Chapter 40 Fibular Collateral Ligament and the Posterolateral Corner
Although less commonly injured than the cruciate ligaments or the medial knee ligament complex, injuries to the fibular collateral ligament and posterolateral corner comprise a significant portion of knee ligament injuries.25 Associated posterolateral corner injuries provide a potential source of residual instability following anterior cruciate ligament and posterior cruciate ligament reconstruction and can lead to reconstruction graft failure.10,21,22 A high index of suspicion is necessary when initially evaluating the injured knee to detect these sometimes occult injuries. Furthermore, a diligent physical examination and comprehensive review of radiographic studies is necessary to identify these injuries. We will provide a review of the anatomy and clinically relevant biomechanics of the fibular collateral ligament and posterolateral corner. We will then present nonoperative and operative treatment options, as well as the postoperative rehabilitative protocol and potential complications.
Anatomy
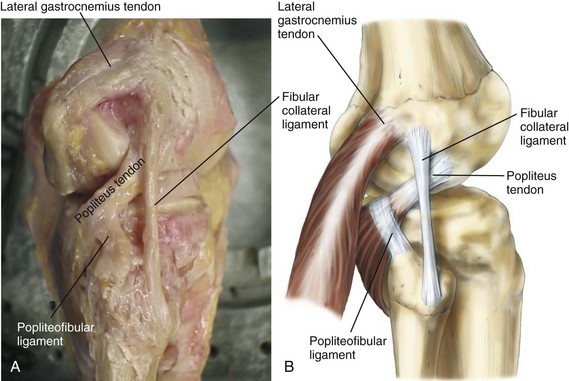
An understanding of the complex anatomy of the lateral aspect of the knee is required prior to performing a physical examination, reviewing the radiographic images, or embarking on a complex reconstruction. We will review the major components of the lateral knee ligament complex, as well as their insertions and actions (Fig. 40-1).
Fibular Collateral Ligament
The fibular collateral ligament is the primary stabilizer to varus stress of the knee.7,8,24 The femoral attachment of the fibular collateral ligament (FCL) is in a small bony depression 1.4 mm proximal and 3.1 mm posterior to the lateral epicondyle.19 At its femoral origin, the cross-section of the FCL is 0.48 cm2. As the FCL travels distally to its attachment on the fibular head, the cross-sectional area decreases slightly to 0.43 cm2. The FCL fibular attachment site is 8.2 mm posterior to the anterior margin of the fibular head and 28.4 mm distal to the tip of the fibular styloid. The FCL occupies 38% of the width of the fibular head at its attachment; the average length of the FCL is 69.6 mm.
Popliteus Tendon
The popliteus muscle courses proximally and laterally from its distal insertion on the posteromedial tibia. It becomes tendinous in the lateral third of the popliteal fossa and becomes intra-articular as it courses deep to the FCL. The cross-section of the popliteus tendon at its femoral insertion is 0.59 cm2.19 Its proximal insertion is along the proximal half of the popliteal sulcus and is always anterior (18.5 mm) to the insertion of the FCL femoral attachment (Fig. 40-2). The tendinous portion of the popliteus is approximately 55 mm in length.
Popliteofibular Ligament
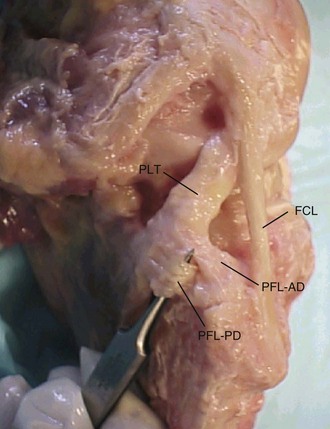
The popliteofibular ligament originates from the musculotendinous junction of the popliteus muscle and inserts onto the fibular styloid. It has two divisions (Fig. 40-3), anterior and posterior; the posterior division is larger at its fibular attachment site (3 vs. 6 mm, respectively).19 The popliteofibular ligament provides an important restraint to external rotation.24
Lateral Gastrocnemius Tendon and Fabellofibular Ligament
The lateral gastrocnemius tendon originates along the supracondylar process of the distal femur (see Fig. 40-1). This attachment averages 13.8 mm posterior to the femoral attachment site of the FCL.19 Because it is less frequently injured than the other structures of the posterolateral knee, it can be an important landmark during surgical reconstruction. As the lateral gastrocnemius tendon courses distally, it becomes inseparable from the lateral capsule, just proximal to the fabella. The fabella (Latin for “little bean”) is a sesamoid bone that is found within the lateral gastrocnemius tendon in 30% of individuals.11 If not fully ossified, a cartilaginous analogue is frequently found up to 66% of the time. The fabellofibular ligament is a thickening of collagen that extends in a vertical orientation from the fibular styloid to the fabella. It is the distal edge of the capsular arm of the short head of the biceps femoris. It courses between the biceps tendon and gastrocnemius tendon.
Biceps Femoris Tendon: Long and Short Heads
The two heads of the biceps tendon also provide important stabilization of the lateral knee complex. The main tendon of the long head of the biceps femoris divides approximately 1 cm proximal to the fibular head into direct and anterior arms.19 The direct arm inserts onto the posterolateral fibular head and is the more important of the two. The anterior arm has a small insertion site on the more distal and anterior fibular head before most of the tendon continues on as a broad fascial aponeurosis over the anterior compartment of the leg. The anterior arm forms a bursa as it passes superficial to the fibular collateral ligament and the interval between the direct arm and the anterior arm, which provides a crucial access point to the FCL during reconstruction. The long head of the biceps tendon is also an important anatomic landmark for identification of the peroneal nerve, which lies just to its posterior (Fig. 40-4).
Iliotibial Band
The iliotibial band is the most superficial of the layers of the lateral aspect of the knee. Its broad superficial layer is the first structure encountered deep to the subcutaneous tissues and covers a significant portion of the lateral knee (see Fig. 40-4). Its insertion is at Gerdy’s tubercle, along the anterolateral aspect of the tibia. The other components of the iliotibial band include an anterior expansion known as the iliopatellar band, a deep layer that blends with the lateral intermuscular septum, and a capsulo-osseous layer that attaches to the tibia just posterior and proximal to the main attachment at Gerdy’s tubercle.33
Clinically Relevant Biomechanics of the Posterolateral Knee
The structures of the lateral knee and posterolateral corner provide the primary restraint to varus stress of the knee,7,8 as well as posterolateral rotation of the tibia in relationship to the femur.24 These structures are also important secondary stabilizers to anterior and posterior tibial translation when the cruciate ligaments are torn.13 We will next review these static and dynamic stabilizers in regard to the stresses experienced by the knee.
Varus Stress
The fibular collateral ligament is the primary restraint to varus stress across the knee. Cutting studies have demonstrated that selective sectioning of the FCL results in an increase in varus opening.7,8 In cutting series in which the FCL remains intact, varus stability has been preserved. The popliteus, popliteofibular ligament (PFL), iliotibial band, lateral gastrocnemius tendon, and short and long heads of the biceps tendon, as well as the cruciate ligaments, are secondary restraints to varus force; their contribution has been noted after sectioning of the FCL.13
External Tibial Rotation
The FCL and popliteus complex are the primary restraints to tibial external rotation.24 With sectioning of the FCL, popliteofibular ligament, and popliteus tendon, an increase in tibial external rotation has been shown in a number of studies; it is most prevalent at approximately 30 to 40 degrees of knee flexion.30
Just as the FCL and popliteus complex act as a secondary restraint to the posterior cruciate ligament (PCL) in resisting posterior tibial translation, the PCL acts as a secondary restraint to prevent external rotation of the tibia on the femur.13 Because of this relationship, combined posterior cruciate ligament and posterolateral corner injuries are particularly unstable to external rotation forces.
Anterior Tibial Translation
The ACL is the primary restraint to anterior tibial translation.34 In knees with an intact ACL, the lateral ligament complex does not provide significant restraint to anterior tibial translation. However, in an ACL-deficient knee, the structures of the posterolateral corner provide an important secondary anterior translation stabilization role.22 This is particularly true during the first 40 degrees of knee flexion.
Posterior Tibial Translation
The PCL is the primary restraint to posterior tibial translation, but the structures of the posterolateral corner (PLC) also play a primary role in preventing posterior translation of the tibia on the femur.7 This contribution is noted most in full extension and at lower degrees of flexion.8,34 The contribution of the PLC increases in the PCL-deficient knee, in which the popliteus tendon appears to contribute the most to secondary stability of the structures of the PLC.9
Injuries to the Fibular Collateral Ligament and Posterolateral Corner
Mechanism of Injury
A direct blow to the medial (particularly the anteromedial) knee is a common mechanism of injury to the FCL and PLC, although noncontact hyperextension and noncontact varus stress injuries have also been well described.23 Only 40% of PLC injuries are sports-related.30 Motor vehicle accidents, falls, and other high-energy trauma comprise a significant portion of these injuries. Usually, injuries to the PLC are associated with ACL or PCL tears because only approximately 25% of PLC injuries are isolated knee ligament tears.15,25
History and Physical Examination
Common symptoms include pain, subjective side to side instability (near extension), difficulty with stairs, difficulty on uneven ground, swelling, and ecchymoses. A varus thrust gait can be noted by the patient and physician. Patients may also report parasthesias in the peroneal nerve distribution, as well as a footdrop. It has been reported that common peroneal nerve injury can be seen in up to one third of posterolateral corner injuries.23,34
A detailed physical examination is an important and required component of a patient’s evaluation. A patient’s gait should be examined to assess for evidence of a varus thrust with the initiation of the stance phase.6 The alignment of the limbs should be evaluated and the skin examined for any evidence of penetrating trauma, open wounds, or ecchymoses. A detailed neurovascular examination with diligent recording of distal pulses, as well as muscle grading of ankle dorsiflexion, plantar flexion, inversion, and eversion strength, is also completed. Sensory examination of the distal extremity is performed with attention to the dorsum of the foot, which is supplied by the superficial peroneal nerve, and to the first web space, which is supplied by the deep peroneal nerve.
Varus Stress Test
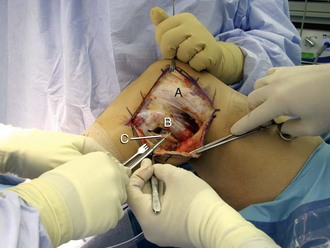
With the knee in full extension and at 30 degrees of flexion, the femur is stabilized to the examination table with the examiner’s hand (Fig. 40-5). A varus force is applied through the patient’s foot or ankle. The lateral knee joint line is palpated by the examiner’s finger (from the hand that is stabilizing the knee) and the amount of lateral compartment gapping is assessed. All stability examinations should be graded on amount of opening (as compared with the contralateral side) and firmness of the end point. Opening of the lateral compartment with the knee flexed to 30 degrees requires an injury to the FCL and possibly the secondary stabilizers of the PLC. The knee is then brought up to full extension; if the stability is restored, an isolated injury to the FCL and PLC is presumed. If the varus instability persists in full extension, a combined FCL and PLC and cruciate ligament injury is presumed.
Dial Test
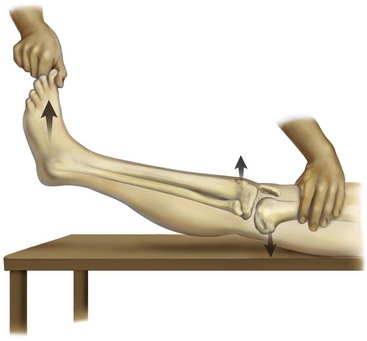
The dial test measures external rotation of the tibia in regard to the femur. The test is performed in the prone or supine position. The femur is fixed with one hand while the ankle and foot are externally rotated (Fig. 40-6). This is done with the knee flexed to 30 degrees. An increase of more than 10 degrees of external rotation compared with the uninvolved side suggests an injury to the PLC.8 The knee is then flexed to 90 degrees. Because of its role as an important secondary stabilizer, a knee with an intact PCL will see a decrease in external rotation. If, at 90 degrees, there is an increase in external rotation, as compared with 30 degrees, a combined PLC and PCL injury is presumed. A sequential sectioning study by Bae and coworkers2 have demonstrated increased external rotation following sectioning of at least three ligaments of the PCL and PLC. It was cautioned that the dial test may not be sufficiently sensitive to identify one- or two-ligament injuries.
External Rotation Recurvatum Test
In the external rotation recurvatum test, the patient is placed supine, with the knees and hips extended. The great toe is grasped and the leg lifted from the table with gentle pressure applied to the proximal knee (Fig. 40-7). The height of the heel in centimeters or degrees of hyperextension of the knee is recorded and compared with the contralateral side. A wide variation of the sensitivity of this test has been reported. Recently, LaPrade and colleagues18 evaluated this test and found it to identify less than 10% of a series of 134 patients with posterolateral corner injuries. However, in their study, a positive external rotation recurvatum test predicted a combined anterior cruciate ligament and posterolateral corner injury.
Reverse Pivot Shift
The reverse pivot shift is performed by positioning the patient supine with the knee flexed to almost 90 degrees. A valgus load is applied across the knees and an external rotation force applied to the tibia. The knee is then slowly extended. Reduction of the previously subluxated lateral tibial plateau at approximately 35 to 40 degrees of flexion is a positive result. A positive reverse pivot shift and injuries to the PLC have been correlated.30 It is important to compare the results with the contralateral knee because the test has been reported to be positive in 35% of normal knees.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree