Extensor Mechanism Allograft
Alexander P. Sah
Craig J. Della Valle
Aaron G. Rosenberg
INDICATIONS
Extensor mechanism failure in the setting of a total knee arthroplasty can be a devastating complication that is difficult to manage. The extensor mechanism can be disrupted by tibial tubercle avulsion, patellar tendon rupture, patella fracture, or quadriceps tendon rupture (Fig. 31-1). Whether occurring intraoperatively or postoperatively, primary repair of the extensor mechanism is associated with a substantial rate of failure and associated complications (1, 2, 3).
Failure of a primary repair is often the result of compromised blood supply or significant soft tissue loss or damage. In this setting, an extensor mechanism allograft reconstruction may be indicated. A fresh-frozen allograft is composed of an intact allograft extensor mechanism including tibial tuberosity, patellar tendon, patella, and quadriceps tendon (Fig. 31-2). Although various reconstructive procedures such as medial gastrocnemius flaps or Achilles allografts have been described (4,5), we have found that the use of a complete extensor mechanism allograft has most reliably been associated with a successful outcome (6,7). We believe the success of this procedure is related to the surgeon’s ability to obtain robust fixation both proximally and distally as well as the ability to completely cover the allograft with native soft tissue in most cases. An extensor mechanism allograft may also be indicated in the treatment of severe heterotopic ossification of the extensor mechanism, severe patella baja, or conversion of a previous knee arthrodesis to a total knee with a fibrosed or deficient extensor mechanism.
CONTRAINDICATIONS
Active infection or repeated unsuccessful staged reimplantation surgeries with infection are contraindications to the procedure.
Patient inability to comply with postoperative immobilization and participation in a suitable rehabilitation program is a contraindication to the procedure.
In the setting of a problematic total knee arthroplasty (aseptic loosening, malalignment, instability), extensor mechanism reconstruction is likely to fail unless the knee is revised.
For patients not meeting the criteria for extensor mechanism allograft, bracing or knee arthrodesis are alternative options.
PREOPERATIVE PREPARATION
Preoperative planning includes an appropriate history, physical examination, and radiographic evaluation. Information regarding previous procedures or surgeries is useful to estimate the amount and type of host soft tissue available. The affected knee must be tested for both active and passive range of motion. Flexion contractures are common in total knee replacements with extensor mechanism
disruption. It must be determined whether a contracture can be addressed with soft tissue procedures or if component revision is required. Left untreated, a flexion contracture will predispose to failure of the extensor mechanism reconstruction. In addition, the tibial and femoral components should be evaluated for any signs of malalignment or loosening, which would also warrant component revision. A computed tomography scan may be useful to thoroughly evaluate component rotation (8). Hardware in the area of the tibial tubercle should be recognized, and the proper equipment should be available for possible removal. Preoperative workup for infection, including erythrocyte sedimentation rate, C-reactive protein, and complete blood count with differential are useful, followed by a knee aspiration if any of these values are elevated. Medical comorbidities or immunosuppressive therapy that may affect soft tissue healing must be taken into consideration.
disruption. It must be determined whether a contracture can be addressed with soft tissue procedures or if component revision is required. Left untreated, a flexion contracture will predispose to failure of the extensor mechanism reconstruction. In addition, the tibial and femoral components should be evaluated for any signs of malalignment or loosening, which would also warrant component revision. A computed tomography scan may be useful to thoroughly evaluate component rotation (8). Hardware in the area of the tibial tubercle should be recognized, and the proper equipment should be available for possible removal. Preoperative workup for infection, including erythrocyte sedimentation rate, C-reactive protein, and complete blood count with differential are useful, followed by a knee aspiration if any of these values are elevated. Medical comorbidities or immunosuppressive therapy that may affect soft tissue healing must be taken into consideration.
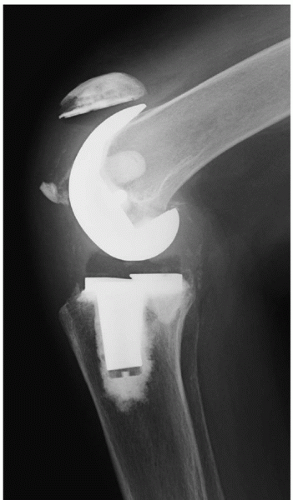 FIGURE 31-1 Preoperative lateral radiograph showing avulsion fracture of the inferior pole of the patella, resulting in extensor mechanism incompetence. |
 FIGURE 31-2 The fresh-frozen, nonirradiated extensor mechanism allograft includes quadriceps tendon, patella, patellar tendon, and proximal tibia. |
Early planning is required to ensure that a fresh-frozen, nonirradiated extensor mechanism allograft (Allosource, Centennial, CO) is available that matches the affected side. For instance, it is not advisable to use a right-sided allograft in a left lower extremity. Furthermore, although resurfacing of the allograft patella may address tracking issues, cementing a patella button onto allograft bone may lead to increased complications (9). Five cm of quadriceps tendon is necessary for sufficient soft tissue fixation and overlap with the host tissue. If the allograft tibia is not delivered in its entirety, a minimum 5 cm of tuberosity bone length must be available for sufficient distal graft fixation. The allograft should be inspected and deemed appropriate before the patient enters the operating room.
TECHNIQUE
The patient is placed supine with a bump under the ipsilateral hip. The lower extremity is prepped with draping placed as proximal as possible to allow proximal thigh exposure if necessary. In a short obese thigh, the use of a sterile tourniquet may be useful to maximize proximal exposure. Previous skin incisions are marked, and hash marks are made transversely along the planned incision to assist during closure (Fig. 31-3).
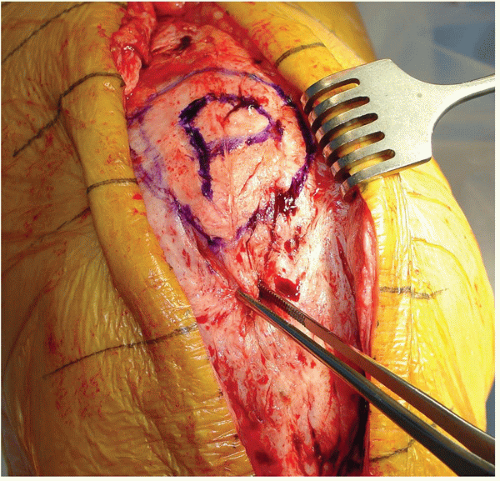
A midline incision is made through the previous skin incision. If multiple incisions exist, an attempt is made to use the most lateral incision to avoid added disruption of the vascular supply to the skin. Full-thickness subfascial skin flaps are raised on either side of the incision to preserve skin vascularity. The host extensor mechanism is evaluated, and the patella is outlined (Fig. 31-4). The host
extensor mechanism, from the quadriceps tendon through the patellar tendon, is incised in the midline (Fig. 31-5). The patella is shelled out from the host tissue and can be divided in half longitudinally in line with the extensor mechanism arthrotomy with an oscillating saw to facilitate this process (Fig. 31-6). The surrounding soft tissue is preserved in continuity with the medial and lateral flaps. This approach provides equal soft tissue on the medial and lateral sides for eventual closure over the extensor allograft. The medial and lateral gutters as well as the suprapatellar pouch are re-established (Fig. 31-7). If there is tendinous tissue at the actual site of the host tuberosity, it is removed by sharp dissection, as it is critical in allowing proper visualization for preparing the host tibial trough.
extensor mechanism, from the quadriceps tendon through the patellar tendon, is incised in the midline (Fig. 31-5). The patella is shelled out from the host tissue and can be divided in half longitudinally in line with the extensor mechanism arthrotomy with an oscillating saw to facilitate this process (Fig. 31-6). The surrounding soft tissue is preserved in continuity with the medial and lateral flaps. This approach provides equal soft tissue on the medial and lateral sides for eventual closure over the extensor allograft. The medial and lateral gutters as well as the suprapatellar pouch are re-established (Fig. 31-7). If there is tendinous tissue at the actual site of the host tuberosity, it is removed by sharp dissection, as it is critical in allowing proper visualization for preparing the host tibial trough.
 FIGURE 31-3 Previous skin incisions are identified, and hash marks are placed to assist in soft tissue closure. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree