Femoroacetabular Impingement
Thomas J.W. Byrd
Surgical correction of various hip impingement problems was described even early in the last century (1, 2). In 1975, Harris and coauthors (3) described the “pistol grip” deformity of the femoral head observed in association with early age-onset osteoarthritis. In 1998, we described arthroscopic correction of impingement due to posttraumatic osteophytes and have also reported an arthroscopic technique of cheilectomy for femoral protuberances associated with Perthes disease (4, 5). However, it was Ganz and colleagues who formulated the concept of femoroacetabular impingement (FAI) describing pincer, cam, and combined types (6, 7 and 8). Subsequently, we and other authors have reported arthroscopic methods for correcting this disorder (9, 10, 11, 12 and 13).
FAI is not a cause of hip pain. It is simply a morphologic variant that predisposes the joint to intra-articular pathology that then becomes symptomatic. The arthroscope can be instrumental in assessing this associated intra-articular damage, which aids in establishing the correct treatment algorithm and can include arthroscopic correction of the impingement when necessary.
PATHOMECHANICS
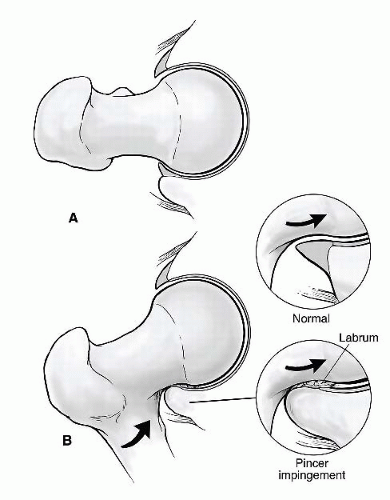
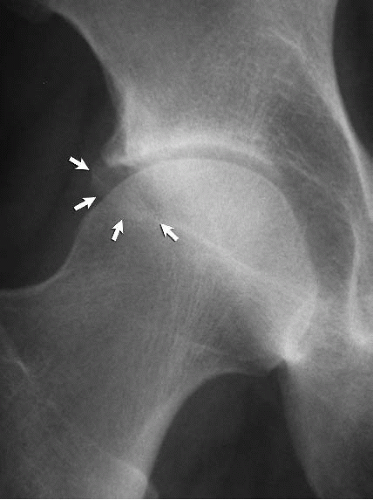
Pincer impingement is caused by an excessive prominence of the anterolateral rim of the acetabulum. This can occur simply from overgrowth of the anterior edge or retroversion of the acetabulum. Sometimes there is a separate piece of bone along the anterolateral rim, referred to as an os acetabulum. The origin of this separate bone fragment is variable and may include a rim fracture secondary to cam impingement, an unfused physis, a traction injury from the enthesis of the rectus femoris, or ossification of a portion of the labrum. With hip flexion, the prominent rim of the acetabulum crushes the labrum against the femoral neck (Fig. 50.1). This cyclical submaximal repetitive microtrauma leads to breakdown and failure of the acetabular labrum. Secondarily, over time, a variable amount of articular failure within the adjacent acetabulum will occur. Pincer impingement occurs just about equally in males and females and more commonly starts to cause symptoms in middle age (9). More severe examples of pincer impingement occur with profunda or protrusio disorders of the acetabulum. These should be carefully assessed as some may be better corrected by open surgical procedures.
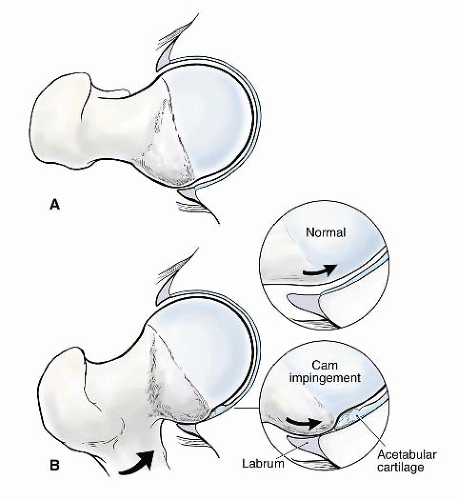
Cam-type FAI refers to the cam effect created by a nonspherical femoral head. During flexion, the prominence of the out-of-round portion rotates into the acetabulum, engaging against its surface, resulting in delamination and failure of the acetabular articular cartilage (Fig. 50.2). Early in the disease process, the labrum is relatively preserved, but, with time, it begins to sustain secondary damage. Cam impingement is classically attributed to a slipped
capital femoral epiphysis, resulting in a bony prominence of the anterior and anterolateral head-neck junction. However, the most common cause is the pistol grip deformity, attributed to a developmental abnormality of the capital physis during growth. The exact etiology of this growth disturbance is unclear; it may represent premature asymmetric closure of the physis, and it has been postulated that this could be due to late separation of the common proximal femoral growth plate that forms the physis of the greater trochanter and femoral head (14).
capital femoral epiphysis, resulting in a bony prominence of the anterior and anterolateral head-neck junction. However, the most common cause is the pistol grip deformity, attributed to a developmental abnormality of the capital physis during growth. The exact etiology of this growth disturbance is unclear; it may represent premature asymmetric closure of the physis, and it has been postulated that this could be due to late separation of the common proximal femoral growth plate that forms the physis of the greater trochanter and femoral head (14).
CLINICAL EVALUATION
The onset of symptoms associated with FAI is variable, but the damage results from the cumulative effect of cyclical abnormal wear associated with the altered joint morphology. The onset may be gradual, or often patients will recount an acute precipitating episode prior to which they were relatively asymptomatic. However, on close questioning, they will frequently recall previous nonspecific symptoms of a groin strain. Also, many patients will recount that they have never been very flexible in their hips.
Physical Examination
The trademark feature of FAI is diminished internal rotation caused by the altered bony architecture of the joint. However, there is much variation in the normative data on hip range of motion. Also, although only one hip may be symptomatic, the altered morphology is usually present in both hips and there may not be much asymmetry in motion comparing the symptomatic with asymptomatic side. Be aware that many patients may demonstrate reduced internal rotation and still not suffer from pathologic impingement. Also, although uncommon, pathologic impingement is occasionally observed in individuals with normal or even increased internal rotation. Forced flexion, adduction, and internal rotation is called the impingement test in reference to eliciting symptoms associated with impingement (Fig. 50.3). However, virtually any irritable hip, regardless of the etiology, will be uncomfortable with this maneuver. Thus, although it is quite sensitive, it is not necessarily specific for impingement. This maneuver may normally be a little uncomfortable so the symptomatic side must be compared with the asymptomatic side. Most important is whether this recreates the characteristic type of pain that the patient experiences with activities.
These conditions often have a chronic component, even at the time of initial evaluation. Thus, secondary findings may be present due to compensatory mechanisms. Lateral pain may be present from trochanteric bursitis and posterior tenderness within the gluteal muscles may be present from overfiring, attempting to splint the joint. These secondary features may be more easily evident on examination and can obscure the underlying primary joint pathology. The anterior groin, lower abdominal, and adductor area must be carefully palpated to localize tenderness suggestive of athletic pubalgia (Fig. 50.4) (15). This can mimic or coexist with FAI. Tenderness with resisted sit-ups, hip flexion, or adduction should raise an index of suspicion for athletic pubalgia. Pain with passive flexion and internal rotation is more indicative of an intra-articular source.
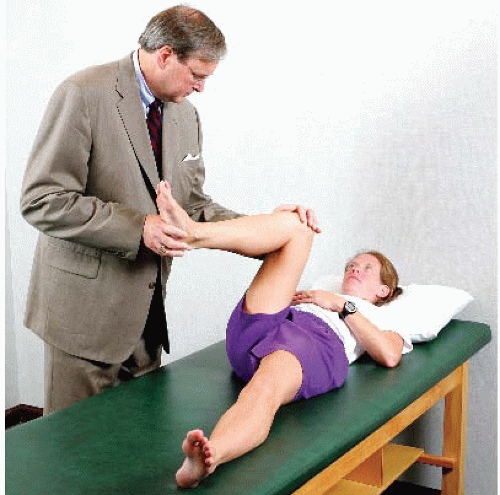 FIGURE 50.3. The impingement test is performed by provoking pain with flexion, adduction, and internal rotation of the symptomatic hip. (Reprinted with permission from J.W. Thomas Byrd.) |
Imaging
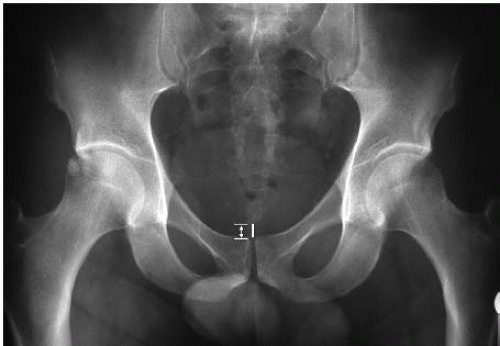
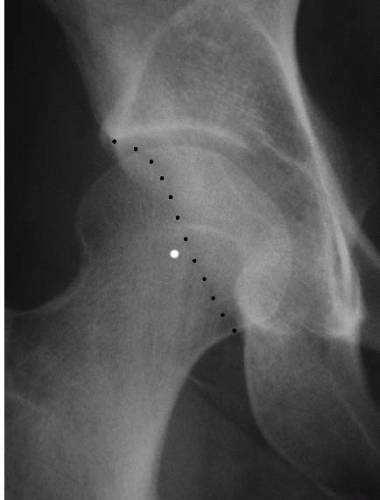
Radiographs should include a well-centered anteroposterior (AP) pelvis view and a lateral view of the affected hip (Fig. 50.5) (16). These are important for assessing impingement as well as evaluating joint space preservation and other acute or chronic bony changes. Overcoverage of the anterior acetabulum, characteristic of pincer impingement, is evaluated by the presence of a crossover sign (Fig. 50.6). This can be due to acetabular retroversion, indicated by the posterior wall sign (Fig. 50.7). The presence of an os acetabulum can also be evaluated (Fig. 50.8). The sphericity of the femoral head is assessed on both the AP and the lateral view (Fig. 50.9). There is some controversy regarding the optimal lateral radiograph. One study showed that the 40° Dunn view most predictably demonstrates the cam lesion (17). However, because of the variable shape and location of the lesion, no radiograph is consistently reliable. A frog lateral view is easy to obtain in a reproducible fashion and has demonstrated efficacy in assessing the cam lesion. Whatever lateral radiograph is chosen, the clinician must be cognizant that it can underinterpret the extent of a cam lesion. A herniation pit may be present in the region of the anterolateral femoral head-neck junction (Fig. 50.10). This has been reported with 30% prevalence in pathologic cases of FAI, but is sometimes observed in asymptomatic individuals (18). There are several caveats regarding radiographic interpretation of FAI. Indices of pincer impingement are assessed on a supine pelvis radiograph, and it is uncertain how this can be extrapolated to the orientation of the pelvis when standing. Dynamic positioning of the pelvis in real life is influenced by numerous other factors,
such as lumbar lordosis or kyphosis. The shape of cam lesions is variable and its epicenter may be more anterior or lateral. Thus, radiographs represent a poor twodimensional image of the lesion’s three-dimensional anatomy.
such as lumbar lordosis or kyphosis. The shape of cam lesions is variable and its epicenter may be more anterior or lateral. Thus, radiographs represent a poor twodimensional image of the lesion’s three-dimensional anatomy.
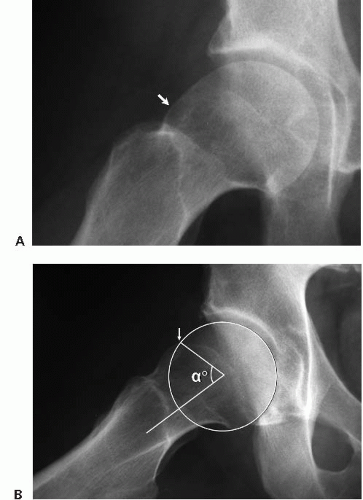 FIGURE 50.9. A frog lateral view of the right hip. A: The cam lesion (arrow) is evident as the convex abnormality at the head-neck junction where there should normally be a concave slope of the femoral neck. B: The Alpha angle is used to quantitate the severity of the cam lesion. A circle is placed over the femoral head. The Alpha angle is formed by a line along the axis of the femoral neck (1) and a line (2) from the center of the femoral head to the point where the head diverges outside of the circle (arrow). (Reprinted with permission from J.W. Thomas Byrd.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|