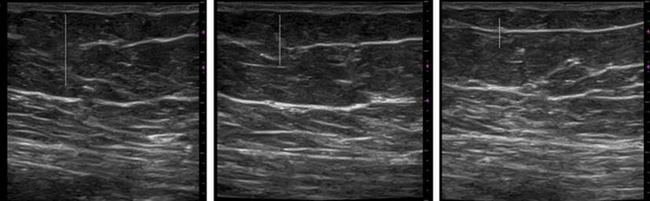
5.1 Fascia-related disorders Dupuytren’s disease (Chapter 5.2) illustrates the contractile power that can be generated by the fascia. In the early stages, vertical fibers from the palmar fascia to the skin create indentations or “pits” where they attach; later on, palmar nodules develop between the palmar fascia and the skin. Longitudinal cords develop, particularly generating deformities in the little and ring fingers. There are surgical, local and systemic pharmacologic treatments directed at the mechanical connections or the underlying processes. Chapter 5.3, Scleroderma, addresses autoimmune conditions that result in inflammation, scarring, and thickening of skin, superficial and deep fascia, blood vessels and lymphatics, and internal organs. This results in a much broader spectrum of changes than seen in the previous chapter. Patients with these conditions may have localized patches or lines of hardened tissues, or more systemic involvement affecting hands and feet, head and neck, gastrointestinal tract, lungs and heart. Conventional therapy directed toward the vascular or immune system or fibroblast proliferation can be complemented by manual therapy for specific components to restore mobility and pliability of tissues. Chapter 5.4 addresses the normal anatomy and biomechanical function of the plantar fascia and the clinical signs, imaging and histopathology in plantar fasciitis. The author proposes that normal physiological loading is not sufficient to create an overuse injury in normal plantar fascia. Rather, there is an imbalance of loading with tissue threshold for remodeling, from an underlying fascial defect which reduces tissue ability to accommodate load or from a neuromuscular defect which increases loading on otherwise normal tissues. Both of these conditions are seen in diabetes, as described, in the following chapter. The “diabetic foot” (Chapter 5.5) is seen in almost 15% of persons with diabetes. Diabetes is a disease of small blood vessels in the body, affecting not only the pancreas but also nerves (hence “diabetic neuropathy”) and peripheral skin. The elevated blood glucose levels lead to glycosylation of structural proteins in connective tissue, with fascial tissues becoming thicker and stiffer. Structural changes in the plantar fascia, Achilles tendon, and joint mobility of the lower extremity result in a constellation of changes which are termed the diabetic foot. Frozen shoulder (Chapter 5.6) is a common condition, which progresses through freezing, frozen and thawing stages, also often associated with diabetes. Despite the defined clinical progression stages, the causes of primary frozen shoulder remain largely unknown, while numerous conditions can trigger the secondary form. Physical and pharmacological treatment varies according to the stage of the disease. Myofascial trigger points (Chapter 5.7) are identified by manual palpation in everyday clinical practice in a wide variety of patients. Pathophysiological changes point to localized hypoxia with connective tissue shortening and crosslink, commonly induced by direct trauma, acute or chronic strain. Taut bands develop in conjunction with trigger points, resulting in restricted motion or coordination, decreased blood flow or sensation, or compression of neural or vascular structures. While most of this chapter deals with conditions causing tissue shortening, Chapter 5.8 addresses the issue of tissue hypermobility seen in inherited connective tissue disorders such as Marfan and Ehlers–Danlos syndromes. Patients have muscle weakness, pain, and fatigability, with reduction in vibratory sense. Extracellular tenascin-X acts as a bridge between collagen fibrils and enhances stiffness of connective tissues. Deficiency in this seems to be directly related to the muscle symptoms in humans, and studies of a mouse model with tenascin-X deficiency show reduced epimuscular myofascial force transmission. Finally, cerebral palsy with spastic paresis (Chapter 5.9) provides an example of a neurological condition affecting the ability to control and contract muscles, which may become atrophied, hypertrophied or fibrotic. Surgical and medical interventions have been developed to reduce muscle tone. Reviewing the muscle function, particularly during surgery to balance contraction power between wrist flexors and wrist extensors, has led to an appreciation of the role of the fascial connections between adjacent muscles, and even between muscles on opposite sides of a joint. These connections may vary a great deal from person to person. Further elucidation of these connections and how they form may lead to treatment plans more effectively tailored to the individual patient. A similar analysis may be useful in other neurological conditions such as stroke, multiple sclerosis, and spinal cord injury, which lead to increased tone in the muscles and have anecdotal reports of changes with manual therapies. The current state of the art and science leaves therapists primarily relying on their palpation skills (seeChapter 6.2), coupled with an understanding of the underlying physiological processes, to design and direct therapy. This section illustrates a number of the physiological changes associated with both decreased and increased motion of fascial tissues. The noninvasive imaging techniques described in Chapters 8.2 and 8.3 of this book have the potential to provide much more specific guidance to direct therapy and monitor tissue changes. Particularly important will be the development of ways to quantify the visual image, similar to what is now done in tissue elastography of the breast to detect more dense cancerous tissues. As these techniques become more widely used, the role of fascia in other conditions will become better documented and therapies will become more specific.
An introduction
Musculoskeletal Key
Fastest Musculoskeletal Insight Engine