Extensile Approaches for Revision Total Hip Arthroplasty
R. Stephen and J. Burnett
Key Points
Introduction
Surgical exposure in revision total hip arthroplasty (THA) requires careful preoperative planning and attention to detail. The most common surgical exposures utilized for revision THA surgery include posterolateral and anterolateral/direct lateral exposures. These exposures are the mainstay of revision THA surgery and are useful when acetabular revision alone is required, or when an uncomplicated revision of a femoral component is necessary, without more extensive bone defects. The decision of which surgical exposure to use will depend on factors that include surgeon experience and preference, patient body habitus (i.e., obesity), patient anatomic factors, location and type of prior surgical incisions over the hip, and implant selection. The most important aspect to consider is surgeon experience and preference. The two most commonly used routine surgical revision exposures utilized are the anterolateral and posterolateral approaches to the hip.
The anterolateral exposure is an abductor splitting approach that requires removal and repair of the anterior 30% to 40% of the gluteus medius and minimus. This approach may also be utilized for revision total hip replacement (THR) surgery. Disadvantages of this exposure include (1) an increase in limp due to splitting of the abductor muscle (also likely due to traction injury to anterior branches of the superior gluteal nerve during surgery); (2) an increase in formation of heterotopic bone within the abductor muscles and anteriorly over the capsule and greater trochanter; (3) a greater incidence of trochanteric complications (e.g., intraoperative fracture, postoperative fracture or “escape” of the greater trochanter, trochanteric pain usually secondary to failure of the abductor to heal back following repair); and (4) a tendency to insert the femoral component angled from anterior to posterior within the femoral canal (i.e., nonanatomic femoral component placement). Many surgeons select this approach on the basis of the potential for a reduced dislocation rate and are willing to accept the “disadvantages” already discussed. With the popularity of less invasive surgery, the posterolateral exposure has again gained prominence. Disadvantages of the posterolateral approach include (1) a slightly higher risk of dislocation, although with experience this is minimized, and (2) careful attention to component orientation, so that implants are inserted in proper anteversion. In Canada between 2008 and 2009,1 the direct lateral approach (60%) and the posterolateral approach (36%) were combined for more than 95% of all surgical exposures in primary and revision THA surgery.
More extensile exposures may be required to access the hip to address bone defects and exposure of acetabular or femoral periprosthetic fractures, as well as for removal of well-fixed implants (e.g., removal of a well-fixed femoral component) and those in the previously multiply operated hip. The ideal extensile exposure should satisfy several objectives. It should provide satisfactory exposure of both components. It should allow preservation of healthy bone and soft tissue for exposure and closure. Ideally, this exposure would incorporate previously healed incisions and soft tissue planes from prior exposures. Finally, extensile exposures should preserve the blood supply to bone and soft tissues, which will be incorporated into the reconstruction. The objectives of this chapter are to discuss extensile exposures to the hip (femoral and acetabular) in revision THA, while discussing the most common extensile exposures utilized, which the surgeon should be familiar with, along with indications for their use.
A detailed description focusing on the extended trochanteric femoral osteotomy extensile exposure will highlight the chapter, including pearls and technique recommendations.
Indications/Contraindications for Extensile Exposure Of The Hip in Revision Total Hip Arthoplasty
The most common revision indications include polyethylene liner wear with or without periprosthetic osteolysis, aseptic loosening of one or more components, recurrent instability, and infection (chronic or acute). Not all of these indications will require extensile exposure of the hip. If one or more components are loose and no cement is retained distal to the femoral component, then extensile exposure may not be required. If varus remodeling of the proximal femur occurs, then careful preoperative templating is required to determine the reconstructive options and whether an extensile exposure is required on the femoral side. If an isolated acetabular revision is required with retention of a well-fixed femoral component, then a more extensile exposure is required to expose the acetabulum and at the same time retract the femoral component out of the field, so that it does not prevent adequate acetabular exposure. Removal of a well-fixed (cemented) or cementless femoral component may require an extended trochanteric osteotomy; this should be planned for preoperatively. More extensile exposure of the acetabulum, which may include the outer table of the ilium or the ischium, is required if the surgeon is planning to use a reconstruction cage or porous metal augments, or to stabilize a pelvic discontinuity. Both standard trochanteric osteotomy and the trochanteric slide osteotomy provide useful extensile exposures of the acetabulum; their limitations include fixation of the osteotomy and the risk of nonunion.
Contraindications to utilizing an extensile exposure to the hip include when the hip may be approached safely by one of the previously discussed standard approaches, when there is significant risk to neurovascular structures with the extensile exposure, and when the surgeon is unfamiliar with extensile exposure techniques and options.
Preoperative Planning
Old Incisions and Previous Surgical Exposure
Prior incisions should be noted by the surgeon for incision length, location over the hip, scarring, and mobility of underlying deep soft tissues, and should be considered for their utility in revision surgery (Fig. 21-1). The preoperative history should include questions about wound healing or breakdown along one or more of the old incision(s), wound problems such as infection, and any required intervention for the wound beyond routine wound care. In addition, a history of any postoperative transient neurologic symptoms should heighten surgeon awareness of a nerve injury, transient or permanent, and may have implications for selection of a revision exposure. Frequently, patients may be unable to recall which of several incisions was used for which procedure if more than one old incision is present. Obtaining previous operating room (OR) reports, in addition to the implant record, should be imperative to determine prior exposure and to identify whether any problems were present at the time of the previous procedure(s). Incisions from childhood pelvic osteotomy procedures should be noted, particularly the ilioinguinal and iliofemoral approaches, which are not commonly utilized in revision THA surgery. The significance of these prior incisions is that there may be significant scarring in the anterior aspect of the hip, including the acetabulum and the femur, and neurovascular structures in these areas may be tethered form these prior exposures. Similarly, if a prior Southern exposure (far posterior approach at the proximal aspect) has been utilized, the surgeon should beware that the sciatic nerve may be similarly scarred or tethered within the soft tissues posteriorly.

Figure 21-1 A, Direct lateral incision. This incision is centered longitudinally over the greater trochanter and is an abductor muscle splitting approach. B, Posterolateral incision. This approach distally is similar to the anterolateral, curving from the tip of the greater trochanter slightly posteriorly and entering the hip posterior to the abductor musculature. C, Southern posterior approach incision. This approach is done even farther posteriorly and limits exposure to the superior-lateral acetabulum.
The type of prior incision should alert the surgeon to component orientation factors, which should be noted preoperatively. For example, if the prior exposure was a direct lateral (or anterolateral) approach, the acetabular and femoral components most likely will have been implanted in anatomic orientation (i.e., matching the native acetabular and the native femoral neck anteversion). In contrast, if the prior exposure used a posterolateral approach, then the components likely will have been implanted with increased femoral and acetabular anteversion. This may have implications in the selection of your exposure at revision. If the prior incision has utilized a transgluteal approach, then careful physical examination should be performed to assess side-lying abduction strength, because weakness or pain in the region of a prior abductor splitting exposure may be associated with abductor pull-off, nonhealed abductor repair (Fig. 21-2), or a dysfunctional superior gluteal nerve. If an isolated revision is being performed on the femoral side and the prior exposure was direct lateral, then if the surgeon elects to use a revision posterolateral approach, the acetabular component will have limited anteversion, and this may have implications for postoperative instability concerns.
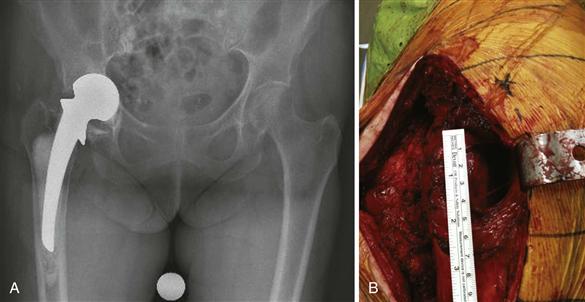
Figure 21-2 The previous hip exposure used at the time of hemiarthroplasty (A) for hip fracture was a direct lateral abductor splitting approach. At revision (B), the anterior 60% of the hip abductor musculature was absent with failure of the previous repair and the “bald eagle” sign of a bare trochanter, along with a large anterior defect of abductors and hip capsule.
Prior incisions should be considered whenever possible, depending on the procedure to be performed, to avoid the issues surrounding multiple incisions in close proximity over the hip. It is not uncommon for surgeons who use the direct lateral approach to the hip in primary THA to extend the incision slightly posterior at the proximal aspect, allowing less skin tension during femoral preparation while the leg is in the sterile leg bag. Thus, the surgeon should seek the prior OR report to identify the deep exposure because this may be confused as a prior posterolateral exposure (Fig. 21-3). Incorporating the distal aspect of an old incision that extends down the thigh is most commonly utilized, even if it is slightly anterior or posterior to the mid axial line. If the surgeon changes the direction of that old incision proximally, attempts should be made to minimize acute angles when extending off an old incision. This will help minimize wound edge necrosis. If surgery has been performed recently over the hip, the surgeon should strongly consider using the recent incision, with distal and proximal extension as needed. Performing a new parallel incision adjacent to a recent incision will place the wound at risk for wound necrosis in the bridge between these two incisions, and thus is contraindicated in the setting of a recent hip incision. If a new parallel incision is utilized in close proximity (and with a narrow skin bridge) to a remote incision, there is still concern for wound healing problems in the skin bridge (Fig. 21-4). If in doubt about old incisions and wound problems, a preoperative consultation with a plastic surgeon may be useful, especially in the multiply operated hip with scarring of the soft tissues.

Figure 21-3 A, Preoperative right total hip arthroplasty (THA) acetabular revision for aseptic loosening and a type 3A Paprosky acetabular defect. B, The prior hip incision appears to resemble a posterolateral exposure. Review of the operating room (OR) report indicates a direct lateral abductor splitting deep exposure. The same incision was utilized for an extensile posterolateral approach for the acetabular revision. C, Postoperative x-ray of acetabular reconstruction utilizing a porous metal acetabular structural augment.

Figure 21-4 The hip exposure used previously was a direct lateral approach. At revision, the surgeon elected to incorporate a posterolateral incision with a narrow skin bridge, resulting in wound healing problems, most notably in the skin bridge between the prior incisions.
Deep dissection is preferred along the route of prior surgical exposure, when possible and when the surgeon is familiar with the prior deep exposure. Deep exposure for direct lateral, posterolateral, and transtrochanteric exposures may be performed utilizing a laterally based skin incision, provided the incision is long enough and is in the midline. Attempting to perform a direct lateral (anterolateral) exposure utilizing a posteriorly based skin incision is difficult because exposure of the abductors anteriorly is very difficult.
Selecting which approach to use will be dependent on surgeon experience and familiarity. Although surgeons typically perform one approach for primary and uncomplicated revision THA surgery, the surgeon who is performing revision surgery must be familiar with multiple exposures, so that the most appropriate exposure is selected.
Radiographs and Templating for Extensile Exposures
Typical radiographs obtained before revision THA surgery include low-centered anteroposterior (AP) pelvis, AP hip, and lateral of the femur. Additional views may be helpful, such as Judet views to assess the potential for pelvic discontinuity, and cross-table lateral to assess the acetabular component version. Digital templating has emerged as a useful tool that utilizes radiographic markers to calibrate accurate implant sizes and preoperative templating (Fig. 21-5). In revision surgery for osteolysis involving the femur or the acetabulum or both, computed tomography (CT) scanning may provide useful information regarding the location and degree of osteolysis, as routine radiographs may underestimate the degree of osteolysis of the pelvis and acetabulum.

Figure 21-5 Digital templating for a revision femoral component. The radiograph must be a long film to include the femur and must be of sufficient length for revision femoral component templating so the component, as well as the acetabular component, can be revised. A ball marker of known dimension (2.54 cm) or the known femoral head diameter allows for size calibration.
It is critical to plan and template for an extensile exposure in advance, specifically, on the femoral side when an extended trochanteric osteotomy is considered. Assessment and planning for radiographic bone defects, the length of a retained femoral implant or distal cement mantle, and the implant selected for the femoral reconstruction must all be considered. On the acetabular side, if there is suspicion for pelvic discontinuity or a periprosthetic acetabular fracture, this must be considered preoperatively. Wide and extensile exposure of the posterior column of the acetabulum, ilium, and ischium is a specialized exposure, with the sciatic nerve and superior gluteal neurovascular structures at risk. If the surgeon is unfamiliar with this exposure, we recommend asking a surgeon with complex pelvic and acetabular trauma surgery experience to be involved in that aspect of the exposure and reconstruction.
The presence and severity of heterotopic ossification (HO) of bone around the hip on radiographs (Fig. 21-6) should alert the surgeon to the possibility of a difficult exposure, and to the fact that recurrence of heterotopic bone may occur. If the heterotopic bone is extensive and is causing impingement of the hip, this may affect the decision about surgical exposure and resection of this bone, which is rarely necessary. In the presence of heterotopic bone on a preoperative radiograph, the surgeon should consider utilizing HO prophylaxis, a single dose of preoperative or postoperative radiotherapy to the field, or postoperative indomethacin oral prophylaxis for 6 weeks.

Figure 21-6 A, Preoperative x-ray showing severe heterotopic ossification (HO) of the right hip. This patient has an infected total hip arthroplasty (THA) with a draining sinus. B, Removal of the extensive HO, exposure of the hip, and removal of the cementless femoral component were facilitated by an extended trochanteric osteotomy. C, Postoperative x-ray following revision to a prosthesis of antibiotic-loaded cement (PROSTALAC, DePuy, Warsaw, Ind). Indomethacin was used postoperatively for HO prophylaxis for 6 weeks.
Decription of Extensile Exposure Techniques: Femoral
Extended Trochanteric Osteotomy
The extended trochanteric osteotomy (ETO) is the most widely utilized extensile exposure for the femoral canal and is a useful exposure in revision THA surgery. Originally described by Wagner,2 this technique and its results have been reported and popularized by Paprosky and associates3–9; this approach is indicated for exposure of the femur to remove a well-fixed femoral component (and cement mantle), direct femoral canal access for femoral revision, difficult dislocation secondary to significant HO or protrusion, excellent access for acetabular revision, and correction of proximal femoral deformity in the setting of proximal femoral varus remodeling. The osteotomy may be performed via the posterolateral and the anterolateral exposure. The principle of the approach is that the greater trochanter with abductor attachments remains in continuity with a femoral shaft osteotomy with attached vastus lateralis musculature. The osteotomy, when performed posterolaterally, incorporates the lateral one third to one half of the femoral cortical shaft, and the vastus lateralis is elevated posteriorly off the intermuscular septum. Most of the vastus muscle remains attached to the cortical fragment, preserving its vascularity. When performed via the direct lateral approach, the vastus is divided at its midsubstance, and the osteotomy is hinged posteriorly. The difference between these two approaches and their muscular intervals is depicted in Figure 21-7. In addition, the ETO is useful when a standard trochanteric osteotomy may be unfavorable, as with osteolysis of the greater trochanter. With attention to surgical technique, preservation of the blood supply to the osteotomy fragment, and rigid fixation, the results of this osteotomy have been very favorable.10
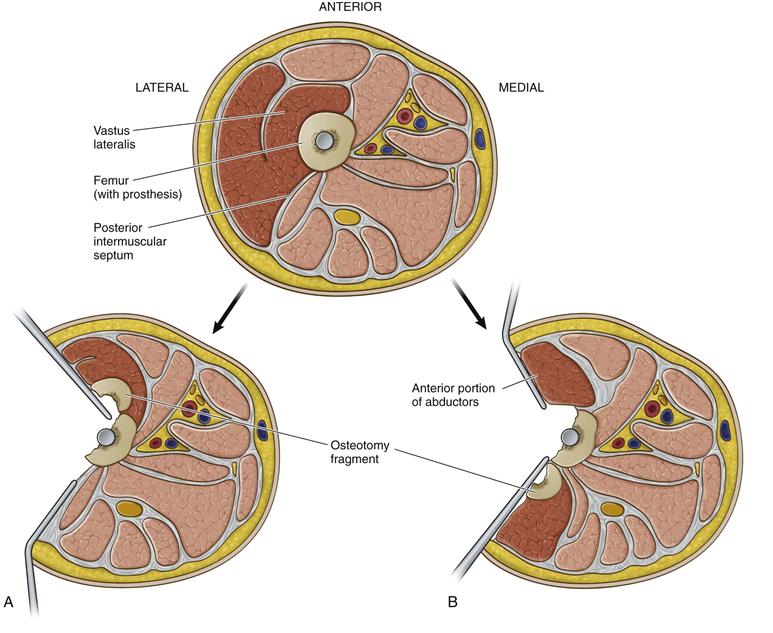
Figure 21-7 Cross-section of the proximal femur below the level of the greater trochanter demonstrating anatomic differences between the extended trochanteric osteotomy (ETO) performed via a posterolateral approach versus a modified direct lateral approach. A, When performed through a posterolateral approach, the vastus lateralis is elevated off the posterior intermuscular septum and is retracted anteriorly. The posterior limb of the osteotomy is created first, and after the remaining anterior and distal cuts are completed, the osteotomy fragment is hinged anteriorly. Most of the vastus muscle substance remains attached to the cortical fragment and helps preserve its vascularity. B, When performed through a direct lateral approach, the vastus lateralis is divided in midsubstance. The anterior portion of the vastus is retracted anteriorly in continuity with the anterior third of the abductors. The anterior limb of the osteotomy is created first, and after the remaining posterior and distal cuts are completed, the osteotomy fragment is hinged posteriorly. The posterior portion of the vastus muscle substance remains attached to the cortical fragment, which helps preserve its vascularity.
Preoperative planning for an ETO requires careful templating. Assessment of leg length differences, components to be removed, and bone defects/osteolysis are identified. The length of the osteotomy is templated to allow component removal and to preserve distal bone for the revision implant. Generally, the minimum osteotomy length is 10 cm (a shorter osteotomy may be performed) measured from the tip of the greater trochanter or 7 to 8 cm from the lesser trochanter. To remove a cemented implant with a distal cement mantle and plug, the surgeon must consider that it may not be simple to remove distal cement and the plug if the osteotomy has been performed above the cement mantle and plug. Although specialized instruments such as ultrasonic cement removal tools and cement osteotomes are helpful,11 removal of cement from above remains a challenge and is time-consuming. When possible, the osteotomy should be long enough to remove the implant along with any cement mantle, with awareness of the principle that 4 to 6 cm of scratch-fit endosteal contact may be required beyond the osteotomy for a porous-coated cylindrical revision stem. To remove an ingrown fully porous-coated cylindrical primary THA straight stem, the osteotomy should extend distal below the metaphyseal flare of the implant, to the level of the cylindrical portion of the stem. The stem may then be cut with a metal cutting wheel, and the distal stem removed with trephines3 (Fig. 21-8). If the stem is a revision bowed fully porous-coated implant, the osteotomy will not span the entire length of the implant, rather the surgeon must perform the ETO to the junction of the middle and distal one third of the implant, section the implant using a metal disk–cutting wheel, and then use trephines to trephine over the distal remaining portion of the stem.
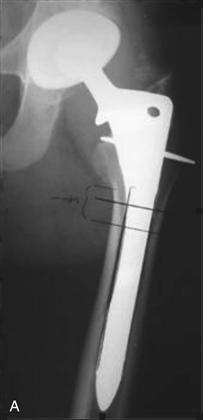

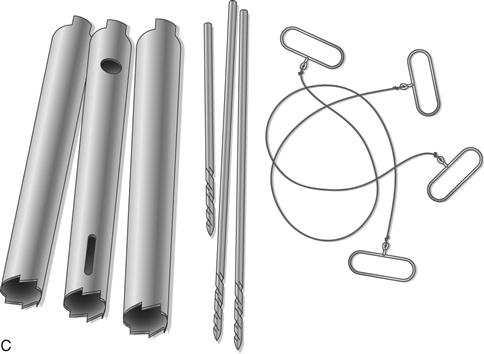
Figure 21-8 A, Removal of a cementless cobalt chrome cylindrical fully porous-coated stem requires preoperative planning and templating. The stem is cut below the metaphyseal flare of the implant with a metal cutting burr (diamond wheel disk or burr). B, The proximal metaphyseal portion is removed with Gigli saw assistance (multiple Gigli saws are necessary because they overheat and break during the procedure). Cylindrical hollow trephines are then used to trephine over the retained distal cylindrical portion of the stem. Several trephines of the same diameter are recommended because the trephine frequently cracks at the head because of fatigue and heat damage during trephining. C, Femoral implant after removal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







