External Fixation in the Hand
William H. Seitz Jr
INTRODUCTION
Miniaturization of external fixation apparatus, applications, and techniques has evolved to afford hand surgeons a unique and useful tool to treat a variety of difficult conditions that they face on a regular basis. Principles as applied to the hand are similar to those applied across segments of the entire limb and long bones; however, the complexities of the hand including tendon gliding, multiple small joint interactions, fine neurologic structures, and limited space for skeletal targeting all require technical expertise and careful planning and execution of the process. The techniques of applying miniature external fixation in the hand have application in acute trauma, in posttrauma reconstruction and staged management of infections, in burn reconstruction, in deformity correction, and in congenital hand surgery (1,2,3,4,5,6,7,8,9,10).
This chapter will review the indications, contraindications, perioperative preparation, surgical technique, “pearls and pitfalls,” postoperative management, potential complications, and their management with an overview of expected results.
INDICATIONS
Acute trauma
Unstable intra-articular fractures (CMC, MP, PIP joints)
Unstable segmental fractures (pathologies unknown)
Open fractures (gunshot wounds)
Crush injuries
Soft-tissue loss
Posttrauma reconstruction
Malunion/nonunion
Arthritis
Instability
Contracture
Deformity
Amputation
Burn reconstruction
Contracture
Deformity
Amputation
Congenital hand deformity
Symbrachydactyly
Transverse terminal arrest
Hypoplastic thumb
Complex syndactyly (Apert’s syndrome)
Radial clubhand
Contractures
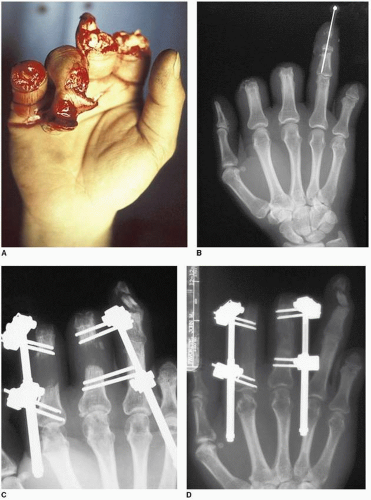
Acute Trauma
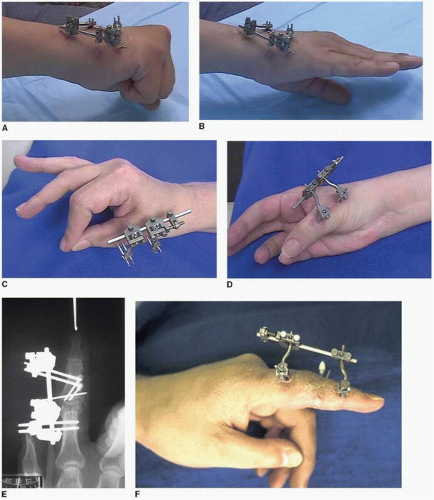
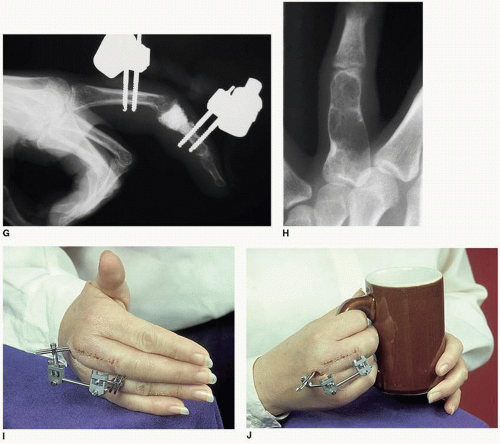
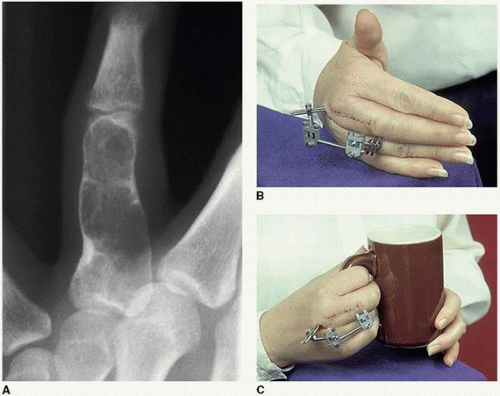
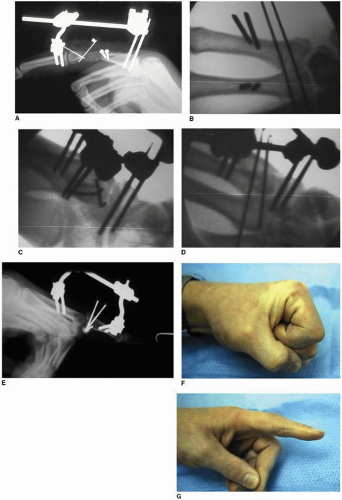
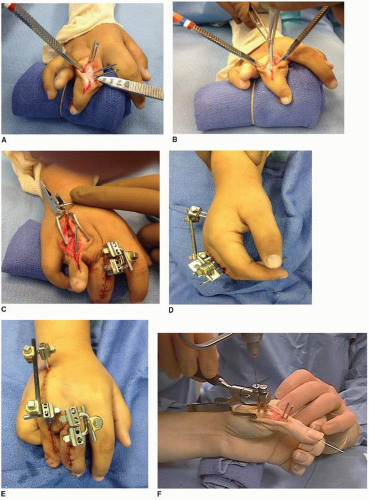
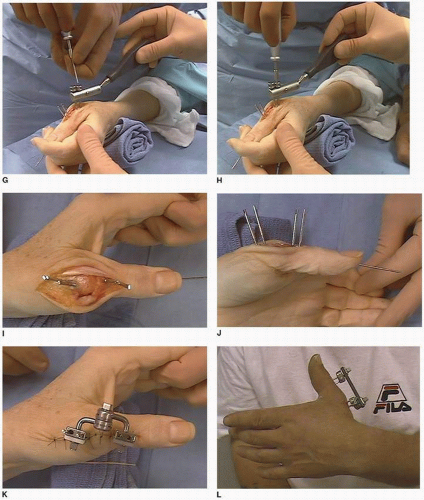
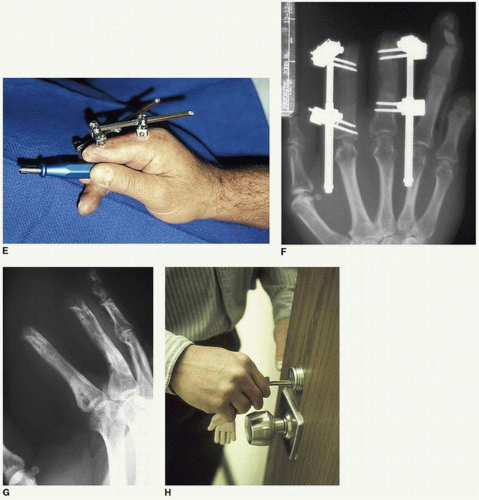
In the setting of acute trauma, indications for external fixation can include unstable intra-articular fractures involving the proximal interphalangeal (PIP), metacarpophalangeal (MP), and carpometacarpal (CMC) joints (Fig. 10-1; Video 10-1). They may also include unstable segmental fractures with or without bone loss, open fractures, crush injuries, or injuries with soft-tissue loss (skin, tendon, and muscle injury) (Fig. 10-2; Video 10-2). Some contaminated wounds may present
indications for external fixation to be used as a spanning apparatus until definitive internal fixation can be performed pending wound care, debridement, and resolution of potential infection (Fig. 10-3; Video 10-3). Areas of traumatic or burn loss of skin and subcutaneous tissue can be bridged and position maintained pending adequate coverage (Fig. 10-4; Video 10-4). Combinations of joint, tendon, burn, and soft-tissue injury may also be managed by means of dynamic fixation, which allows some degree of tendon excursion avoiding adhesions and contractures during the early healing phases (Fig. 10-5; Video 10-5) (4,11).
indications for external fixation to be used as a spanning apparatus until definitive internal fixation can be performed pending wound care, debridement, and resolution of potential infection (Fig. 10-3; Video 10-3). Areas of traumatic or burn loss of skin and subcutaneous tissue can be bridged and position maintained pending adequate coverage (Fig. 10-4; Video 10-4). Combinations of joint, tendon, burn, and soft-tissue injury may also be managed by means of dynamic fixation, which allows some degree of tendon excursion avoiding adhesions and contractures during the early healing phases (Fig. 10-5; Video 10-5) (4,11).
External fixation utilizes the principles of “ligamentotaxis” whereby the soft-tissue envelope is tensioned around the skeletal architecture to both mold the fragments into place and provide tension on the tendinous, muscular, and ligamentous structures providing a physiologic environment
so as to minimize contracture and adhesions. The principle, however, does not ensure fine fragment realignment in the face of intra-articular fractures and therefore may need to be augmented by means of fine fragment realignment using various forms of internal fixation, intercalary support, or subchondral support in the face of loss of bone stock through bone grafting (Fig. 10-6; Video 10-6) (5,8,9,10).
so as to minimize contracture and adhesions. The principle, however, does not ensure fine fragment realignment in the face of intra-articular fractures and therefore may need to be augmented by means of fine fragment realignment using various forms of internal fixation, intercalary support, or subchondral support in the face of loss of bone stock through bone grafting (Fig. 10-6; Video 10-6) (5,8,9,10).
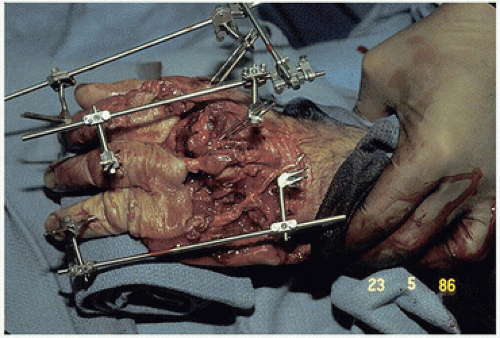
Posttraumatic Reconstruction
The outcome of trauma may result in malunion or nonunion, posttraumatic arthritis, joint instability, contracture, or amputation.
Indications for use of external fixation in posttraumatic reconstruction include providing stable fixation for realignment and osteotomy; compression arthrodesis, which leaves no long-term hardware in place; transarticular stabilization in conjunction with ligament reconstruction; slow distraction of severe contractures; and distraction lengthening of an amputated thumb or multiple digits (11,12,13,14,15,16) (Figs. 10-7A and 10-8; Videos 10-7 and 10-8).
In all these cases, the external fixation apparatus acts as a stable bridge or self-limited traction system, which is quite sturdy and supports the complexities of multiple joint control through the interaction of extrinsic and intrinsic musculotendinous excursion across the injured area allowing joint mobility of adjacent articulations and ligamentous flexibility. It is indicated in conditions where other alternative forms of fixation may not provide ideal stability (K-wires, interfragmentary screws, plate and screw fixation, and intramedullary fixation).
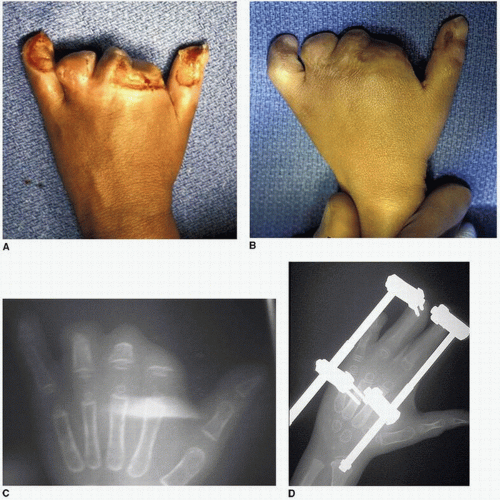
Burn and Congenital Hand Reconstruction
In patients who are born with congenital hand differences, such as symbrachydactyly, transverse terminal arrest, hypoplastic thumbs, or complex syndactyly with failure of formation of parts, external fixation techniques can be utilized applying the techniques of callotasis or distraction lengthening to elongate small digital remnants to form functional digits for purposes of sensate prehension (Fig. 10-9; Video 10-9) (12,16,17,18




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree