Femoral Shaft
EPIDEMIOLOGY
The highest age- and gender-specific incidences of femoral shaft fracture are seen in males from 15 to 24 years of age and in females 75 years of age or older.
Femoral shaft fractures occur most frequently in young men after high-energy trauma and elderly women after a low-energy fall.
The bimodal distribution peaks at 25 and 65 years of age with an overall incidence of approximately 10 per 100,000 population per year.
ANATOMY
The femur is the largest tubular bone in the body and is surrounded by the largest mass of muscle.
An important feature of the femoral shaft is its anterior bow.
The medial cortex is under compression, whereas the lateral cortex is under tension.
The isthmus of the femur is the region with the smallest intramedullary (IM) diameter. The diameter of the isthmus affects the size of the IM nail that can be inserted into the femoral shaft.
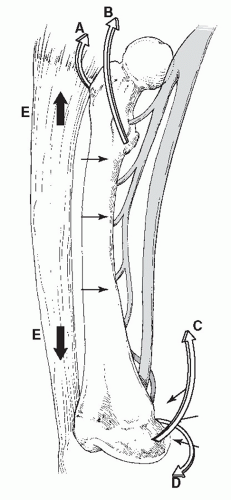
The femoral shaft is subjected to major muscular deforming forces (Fig. 32.1).
Abductors (gluteus medius and minimus): They insert on the greater trochanter and abduct the proximal femur following subtrochanteric and proximal shaft fractures.
Iliopsoas: It flexes and externally rotates the proximal fragment by its attachment to the lesser trochanter.
Adductors: They span most shaft fractures and exert a strong axial and varus load to the bone by traction on the distal fragment.
Gastrocnemius: It acts on distal shaft fractures and supracondylar fractures by flexing the distal fragment.
Fascia lata: It acts as a tension band by resisting the medial angulating forces of the adductors.
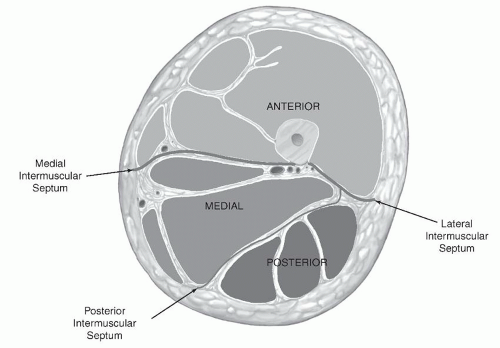
The thigh musculature is divided into three distinct fascial compartments (Fig. 32.2):
1. Anterior compartment: This is composed of the quadriceps femoris, iliopsoas, sartorius, and pectineus, as well as the femoral artery, vein, and nerve, and the lateral femoral cutaneous nerve.
2. Medial compartment: This contains the gracilis, adductor longus, brevis, magnus, and obturator externus muscles along with the obturator artery, vein, and nerve, and the profunda femoris artery.
3. Posterior compartment: This includes the biceps femoris, semitendinosus, and semimembranosus, a portion of the adductor magnus muscle, branches of the profunda femoris artery, the sciatic nerve, and the posterior femoral cutaneous nerve.
Because of the large volume of the three fascial compartments of the thigh, compartment syndromes are much less common than in the lower leg.
The vascular supply to the femoral shaft is derived mainly from the profunda femoral artery. The one to two nutrient vessels usually enter the bone proximally and posteriorly along the linea aspera. This artery then arborizes proximally and distally to provide the endosteal circulation to the shaft. The periosteal vessels also enter the bone along the linea aspera and supply blood to the outer one-third of the cortex. The endosteal vessels supply the inner two-thirds of the cortex.
Following most femoral shaft fractures, the endosteal blood supply is disrupted, and the periosteal vessels proliferate to act as the primary source of blood for healing. The medullary supply is eventually restored late in the healing process.
Reaming may further obliterate the endosteal circulation, but it returns fairly rapidly, in 3 to 4 weeks.
Femoral shaft fractures heal readily if the blood supply is not excessively compromised. Therefore, it is important to avoid excessive periosteal stripping, especially posteriorly, where the arteries enter the bone at the linea aspera.
MECHANISM OF INJURY
Femoral shaft fractures in adults are almost always the result of highenergy trauma. These fractures result from motor vehicle accidents, gunshot injuries, or falls from a height.
Pathologic fractures, especially in the elderly, commonly occur at the relatively weak metaphyseal-diaphyseal junction. Any fracture that is inconsistent with the degree of trauma should arouse suspicion for pathologic fracture.
Stress fractures occur mainly in military recruits or runners. Most patients report a recent increase in training intensity just before the onset of thigh pain.
Recently, insufficiency fractures of the femur have been reported with extended use of bisphosphonates. These fractures have an “atypical” appearance on radiographs including lateral cortical thickening, a medial spike, and a transverse to short oblique fracture line.
CLINICAL EVALUATION
Because these fractures tend to be the result of high-energy trauma, a full trauma survey is indicated.
The diagnosis of femoral shaft fracture is usually obvious, with the patient presenting nonambulatory with pain, variable gross deformity, swelling, and shortening of the affected extremity.
A careful neurovascular examination is essential, although neurovascular injury is uncommonly associated with femoral shaft fractures.
Thorough examination of the ipsilateral hip and knee should be performed, including systematic inspection and palpation. Range-ofmotion or ligamentous testing is often not feasible in the setting of a femoral shaft fracture and may result in displacement. Knee ligament injuries are common, however, and need to be assessed after fracture fixation.
More than 1 L of blood may be lost into the thigh. Therefore, a careful preoperative assessment of hemodynamic stability is essential, regardless of the presence or absence of associated injuries.
No- or low-energy mechanisms should alert the examiner to pathologic causes.
ASSOCIATED INJURIES
Associated injuries are common and may be present in up to 5% to 15% of cases, with patients presenting with multisystem trauma, spine, pelvis, and ipsilateral lower extremity injuries.
Ligamentous and meniscal injuries of the ipsilateral knee may be present in 50% of patients with closed femoral shaft fractures.
RADIOGRAPHIC EVALUATION
Anteroposterior (AP) and lateral views of the femur, hip, and knee as well as an AP view of the pelvis should be obtained.
The radiographs should be critically evaluated to determine the fracture pattern, the bone quality, the presence of bone loss, associated comminution, the presence of air in the soft tissues, and the amount of fracture shortening.
One must evaluate the region of the proximal femur for evidence of an associated femoral neck or intertrochanteric fracture.
If a computed tomography scan of the abdomen and/or pelvis is obtained for other reasons, it should be reviewed because it may provide evidence of injury to the ipsilateral acetabulum or femoral neck.