Chapter 11 Facilitating the Teaching and Learning of Clinical Reasoning
These are excerpts from three separate focus group discussions, held with students from three different physical therapist educational programs, where they were discussing their current understandings of and their learning of clinical reasoning.1 Each of the three students quoted above was close to completion of their entry-level education, and each was expressing a degree of uncertainty in their descriptions of clinical reasoning, relating this to not having ever heard clinical reasoning overtly defined or discussed as part of their professional educations, in either the academic or clinical education settings. Each had been listening to fellow students discuss their ideas, and each was attempting to provide an explanation for the brief, superficial, and sometimes contradictory descriptions the group had been able to generate in their discussions so far.
What Can We Learn from the Clinical Reasoning of Expert Physical Therapists that can Inform Our Teaching?
Student Physical Therapists’ Understanding of Clinical Reasoning
Role of Professional Formation in Learning Clinical Reasoning
How can the Teaching and Learning of Clinical Reasoning be Facilitated in Professional Education?
Developing Clinical Reasoning Capability
After completing this chapter, the reader will be able to:
1. Recognize current research-derived models of clinical reasoning in the physical therapy literature and how this knowledge enhances the teaching and the learning of clinical reasoning in practice.
2. Recognize characteristics of the clinical reasoning of expert physical therapists and how these can be used to guide students’ learning of clinical reasoning.
3. Discuss the interdependence of deductive and inductive reasoning in adopting a biopsychosocial approach to patient care.
4. Discuss implications of recent research on the clinical reasoning of student physical therapists for professional education, including the need to link clinical reasoning to professional formation and the need for explicit links between the academic and clinical educational settings.
5. Describe elements of a clinical reasoning capability model and discuss this as a framework within which to develop strategies for facilitating the learning of clinical reasoning.
6. Develop teaching and learning opportunities for facilitating clinical reasoning in the academic setting.
7. Implement strategies for facilitation of clinical reasoning in the clinical education setting.
What is clinical reasoning?
The term clinical reasoning, in the context of allied health professional literature, is most commonly understood to represent the thinking and associated decision making of the clinician in practice. During the past three decades, this simple description of clinical reasoning has been significantly expanded and transformed by developments within the allied health professions literature. Seminal research into expert practice in nursing,2,3 clinical reasoning of experienced occupational therapists,4 and clinical reasoning attributes of expert physical therapists,5,6 as well as theoretical literature concerned with the nature and scope of clinical reasoning,7,8 all contributed to a shift in the original conception of clinical reasoning in medical literature: an individual process of diagnosis occurring inside of the clinician’s head. This more recent allied health literature characterized the reasoning process in an expanded way—involving the patient, occurring during the initial diagnostic encounter, and evolving throughout the subsequent interaction and management over the entire course of a patient’s care.
A recent description of clinical reasoning, applicable to the practice of multiple health care team members (medical doctors, nurses, physical therapists, and occupational therapists), was proposed to be “a process of reflective inquiry, in collaboration with a patient or family (as appropriate), which seeks to promote a deep and contextually relevant understanding of the clinical problem, in order to provide a sound basis for clinical intervention.”9 This definition represents a step in the right direction toward achieving a common understanding of clinical reasoning, but even this description can be considered incomplete in that it does not explicitly encompass the clinical reasoning involved with clinical tasks beyond diagnosis and choice of intervention (e.g., those related to decisions about how to interact with patients, how to teach and facilitate learning in patients, how to determine a prognosis, and how to act when faced with ethical dilemmas).6
Today, our research-derived understanding of skillful clinical reasoning in physical therapy has evolved to include the following aspects10:
• Clinical reasoning involves the interaction of individuals in a collaborative exchange to achieve a mutual understanding of the problem and to negotiate an agreed-on plan for addressing that problem.11,12
• Clinical reasoning is patient centered and situated within a biopsychosocial model of health.5,6
• Clinical reasoning involves both deductive and inductive reasoning.6,11
• Clinical reasoning is complex, nonlinear, and cyclical in nature.11,13
• Clinical reasoning plays a critical role in reflective learning from practice experiences and in the development of clinical expertise.7,11
What can we learn from the clinical reasoning of expert physical therapists that can inform our teaching?
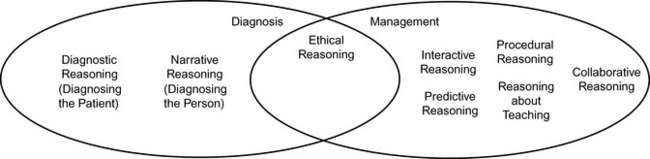
A common finding across research that distinguishes characteristics of expert physical therapists’ practice is their ability to create a collaboratively oriented clinical reasoning exchange with their patients, caregivers, and other members of the health care team.5,11,14–16 These types of exchanges are built into the structure of physical therapy practice. Jensen and colleagues5 characterized expert practice as consisting of several interrelated dimensions, each influencing and influenced by the other (Figure 11-1):
• A dynamic, multidimensional base of knowledge
• A central focus on assessment of movement as linked to functional deficits
• Consistent virtues seen in caring and commitment to patients
• A clinical reasoning process wherein patients were interacted with as people
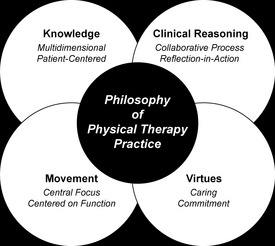
Figure 11-1 Dimensions of expert physical therapists’ practice.
(From Jensen GM, Gwyer J, Shepard KF. Expert practice in physical therapy. Phys Ther 2000;80:28-43; discussion, 44-52.)
Clinical reasoning, as practiced by the experienced physical therapists participating in the study, was collaborative and patient centered in nature: the physical therapists’ focus was on patient function and expectation rather than a medical diagnosis.5 Further, the physical therapists’ practice was focused on understanding a patient’s story, and they used clinical reasoning as a tool to fit the patient story within their clinical and experiential knowledge. These practice methods served to facilitate the collaboration that the expert practitioners valued in clinical practice.
Although the experienced therapists studied by Jensen and colleagues5 were not selected as participants based on objective criteria related to their clinical outcomes, subsequent research16 linked the expert clinician characteristics identified by Jensen and colleagues5 to superior measurable clinical outcomes, providing validity to the characterization of the clinical reasoning of experts as being associated with effective, efficient patient care, as well as being collaborative and patient centered.
The clinical reasoning of novices, in contrast, has been characterized as more therapist centered, lacking in collaboration, with less focus on understanding of the patient as a person in favor of a more narrow focus on only the physical aspects of a patient’s presentation.14–16 These differences between the clinical reasoning characteristics of novice and experienced therapists can be attributed at least in some part to the very different stages of professional practice development they represent.2 Although it is clear that novice clinicians cannot be “experts” at time of entry to practice, they can be explicitly educated to recognize aspects of clinical reasoning that align with more skillful practice and how they influence outcomes. Novices can be provided strategies to promote their own clinical reasoning development within the context of an explicitly biopsychosocially oriented, patient centered, collaborative approach to physical therapist practice.
Clinical reasoning strategies model
Edwards and colleagues6,11 explored the nature of expert clinical reasoning with their research-derived model of clinical reasoning strategies. These researchers studied the clinical reasoning of expert physical therapists in multiple practice contexts (orthopaedic, neurologic, and home health settings) and proposed a model to depict and make explicit the different types, and broad scope, of reasoning “activities” associated with all areas of clinical practice. The eight strategies composing the model (Table 11-1) were further subdivided into three broad categories6,17:
• Strategies used for diagnosing the patient
• Strategies used throughout the management components of patient care
• The ethical reasoning strategy used to drive ethical problem solving as it arises in the diagnostic and management phases of patient care
Table 11-1 Clinical Reasoning Strategies Model
| Reasoning Strategy | Description | Example |
|---|---|---|
| Diagnostic reasoning | Strategy that requires knowledge of: Necessary information and interpretation strategies must be implemented for data from both the patient interview/interaction and the physical examination. Diagnostic reasoning is a deductive strategy. | Using a diagnostic reasoning strategy to create initial diagnostic hypotheses based on interpreted data from the patient interview and examination. The hypothesis includes the identification and validation of: • Activity/participation restrictions • Pathology of body structures • The broad scope of relevant contributing factors (e.g., physical, environmental, psychosocial, emotional, behavioral) Multiple hypotheses are formulated, related to particular impairments that could be contributing to the activity or participation restrictions experienced by the patient. Hypotheses are tested via systematic questioning and physical examination testing, in order to narrow the possibilities and settle on a likely cause-and-effect relationship between impairment(s) and restricted activities |
| Narrative reasoning | Strategy that requires the establishment of and understanding of the “person” inside the patient. This strategy involves an understanding of the patient’s: Validation of these elements is equally important; the therapist should reflect the therapist’s understanding back to the patient for confirmation of understanding. The elements that make up the patient’s life experience should be explicitly integrated into the clinical reasoning and decision process. Narrative reasoning is an inductive strategy. | Using open-ended questions to ask a patient about her beliefs concerning her potential for a full recovery. The therapist then repeats those beliefs back to the patient as he has understood them to confirm she has been correctly understood. The therapist explains that he will keep these beliefs in mind as he conducts the examination, and overtly includes discussion of his findings related to his prognosis for full recovery in comparison to the patient’s beliefs. Any discrepancy is discussed further, and the plan of care reflects this discussion |
| Procedural reasoning | Strategy that requires choice in administration of interventions. This strategy uses re-examination to help determine progress and outcomes. Procedural reasoning can be both a deductive and an inductive strategy. | Therapist formulates several hypotheses about interventions likely to benefit her current patient. She selects one, asks for and receives consent from her patient to trial the intervention, and chooses impairment(s) and relevant related activity restriction(s) to re-examine upon completion of the intervention (following the session, at the end of the week, etc.) Therapist decides to continue with the chosen intervention based on results of re-examination, indicating progress toward achieving anticipated outcomes |
| Interactive reasoning | Strategy that requires a means of approach and interaction with the patient; the goal in this interaction is the establishment of rapport. Interactive reasoning can be both a deductive and an inductive strategy. | Therapist notices his patient responds more positively to a quiet, calm tone of voice (assessed by nonverbal communication cues and improved ability to focus on motor control retraining tasks ) compared with her performance while he had been joking with her earlier on in the visit. Therapist modulates his communication and consciously maintains a quiet, calm tone throughout the rest of the session, despite his own preference for establishing rapport through joking and laughing with his patients. |
| Collaborative reasoning | Strategy that requires a working relationship with the patient. The relationship will include a distribution of power in the decision-making process. Collaborative reasoning fosters a consensual approach in: Collaborative reasoning can be both a deductive and an inductive strategy. | Therapist asks her patient what her goals are for physical therapy. Patient states she has two “less important” goals, and those mirror the therapist’s hypotheses for appropriate goals. However, the goal she indicates as “most important” is one that the therapist hadn’t considered, and while it is still appropriate, feels is much less important to focus on. Therapist and patient discuss these differences explicitly and come to an agreement for a plan of care wherein the patient’s wishes for prioritization of her main goal are honored, and the other goals are also integrated simultaneously. The patient and therapist agree that this is reasonable, and although the therapist feels the patient may not achieve the goals that the therapist thinks are most important as quickly, as a result of spending some of the time in therapy focused on the goal the patient values most, both agree that the mutually derived plan of care is acceptable. |
| Reasoning about teaching | Strategy that requires approaches and strategies for educating patients. Like narrative reasoning, this strategy requires the therapist to verify that new information has been understood by the patient. The reasoning about teaching strategy can be both a deductive and an inductive strategy. | A patient returns for a follow-up session and reports that he has not performed the home exercise program prescribed at the last session. The therapist hypothesizes that the patient may not have remembered how to do the exercises and/or may not have remembered to do them during his busy work day. The therapist, however, also invites the patient to offer more of his perspective by asking, “Can you tell me more about why you didn’t perform the home program?” before beginning to reinstruct the patient or problem-solve about ways to fit the exercises into the work day. The patient indicates that he didn’t really see the relevance of those particular exercises to his particular participation restrictions and so chose not to do them. The therapist then initiates a discussion of his perception, and they come to a mutual understanding of an exercise program that is perceived as relevant to the patient and appropriate to the therapist. |
| Predictive reasoning | Strategy that requires focus on the process of developing a prognosis. Choices about management and the implications of those choices should be explored and considered (e.g., what factors influence development of the worst-case scenario vs. best-case scenario). Predictive reasoning can be both a deductive and an inductive strategy. | The patient is a woman with three very young children, all of whom require lifting for sleep, changing, and eating throughout the day. She presents to the physical therapist with a recent onset of severe lower back pain. Upon completion of the examination, the therapist discusses her prognosis for recovery from her acute back. He explains what he would predict her course of recovery could be if she could get assistance with her children and avoid lifting for a period of time, and explains how the time would likely be longer to achieve the same degree of recovery should she be unable to get help with the lifting of her children in the short term. The therapist and patient discuss her situation in light of these two possible outcomes and develop the plan of care and goals with timeframes accordingly. |
| Ethical reasoning | Strategy that requires the awareness and resolution of both ethical and pragmatic dilemmas in patient practice. The end result should be “doing the right thing” as dictated by all of the situational variables and constraints. Ethical reasoning can be both a deductive and an inductive strategy. | A physical therapist working in a for-profit private clinic has received a continuation of therapy referral from a physician for a patient with Medicare insurance who she recommended should be discharged to a home program. This therapist’s manager suggests she should continue to see the patient “to make the physician happy” because the patient has available benefits remaining. The therapist must come to a decision about continuing or not continuing care for this patient, while weighing factors related to her responsibilities to her patient, her employer, and her relationship with the referring physician. The therapist uses deductive (principle-based) and narrative reasoning to come to a context-appropriate decision. |
Data from Edwards I, Jones M, Carr J, et al. Clinical reasoning strategies in physical therapy. Phys Ther 2004;84:312-335.
These strategies were employed by the therapists in a dynamic manner, resulting in a cue-based decision-making interplay, in which different forms of reasoning were used when judged appropriate to further the mutual inquiry process by therapist with patient (Figure 11-2).6 In other words, these skilled clinical reasoners were able to respond to the emerging data and cues they perceived in a very fluid and individualized manner, most appropriate for an individual patient as he or she presents in a particular moment in time.
As noted in Table 11-1, there are different forms of reasoning employed within the whole of the model. Deductive reasoning, for example, employs development and systematic testing of hypotheses to establish a cause-and-effect relationship between variables.
Conversely, inductive reasoning does not involve the development or testing of hypotheses, but rather it proceeds from a thorough understanding of the particulars of the case, including the context in which the physical therapist interacts with the patient. As applied to this situation, inductive reasoning can be defined as the eliciting of data directly from patients, from their perspective, in order to understand that individual’s own perspective or story. In the case of narrative reasoning, a similar goal of understanding cannot be achieved by making assumptions about how one might feel if in a similar circumstance: what characterizes narrative reasoning is the focus on achieving an understanding of the person’s situation and having this validated by the patient, thereby minimizing the influence of a clinician’s bias or faulty assumptions on the reasoning process (Box 11-1). The focus of inductive reasoning is on the particulars of the case and making decisions about these.
Box 11-1 Example of Narrative Reasoning Dialogue
• Outcome of dialogue: achievement of understanding by therapist that this patient’s experience has been one of not only being limited from playing soccer with his kids, but also a feeling of losing his ability to participate in this particular way with his children as he would like to as their father.
The fluid shifts between inductive and deductive reasoning are a key finding in the research done by Edwards and colleagues.6 This shifting occurred within the therapist’s diagnostic process and throughout the patient’s continuing management. How these shifts occurred has important implications for teaching and practice: not only, then, should the therapist consider the specific findings from the patient interview and examination to come to a diagnosis, but the therapist also needs to come to a confirmed understanding of the person’s beliefs, culture, values, and experiences (i.e., all of the factors that contribute to the context in which physical therapy occurs) to fully understand how to be most effective with this particular person.
A similar dialectic occurs in ethical reasoning, the third main category of clinical reasoning in this framework.18 Deductive reasoning in ethics involves consideration of the norms of ethics, primarily bioethical principles, a profession’s code of ethics, and the accepted values of a profession. To engage in ethical reasoning from these norms alone would neglect critically important factors such as the patient’s and caregiver’s beliefs, relationships, culture, and values.19 The particular therapist’s narrative, which incorporates the therapist’s values, beliefs, and experiences, is an integral part of inductive reasoning.18 The conscious integration of the therapist’s personal narrative in ethical reasoning requires a critically self-reflective practitioner; that critical self-reflection provides the foundation for the therapist’s continued moral development.18,19
Thus, inductive reasoning in ethics provides the means through which the patient’s, the caregiver’s, and the therapist’s voices counterbalance the deductive reasoning process. Just as with clinical reasoning, expert physical therapists engage in a fluid back-and-forth between deductive and inductive when considering the ethical dimensions of their work with patients and caregivers. Each side of the dialectic informs the other, with neither alone sufficient. Expert physical therapists’ ethical reasoning is also characterized by their recognition of patterns among the different ethical situations they have encountered through their careers.18,19
This case-based reasoning, or casuistry (in which previous reasoning patterns are used to determine current action), is the means through which experienced physical therapists link their narrative and principle-based reasoning strategies. Edwards and Delany19 use the metaphor of an ethical reasoning bridge (Figure 11-3), with one pylon being the ethical principles applicable to the case and the other pylon the particulars of the case gained through narrative. The therapist uses the patterns from familiar, exemplar cases to connect the two pylons and thereby arrive at a deeper understanding of the ethical dimensions of the case, further developing their clinical expertise.
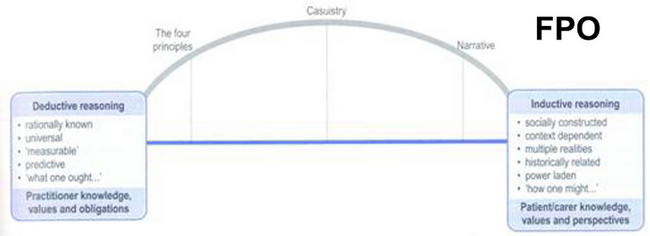
Figure 11-3 The ethical reasoning bridge.
(Modified from Edwards I, Delany C. Ethical reasoning. In Higgs J, Jones M, Loftus S, Christensen N [eds]. Clinical Reasoning in the Health Professions, 3 rd ed. Amsterdam: Elsevier, 2008.)
As mentioned previously, novices (and one might argue some less skillful experienced clinicians) have been shown to reason clinically with a focus mainly on a patient’s physical presentation,14–16 as opposed to a more holistic focus on both the physical and psychosocial aspects of the patient.1,20 It is proposed that explicit education about and practice in application of the breadth of clinical reasoning strategies, including ethical reasoning, that are used by skilled clinical reasoners (experts) can be a part of the clinical reasoning education of novices.20,21
Student physical therapists’ understanding of clinical reasoning
Recent research by Christensen1 explored what a group of student physical therapists understood about clinical reasoning, how they developed this understanding, and what factors influenced their learning of clinical reasoning. This qualitative research employed a hermeneutic approach, wherein texts were analyzed in an iterative manner, themes identified, and answers to the research questions interpreted. Methods of data collection included focus group and individual interview discussions, including postclinical observation interviews. A model of students’ existing understanding of clinical reasoning was constructed, and key factors perceived as influencing their learning were identified.
The research revealed that the student participants understood clinical reasoning to be a sequential, linear process of deductive problem solving, and variably understood related aspects such as types of knowledge used, the roles of physical therapist and client in clinical reasoning, and how to evaluate the quality of their clinical reasoning. Students demonstrated a lack of awareness of the role of collaboration in the clinical reasoning process. Their understanding was characterized by not fully comprehending the importance of the inter-relationships among the different types of clinical reasoning and how reasoning is integrated into thinking in practice. Finally, these student participants demonstrated an absence of understanding of how to use critical reflection as an experiential learning tool. Factors identified as influential in their learning included variable, largely implicit academic and clinical education curricula and inconsistent opportunities to work with clinical educators skilled in facilitation of clinical reasoning.1,21,22
Research by Nordstrom20 examined the role of physical therapy students as moral agents while on final clinical experiences. This research specifically asked what types of ethical issues these students encountered, how the students reasoned through those ethical issues, and how they negotiated action with their clinical instructors (CIs) and patients in their role as moral agents. Data were collected from physical therapy students and their CIs through journals, multiple interviews with each participant distributed throughout the clinical experience, and focus groups (separated by participant type: student or instructor) at the end of the clinical experiences.
The ethical issues encountered by the students were similar to those seen in other studies of physical therapists and students, including the importance of caring.23–32 These ethical issues were considered in a clinical context as opposed to in isolation as “ethical problems.”
The students’ reasoning was characterized by several different strategies:
• Deductive reasoning strategies, in which they considered the ethical principles and norms of the profession at issue in the situation; clinical and lay language was used rather than the specific language of bioethics.
• Inductive reasoning strategies, where the students’ personal narratives were evident, and formed primarily by the students’ past histories and their interpretations of their roles as both students and future physical therapists.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree