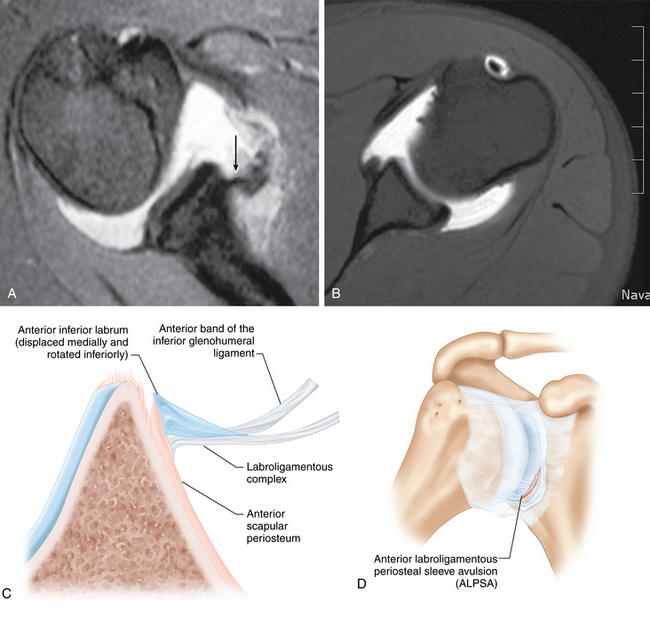
Anterior labroligamentous periosteal sleeve avulsion (ALPSA)
Neviaser first described the ALPSA lesion in 1993.15a The labroligamentous complex heals medially on the glenoid neck allowing for recurrent anterior instability due to the incompetent anterior IGHL. In contrast, the Bankart lesion contains a rupture of the scapular periosteum, and the injured tissue stays at the level of the glenoid surface. Recent reports have suggested that ALPSA lesions do not usually occur with first time dislocations. Habermeyer et al described a “time-dependent” and “recurrence-dependent” etiology for the evolution of the ALPSA lesion.16 Another recent study suggested that almost all ALPSA lesions were found to exist in shoulders with chronic dislocations.17
The ALPSA lesion is best identified with a contrast-enhanced MRI (Fig. 6-5). After an acute injury, the anterior glenoid periosteum is stripped down to the neck of the glenoid, and contrast fills this space. In a chronic situation, the anterior scapular periosteum and labroligamentous structures are found in a ball or heap on the scapular neck.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree