Fig. 18.1
Flow diagram to assist with procedure selection for infected fifth ray ulcerations with suspicion of osteomyelitis. Ideal procedure selection for fifth ray osteomyelitis is based on underlying deformity, location of the ulceration, and extent of osteomyelitis. Consideration is also given to circulation and the quality of the surrounding soft tissues which may be necrotic from gangrene or infection
Ulceration and Osteomyelitis of the Fifth Toe
Partial fifth ray amputation is common for fifth ray osteomyelitis but early intervention with traditional podiatric reconstructive procedures can also be effective at achieving the surgical goals while avoiding amputation. A study by Faglia demonstrated that internal pedal amputations, such as phalanx and metatarsal head resection, is a feasible alternative to ray or toe amputation when appropriate [1]. Osteomyelitis of the fifth toe is generally associated with contiguous spread of infection from adjacent ulceration or gangrene. In the absence of an open wound, the clinician should look for other causes of suspicious radiographic finding including gout, trauma, or degenerative arthritis. Fifth toe ulcers are typically caused by repetitive pressure over prominent bone associated with hammertoe deformity, bone spurs, heloma molle, and arthritis (Fig. 18.2). Neuropathy plays a large but not exclusive role as many of these wounds are chronically painful. Hammertoe deformity or exostosis can lead to prominent bone at the interphalangeal joints (IPJ), which can cause a sinus tract or ulceration leading to osteomyelitis. In general, partial toe amputation, distal Syme’s amputation, and metatarsophalangeal joint (MPJ) disarticulation are less common on the fifth toe compared to the other toes due to concern for continued lateral prominence that would lead to shoe rubbing and future wound breakdown.


Fig. 18.2
Conditions leading to fifth toe osteomyelitis. (a) Neuropathic ulcers overlying the fifth proximal interphalangeal joint (PIPJ) are a common cause of fifth toe osteomyelitis. (b) Structural deformities like overlapping or underlapping digital deformities, hammertoe contracture, DJD, and malunited fractures predispose to tissue breakdown and nonhealing wounds on the medial, lateral, and dorsal aspects of the PIPJ. (c) Contiguous spread of infection from digital gangrene is also common
Proximal Interphalangeal Joint Arthroplasty
Fifth toe PIPJ arthroplasty is useful for dorsal, lateral, and medial PIPJ ulcerations associated with osteomyelitis that is isolated to the head of the proximal phalanx. This conservative surgical approach can effectively treat osteomyelitis of the head of the proximal phalanx by excising the wound and infected bone as well as correcting digital deformity which further reduces the risk of recurrent ulceration. The standard PIPJ arthroplasty technique can be utilized with a dorsal linear approach, but a modified ulcer excision plan is best for cases involving ulceration (Fig. 18.3). Prophylactic PIPJ arthroplasty prior to the onset of osteomyelitis is useful for nonhealing or recurrent PIPJ wounds. Resection of the head of the proximal phalanx also provides a specimen for bone biopsy and relaxes the surrounding tissues to allow primary closure of small wound defects.
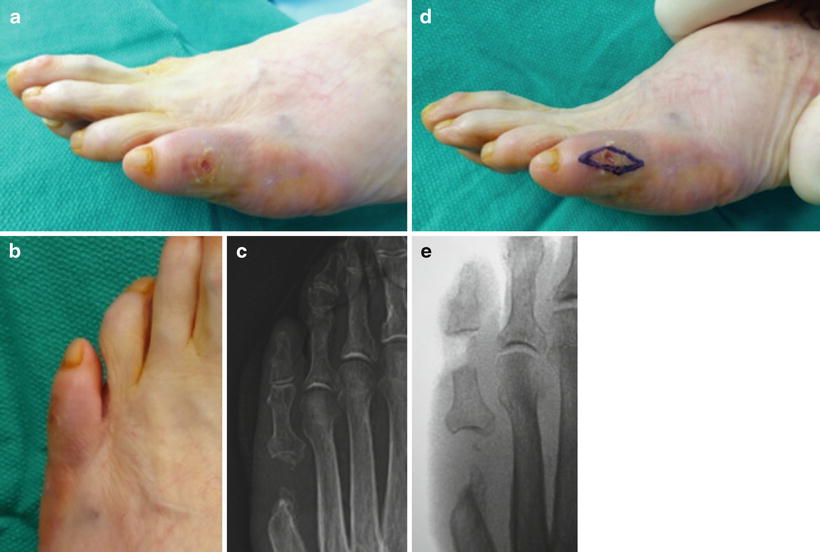
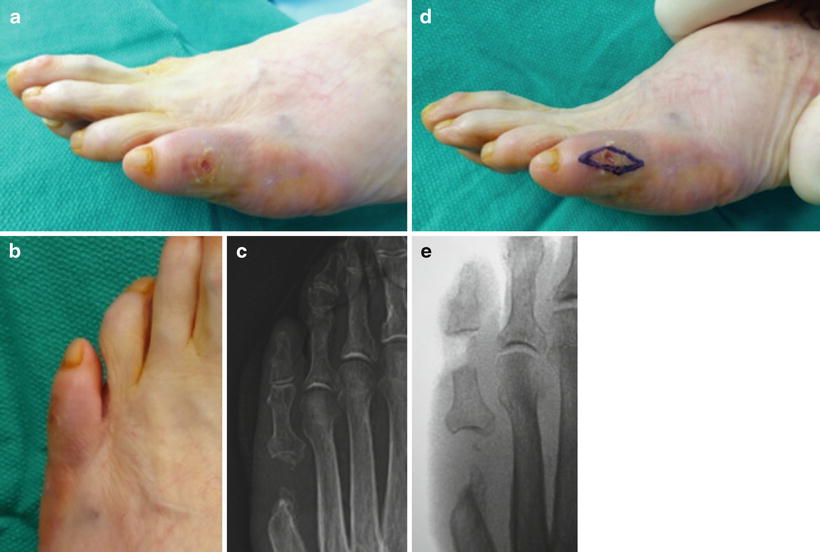
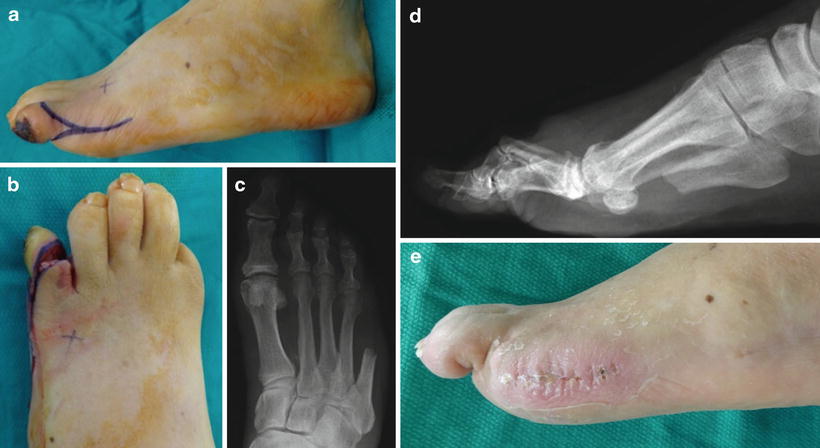
Fig. 18.3
Fifth toe arthroplasty for infected proximal interphalangeal joint ulcer. (a–c) Early intervention for a painful wound with recurring cellulitis, positive probe to bone test, and relatively normal X-ray findings allowed arthroplasty instead of amputation for osteomyelitis. The patient had prior fifth metatarsal head resection for similar wound complications. (d, e) Elliptical excision of the ulcer and arthroplasty of the proximal interphalangeal joint allowed primary closure of the chronic wound. Removal of the head of the proximal phalanx eliminated the prominent bone and provided specimen for biopsy
Fourth and Fifth Digital Syndactylization
Syndactylization of the fourth and fifth toes is useful for persistent interdigital ulcers and ulcerated deep interspace heloma molle (Fig. 18.4). This is a cosmetically appealing alternative to amputation allowing concomitant wound excision, PIPJ arthroplasty, and primary wound closure. Another indication for syndactylization is fifth digital instability after arthroplasty requiring excessive bone loss. Wide resection of the proximal phalanx increases the chance of a flail toe without proper stabilization. The goal of partial syndactylization is to preserve a more normal toe appearance yet remove abnormal tissue deep in the interdigital space. A transverse elliptical incision extends along the bases of the fourth and fifth toes which removes both the ulcer and macerated tissue between the toes (Fig. 18.5). This approach allows direct access to the head of the proximal phalanx, which is resected with a bone-cutting forceps. The lateral aspect of the fourth toe and medial aspect of the fifth toe are then approximated closing the interdigital wound primarily. Suture removal may be difficult in the interdigital space making absorbable sutures ideal (Fig. 18.6).
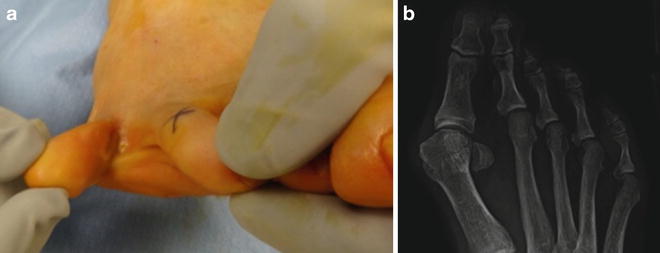


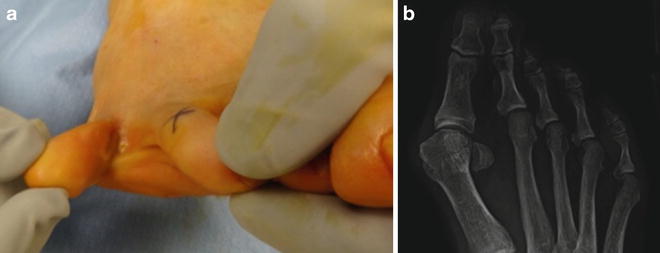
Fig. 18.4
Partial syndactylization and fifth proximal interphalangeal joint (PIPJ) arthroplasty for interdigital ulceration complicated by osteomyelitis. (a) Fourth interspace chronic callus predisposed to periodic interdigital ulceration resulting in fifth toe osteomyelitis and PIPJ sepsis. The tissue deep in the interdigital space is commonly abnormal with maceration and scar tissue formation from longstanding heloma molle. (b) Preoperative X-ray demonstrated pressure of the head of the fifth proximal phalanx on the fourth metatarsal head. Early intervention with a reconstructive approach prior to tissue necrosis allowed excision of the ulcer, resection of the head of the fifth proximal phalanx, and partial syndactylization of the fourth and fifth toes

Fig. 18.5
Partial syndactylization technique. (a) The partial syndactylization technique confines interdigital wound excision to the deep aspect of the interdigital space with the intent to preserve more normal looking toes as compared to complete syndactylization. The wound was excised with careful attention to preserve the dorsal and plantar digital neurovascular structures. (b) Disarticulation of the fifth proximal interphalangeal joint provided exposure for arthroplasty. (c) The head of the proximal phalanx was removed which served as biopsy specimen and also reduced pressure on the fourth metatarsal head

Fig. 18.6
Clinical results after partial syndactylization. Two week postoperative clinical appearance after partial syndactylization and proximal interphalangeal joint arthroplasty. Suture removal may be difficult in the interdigital space making absorbable sutures beneficial. Note how the fourth and fifth toes look relatively normal despite lack of the deep interdigital space. Early intervention allowed early diagnosis of osteomyelitis which in turn translated to minimally invasive treatment. This procedure also eliminated the chronic interdigital corn and ulcer that was painful
Fifth Toe Amputation
Osteomyelitis that encompasses the entire proximal phalanx or involves both the proximal and middle phalanges is ideally treated with complete fifth toe or partial fifth ray amputation (Fig. 18.7). The majority of patients with osteomyelitis of the fifth toe are treated with fifth ray amputation despite the fifth metatarsal being uninvolved. Leaving the fifth metatarsal head may predispose to plantar or lateral prominence and recurrent ulceration depending on bone structure. Removal of the metatarsal head also creates laxity in the soft tissues allowing primary closure of extensive soft tissue defects. One unique approach to preserve the metatarsal head involves a trap door digital fillet flap that utilizes intact dorsal tissue to cover a plantar defect or lateral tissue to cover an interspace defect (Figs. 18.8, 18.9, 18.10, and 18.11).



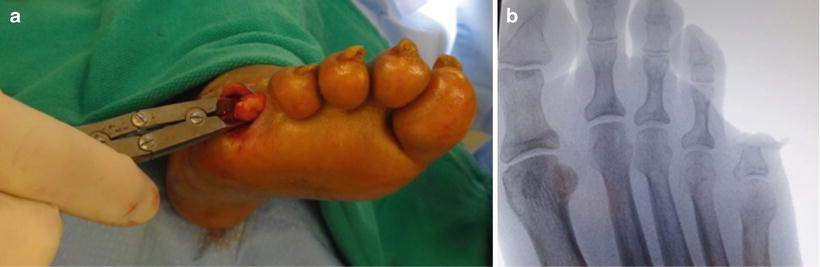


Fig. 18.7
Fifth toe amputation. (a, b) Proximal interphalangeal joint osteomyelitis involving both the middle and proximal phalanges is typically treated with complete fifth toe or partial fifth ray amputation. (c, d) A standard tennis racket incision with dorsal and plantar flaps was utilized for the amputation. (e, f) Note that the lateral head of the fifth metatarsal was remodeled which provided clean margin biopsy and reduced lateral prominence. (g) Primary wound closure with simple sutures allowed prompt healing with resolution of infection 5 days later. Confirmation of a clean bone margin allowed a short course of oral antibiotics

Fig. 18.8
Isolated fifth toe amputation with dorsal trap door digital fillet flap. (a–d) Digital gangrene commonly results in soft tissue infection and eventually osteomyelitis. Full thickness gangrene compromised the plantar tissue making primary closure with isolated fifth toe or fifth ray amputation challenging. Note that the dorsal tissue is not gangrenous but is compromised by infection and vascular insufficiency

Fig. 18.9
Trap door digital fillet flap technique. (a, b) A fishmouth type incision was made around the infected and gangrenous tissue. The dorsal flap of tissue was preserved to allow primary closure with fifth toe amputation. Note how the dorsal flap technique does not allow easy access for fifth metatarsal head resection although the lateral apex of the incision (b) could be extended proximally. (c) The flap was raised full thickness off the proximal phalanx to preserve flap viability
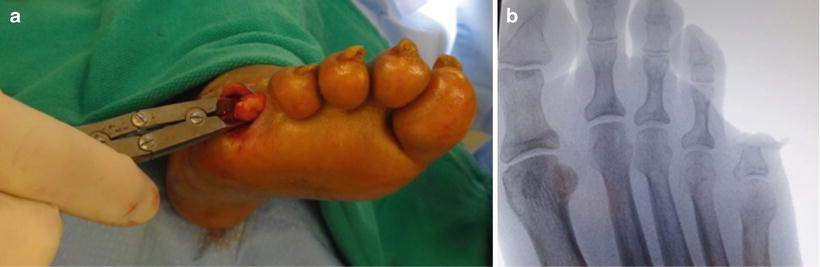
Fig. 18.10
Bone resection for partial fifth toe amputation. (a, b) Toe amputation was performed through the base of the proximal phalanx. Ray amputation is typically at the neck of the fifth metatarsal although partial or complete fifth toe amputation is an option under special circumstances including gangrene. This patient had compromised vascularity and poor health status which lead to this “less is more” approach. There is potential for shoe pressure along the lateral aspect of the fifth digital stump

Fig. 18.11
Healed trap door digital fillet flap. (a) The trap door flap was closed to cover the soft tissue defect. Note that the compromised plantar tissue was entirely unavailable for contribution to wound coverage which necessitated this advanced plastic surgical technique. (b, c) Healing of the trap door flap at 6 weeks without recurrent soft tissue or bone infection
Fifth Metatarsal Phalangeal Joint Ulceration and Osteomyelitis
Infection around the fifth MPJ is most commonly associated with plantar or lateral fifth metatarsal head neuropathic ulceration but also occurs due to soft tissue infection spreading proximally from the fifth toe wounds or gangrene. Partial fifth ray amputation is a common surgical treatment option while complete fifth ray amputation is avoided when possible. A variety of incision plans including flap closure are available and are dictated by the size and location of the wound defect.
Fifth Metatarsal Head Resection
Early diagnosis of fifth metatarsal head osteomyelitis or early intervention for nonhealing or recurrent neuropathic ulceration can be treated with isolated fifth metatarsal head resection (Fig. 18.12). This internal offloading technique allows plantar or lateral wounds to heal promptly and minimizes the chance of recurrence. Armstrong demonstrated that patients who received a fifth metatarsal head resection to treat plantar ulcerations had a lower reulceration rate as compared to those in a conservative treatment group [2]. There is risk of transfer ulceration to the fourth metatarsal head, but in our experience, this appears to be less common after fifth metatarsal head resection as compared to isolated removal of other metatarsal heads.


Fig. 18.12
Fifth metatarsal head resection. (a–c) Tailor’s bunion deformity predisposed to neuropathic ulceration over the lateral aspect of the fifth metatarsal head. Early intervention at the first sign of local cellulitis and bone exposure allowed fifth metatarsal head resection rather than partial ray amputation. (d, e) Elliptical excision of the ulcer with proximal runout allowed exposure for metatarsal head resection. (f) Resection of the metatarsal head not only removed the bony prominence, but allowed for bone biopsy and (g) primary wound closure
Traditional Partial Fifth Ray Amputation
The traditional approach to partial fifth ray amputation involves a standard tennis racket incision consisting of dorsal and plantar soft tissue flaps with midline proximal extension along the lateral border of the foot (Fig. 18.13). This incision approach works well for fifth toe infection and for lateral metatarsal head ulceration, since the ulceration is located within the tissue to be excised. A partial thickness plantar ulceration is also amenable to this approach since the wound should heal secondarily once the infected and prominent metatarsal head is removed. Traditional dorsal and plantar flaps are also easily converted to a transmetatarsal amputation (TMA) if necessary. Extensive tissue loss or full thickness plantar ulcerations typically require alternative incision techniques which are discussed next.