Level of deficiency
Type of deficiency
Treatment options
Quadriceps muscle
Palsy
Functional bracing of ankle and knee to allow knee stability with heel strike and knee flexion with toe loading
Knee joint arthrodesis
Partial disruption with residual function
Bracing in extension for 6–8 weeks
Disruption with loss of function
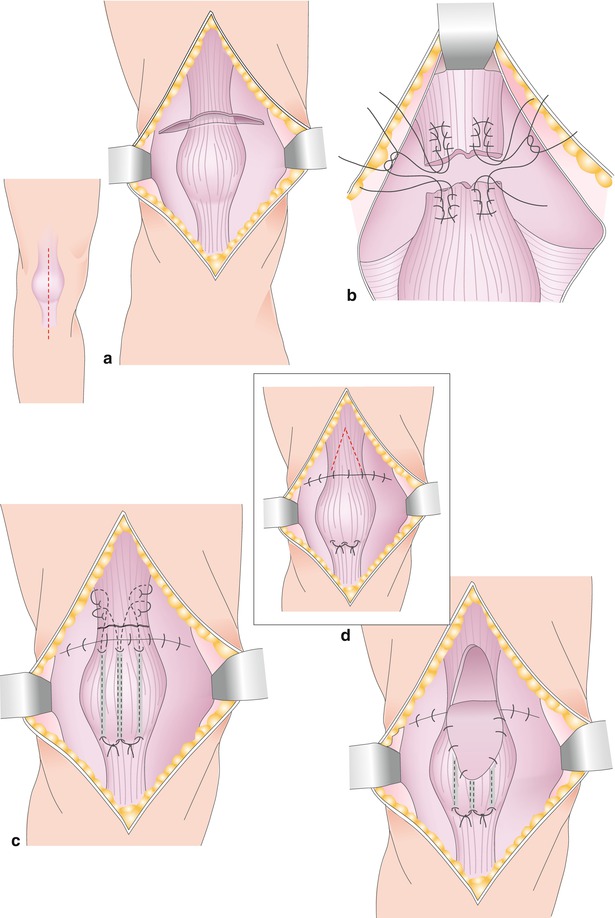
Direct repair augmented with local V-turndown flap (Scuderi procedure), fascia lata, xenograft, or synthetic membranes or heavy sutures and tapes (Fig. 17.1)
Patellar bone
Modified from Ortiguera and Berry JBJS Am (2002)
Type 1: fracture without loss of extensor function
Bracing in extension for 6–8 weeks. Removal of loose fragments after healing has completed
Type 2: fracture with loss of extensor function but stable patellar implant
Closed reduction and internal screw fixation and bracing in extension for 8–12 weeks
If no closed reduction is possible, open reduction; tension band osteosynthesis; McLaughlin suture cerclage to the tibial tubercle; augmentation with fascia lata, xenograft, or synthetic membranes; and bracing in extension for 8–12 weeks
Type 3: fracture with unstable patellar implant
(a) Sufficient bone stock: primary loose body and implant removal and cerclage of residual bone fragments; augmentation with fascia lata, xenograft, or synthetic membranes; revision resurfacing arthroplasty and bracing in extension for 8–12 weeks
(b) Insufficient bone stock (<10 mm thickness or comminution). Primary loose body and implant removal, soft tissue repair and augmentation with fascia lata, xenograft, or synthetic membranes. In addition, one of the following techniques may be used: (1) patellectomy and patelloplasty with duplication of soft tissue, (2) patellar allograft reconstruction, or (3) tantalum patellar replacement (Fig. 17.2)
Patellar tendon
Partial disruption with residual function
Bracing in extension 6–8 weeks
Disruption with loss of function
Direct repair, augmented with allogenous or autogenous semitendinosus tendon, protection with McLaughlin suture cerclage to the tibial tubercle, bracing in extension for 6–8 weeks (Fig. 17.3)
Augmentation with allogenous Achilles bone-tendon graft or patella-tendon-tubercle graft (Fig. 17.4)
Soft tissue defect preventing wound closure
Vascularized gastrocnemius skin, soft tissue, and tendon autograft
17.1 Quadriceps Muscle Deficiency and Quadriceps Tendon Rupture
Extensor mechanism failure due to quadriceps tendon ruptures is the least frequent extensor problem, with an incidence of about 0.1–1.1 % [1–3]. Quadriceps tendon ruptures are reported to be influenced by systemic risk factors like diabetes, rheumatoid or gouty arthritis, chronic renal failure, obesity, and hyperthyroidism [3, 6–10]. These systemic diseases seem to influence tissue vitality and quality, which is crucial for survival of the quadriceps tendon repair. On the other hand, the surgical technique implanting a TKR has to be considered. An aggressive resection of the patellar bone is reported to elevate the risk of a detachment of the quadriceps tendon to the patella [3]. In addition, delayed quadriceps tendon tear or insufficiency may be prevented by using the subvastus approach. If a medial parapatellar approach is used, it should be done at the medial border of the quadriceps tendon in such way that it leaves the main part of the quadriceps tendon attached to the patellar bone.
Quadriceps tendon rupture repair is difficult and the results after treatment are often unsatisfying. Reports evaluating the different treatment options for patients with quadriceps tendon ruptures after TKR are rare.
If the quadriceps muscle has lost its neutral control, functional bracing allowing flexion by toe loading and knee stabilization with heel strike is possible. However, these braces are difficult to apply, and elderly people will usually end up with removal of the implant and knee joint arthrodesis. Patients after knee fusion report relatively good clinical results. Patients report an improved quality of life compared to an insufficient and unstable TKR. Nevertheless, this procedure remains a salvage option in patients with extensor mechanism deficiency. Functional muscle transfer of the semitendinosus and biceps or gracilis have been described for cerebral palsy children with quadriceps deficiency. The clinical value of functional muscle transfers in the presence of TKR is not known [4, 5].
Dobbs et al. published good results with 6–8 weeks bracing in extension in partial quadriceps tendon ruptures, while they reported loss of function in 7 of 11 patients where they chose surgical repair [6]. In 1958, Scuderi published a technique of primary quadriceps tendon repair combined with a turndown augmentation in patients without a TKR [11]. Fernandez-Baillo and colleagues reported a case with quadriceps rupture and TKR where they successfully used the Scuderi technique. The repair was modified in that the quadriceps repair was augmented with Dacron tape [7]. Suture anchors may be used in addition to or in combination with the techniques described.
17.2 Patellar Fracture and Bony Deficiency
The incidence of patellar fractures after TKR varies from 0.68 to 3.9 % and is the most frequent reason causing definitive loss of extensor mechanism after TKR [12]. Risk factors for avascular necrosis and consecutive patellar fracture are suboptimal patellar resection leaving asymmetric and thin bone stock of less than 12 mm. Incomplete coverage of the resected patellar bone by the implant exposes the bone to high ligament stress with increased fracture risk. Excessive internally rotated femoral or tibial implants may increase lateral retinacular tension and promote lateral tracking and lateral patellar fractures [13–15]. In addition, avascular necrosis of the patella has been shown to be associated with spontaneous fracture. A medial approach combined with lateral retinacular release significantly reduces the blood supply and subsequently the vitality and bone quality of the patella. A thermal necrosis due to the exothermal polymerization of the bone cement or due to the heat of saw blades seems not to have a significant impact on avascular necrosis of the patellar bone [16, 17]. The design of the patellar component may also be involved in the incidence of patellar fractures. New implant designs of total knee prostheses with thinner patellar components, avoiding central patellar implant fixation, onlay instead of inlay patellar design, and modified femoro-trochlear grooves have reduced the incidence of patellar fractures [18].
Fortunately, only a few of these fractures result in patellar implant loosening or deficiency of the extensor mechanism. These cases of preserved extensor function can be just observed or treated with 8–12 weeks of extension bracing (Table 17.1). In the presence of a stable patellar implant and persistent symptoms, surgery is restricted to removal of the impinging fragments. In contrast, horizontal or transverse patellar fractures are rather difficult to treat. About 50 % of transverse patellar fractures result in disruption of the extensor mechanism [19]. All reports conclude that transverse patellar fractures with loss of extensor mechanism represent a difficult problem. Reconstructive surgery in the presence of TKR is prone to complications like loss of patellar bone stock, delayed wound healing, infection, loss of TKR, need of patellectomy, and the worst-case scenario, knee joint arthrodesis or amputation. Therefore, the benefits of each treatment option always have to outweigh the risks of the procedure. If the patellar component is stable and the fracture fragments are not significantly dislocated, knee immobilization in extension allowing full weight bearing is recommended. Although this treatment may result in patellar nonunion, a stable nonunion and stable soft tissue may promote sufficient extensor function. Surgical removal of impinging fragments may still be necessary to relieve pain symptoms [12].
In the native patella, tension band osteosynthesis usually is the preferred method for displaced patellar fracture treatment. However, the concept of the “figure of 8” tension band, which should transfer compressive forces to the articular fracture level, is compromised by the stiff patellar implant. At times surgeons have trouble placing the two pins or screws in the remaining thin bone stock next to the patellar component without violating component stability.
Another crucial factor for fracture healing after open reduction and internal fixation is the blood supply of the patella, as in many cases the microcirculation of the patella may have been significantly reduced by the previous TKR. A wide soft tissue stripping, circular tension band fixation will pose additional restrictions to the limited blood supply of the patella. This clearly explains the well-known increased risk of patellar nonunion following open reduction and internal fixation. Thus, the concept of tension band wiring of patellar fractures in patients with TKR has been questioned in the literature. In our small series of seven patients with partial extensor loss following patellar fracture, we used closed reduction and percutaneous screw fixation followed by immobilization for 8 weeks. All fractures united within 12 weeks follow-up. However, if closed reduction cannot be achieved, we still recommend tension band osteosynthesis combined with McLaughlin heavy suture cerclages to the tibial tubercle, but always rigorous augmentation with fascia lata, xenograft, or synthetic membranes and bracing in extension for 8–12 weeks.
If the patellar fracture is combined with a loose and free-floating patellar implant but sufficient bone stock, primary loose body and implant removal and cerclage wiring of residual bone fragments; augmentation with fascia lata, xenograft, or synthetic membranes; and revision resurfacing arthroplasty and bracing in extension for 8–12 weeks are advisable. With insufficient patellar thickness of less than 10 mm or significant bone comminution, surgery may include loose body and implant removal, soft tissue repair, and augmentation with fascia lata, xenograft, or synthetic membranes. In addition, one of the following techniques may be used: (1) patellectomy and patelloplasty with duplication of soft tissue, (2) patellar allograft reconstruction, or (3) tandalum patellar replacement (Fig. 17.5).