Fillet Flaps in Cases of Mutilating Trauma
Bradley Medling
Michael W. Neumeister
Fillet flaps can be a very important reconstructive option in many cases of hand and lower limb trauma. Fillet flaps are, by definition, axial flaps that may provide skin, muscle, fascia, and bone. They can be harvested either as a pedicled flap or as a free flap. Careful a planning and execution of the flaps can allow for reconstruction of local defects with a flap of a similar tissue type. This technique takes advantage of spare parts that would otherwise be discarded, avoiding associated morbidity of a separate flap harvest.
Fillet flaps are most commonly employed after mutilating trauma to the hand. The concept of spare parts surgery should be broadly applied to include any tissue that would otherwise be discarded; these flaps may include bone, nerve, tendon, joints, or the whole digit. Segments of the injured part can be harvested with their blood supply intact, and thereby be used as a vascularized tissue graft or flap.
Frequently, a traumatized extremity is left without soft tissue coverage, leaving exposed vital structures such as bone, joint, tendon, or neurovascular bundles. Vascularized coverage can be salvaged from attached parts of the mangled hand that are otherwise rendered dysfunctional or from amputated parts where a flap is designed over a preserved vascular bundle.
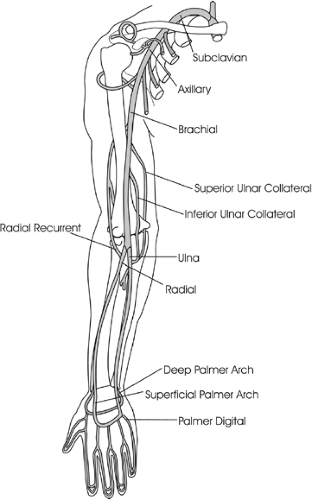
The key component to the safe harvest of a fillet flap is an understanding of the vascular supply to tissue. Since the entire upper extremity and lower extremity can be used in a fillet fashion, the blood supply to the arm and leg must be understood. In the upper extremity, the axillary artery terminates at the lateral border of the pectoralis minor muscle becoming a brachial artery to a point just distal to the antecubital fossa. The brachial artery runs in the medial upper arm in relative proximity to the ulnar and median nerve. At the level of the elbow, the brachial artery is lateral to the median nerve. The brachial artery bifurcates into the radial and ulnar arteries, respectively, under the superficial flexor muscles of the forearm. The radial artery travels under the flexor carpi radialis muscle exiting more superficial in the forearm just lateral to the tendon of the flexor carpi radialis. The ulnar artery travels with the ulnar nerve under the muscle belly of the flexor carpi ulnaris becoming more superficial in the distal forearm. The ulnar artery travels through Guyon’s canal and bifurcates into a superficial and deep branch, each of which communicates with the radial artery component of the superficial and deep palmar arches. The radial artery bifurcates at the wrist into a superficial palmar and deep dorsal branch. The superficial palmar branch courses around the base of the thenar eminence, and the larger deep branch travels under the abductor pollicis longus, extensor pollicis brevis, and the extensor pollicis longus, through the anatomical snuffbox. It then courses between the first and second metacarpals, through the adductor space to form the radial component of the superficial and deep palmar arches. The common digital vessels arise from the superficial palmar arch and travel to the level of the metacarpophalangeal joint, where these vessels now bifurcate to become the digital vessels proper (Fig. 17-1).
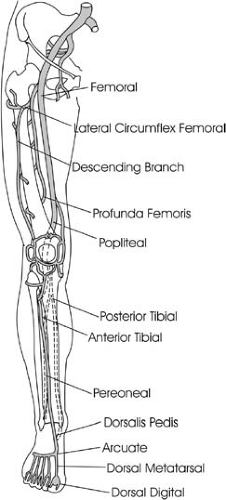
In the lower extremity, the superficial femoral and the profunda femoral vessels may be used as arterial inflow for fillet flaps of the thigh. The superficial femoral vessels continue distally to form the
popliteal artery, which bifurcates in the popliteal fossa to the anterior tibial and posterior tibial arteries. The posterior tibial artery subsequently bifurcates to become the posterior tibial artery and the peroneal artery. The anterior tibial artery travels in the anterior compartment above the interosseous membrane, becoming more superficial as it approaches the extensor retinaculum of the ankle. At this point, this vessel becomes the dorsalis pedis artery, which travels between the first and second metatarsal to the foot. The superficial arcuate branch provides arterial inflow to the dorsum of the foot, while the deep branch pierces between the first and second metatarsal to form the plantar vascular arch. The common digital vessels arise from this arch, and bifurcate at the metatarsal-phalangeal joints to become the digital vessels to the toes. The peroneal artery travels beside the medial aspect of the fibula and terminates as the lateral calcaneal artery behind the lateral malleolus. The poster tibial artery travels in the poster compartment of the lower leg and exits superficial behind the medial malleolus and subsequently bifurcates into the medial and lateral plantar vessels (Fig. 17-2).
popliteal artery, which bifurcates in the popliteal fossa to the anterior tibial and posterior tibial arteries. The posterior tibial artery subsequently bifurcates to become the posterior tibial artery and the peroneal artery. The anterior tibial artery travels in the anterior compartment above the interosseous membrane, becoming more superficial as it approaches the extensor retinaculum of the ankle. At this point, this vessel becomes the dorsalis pedis artery, which travels between the first and second metatarsal to the foot. The superficial arcuate branch provides arterial inflow to the dorsum of the foot, while the deep branch pierces between the first and second metatarsal to form the plantar vascular arch. The common digital vessels arise from this arch, and bifurcate at the metatarsal-phalangeal joints to become the digital vessels to the toes. The peroneal artery travels beside the medial aspect of the fibula and terminates as the lateral calcaneal artery behind the lateral malleolus. The poster tibial artery travels in the poster compartment of the lower leg and exits superficial behind the medial malleolus and subsequently bifurcates into the medial and lateral plantar vessels (Fig. 17-2).
Indications/Contraindications
Before harvesting a fillet flap for soft tissue coverage, the surgeon should identify the ultimate goal of the immediate and delayed reconstructive procedures. Decisions may be less complex for some lower extremity trauma, where discarding the mutilating limb may be in the best interest of the patient from a functional point of view. Prostheses may be much more functional than attempts at salvage where stability and sensation are compromised. Conversely, mangled hands can have significant function if pinch and grasp can be restored. Reconstructive efforts may be turned toward
salvaging fingers or the thumb, rather than using their tissue as spare parts for soft tissue coverage for the remaining injured hand. The ability to restore some sensate function is a key component of the hand’s role in activities of daily living. This separates the overall treatment protocols and goals of upper extremity reconstruction from that of lower extremity reconstruction (Fig. 17-3). The reconstruction process is dictated by the complexity and level of injury. Nerve regeneration, tendon and bone reconstruction, and secondary toe to hand procedures are alternatives to amputation of digits or hands and permit acceptable restoration of function. In both upper and lower extremity, however, there are opportunities that arise to use tissue that would otherwise be discarded, for definitive soft tissue closure.
salvaging fingers or the thumb, rather than using their tissue as spare parts for soft tissue coverage for the remaining injured hand. The ability to restore some sensate function is a key component of the hand’s role in activities of daily living. This separates the overall treatment protocols and goals of upper extremity reconstruction from that of lower extremity reconstruction (Fig. 17-3). The reconstruction process is dictated by the complexity and level of injury. Nerve regeneration, tendon and bone reconstruction, and secondary toe to hand procedures are alternatives to amputation of digits or hands and permit acceptable restoration of function. In both upper and lower extremity, however, there are opportunities that arise to use tissue that would otherwise be discarded, for definitive soft tissue closure.
The availability of adequate tissue often depends on the mechanism of injury to a limb. Clean guillotine lacerations or amputations, with minimal tissue loss, offer the best results at restoration of function. Fortunately, most of these injuries do not mandate that need of spare parts or fillet flaps due to the lack of soft tissue deficits. More traumatic injuries, such as crush and avulsion injuries, or electrical burns, require greater debridement and have more tissue loss. Consequently, these injuries frequently take advantage of spare parts and fillet flap surgery for coverage.
Pedicle or free tissue fillet flaps can be used for proximal amputations that require stable coverage to better preserve function, such as elbow flexion or knee mobility. This technique is usually indicated for amputations with significant proximal tissue loss and where there is a contraindication for replantation. The remaining distal tissue is filleted, based on one neurovascular bundle, and transferred to cover the proximal exposed structures as a free tissue transfer. If there is an intact neurovascular bundle, but with segmental intervening loss of tissue in the limb, the fillet flap can be harvested as a pedicle flap, leaving the vessels and nerves intact. Indications for fillet flaps are included in Table 17-1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree