Fig. 43.1
Lateral curved skin incision to the knee. Swelling and superficial necrosis due to severe hematoma
Planning of a revision surgery is even more important than a primary one. Use the same skin incision if possible. Avoid extensive dissection superficially to the deep fascia.
It also has to be emphasized that the vascular supply is asymmetric and primarily originates from the medial side of the knee. Therefore, a lateral approach always results in less vascular disturbance. However, if another medial incision is used in addition to a lateral one, regardless of the distance between these incisions, the area between the incisions is at risk for necrosis. In the case of multiple longitudinal incisions, the most lateral incision allowing reasonable exposure to the knee should be used to minimize vascular compromise to the overlying skin (Fig. 43.2). Previous transverse skin incisions should be crossed if necessary at a 90° angle (Fig. 43.3). When previous incisions cannot be used, the surgeon should try to leave an intact skin bridge of approximately 6 cm between incisions to minimize the risk of skin necrosis.



Fig. 43.2
Left knee shows scars at the medial and lateral side. Due to vascular skin supply from the medial side, avoid an additional lateral skin incision. Otherwise, skin necrosis is likely regarding the size of the skin bridge

Fig. 43.3
Previous transverse skin incisions should be crossed if necessary at a 90° angle
As the vascular supply comes from the medial side, a lateral approach is less invasive.
The anteromedial aspect of the proximal tibia has limited soft tissue coverage and is the most common location for postoperative wound problems. Avoiding delayed management of wound problems in this area is of paramount importance to avoid a deep infection. A plastic surgeon should be involved at an early stage. Treatment of these necrotic skin lesions with sole skin grafting is often not successful due to the poor blood supply. Use of a medial gastrocnemius rotation flap provides the most reliable solution here [4].
43.2 Deep Exposure
In most revision cases, a medial parapatellar arthrotomy is done. However, if a previous lateral parapatellar arthrotomy was used at primary TKR, it should be used for revision TKR to decrease the risk of patellar osteonecrosis.
If a lateral parapatellar arthrotomy was used in primary TKR, use it also in revision surgery.
During revision TKR, exposure may be facilitated by several additional steps, which are usually not routinely performed in a primary TKR. Following medial arthrotomy, wide resection of the intra-articular scar is performed by clearing any fibrous adhesions in the suprapatellar pouch and lateral and medial gutters. The proximal tibia should be exposed medially by subperiosteal dissection of the medial structures, with care taken to avoid complete release of the superficial medial collateral ligament; otherwise a more constrained prosthesis is needed.
A wide resection of the intra-articular scar tissue in the suprapatellar pouch and medial and lateral femoral gutter is recommended. The proximal tibia should be exposed medially by subperiosteal dissection. Avoid complete release of the superficial medial collateral ligament.
Adhesions over the proximal aspect of the tibia, deep and proximal to the patellar tendon should be released. At this point, the surgeon has to decide if patellar eversion can be safely performed. If this is not the case, the patella can be laterally subluxated to give adequate exposure to facilitate TKR component removal. When components have been removed, tension in the quadriceps mechanism is reduced, leading to probably easier patellar eversion.
The patella can be either everted or laterally subluxated. Avoid distal avulsion of the patellar tendon. A supporting pin placed in the tibial tubercle might help to prevent avulsion.
One must be careful not to avulse the patella tendon distally. Patellar tendon avulsion might occur when excessive tension is applied to the patellar tendon insertion. Thus, the tension applied to the patellar tendon insertion site at the tibial tubercle should be continuously monitored. The integrity of the patellar tendon insertion must be protected under all circumstances. A protective pin can be placed in the tibial tubercle to prevent avulsion, but it does not guarantee that the devastating complication of patellar tendon avulsion will not occur. Aiming for stress prevention to the patellar tendon insertion, Fehring et al. [5] described the “patella inversion method” for exposure in revision TKR. Hereby, a medial parapatellar arthrotomy is performed without eversion of the patella. In order to gain a wider exposure, an early lateral retinacular release is added. Furthermore, the tibia is progressively externally rotated and dissection is made below the periosteum to elevate the medial ligamentous sleeve until exposure is large enough to remove the primary TKR components. If necessary, dissection continues around the proximal tibia at the joint line level until the insertion of the posterior cruciate ligament. Stress on the patellar tendon insertion is released by external rotation of the proximal tibia. Once the components have been removed, the patella can be easily and safely everted to work on it. Fehring et al. reported that the patella inversion method was effective in 95 % of revision TKR [5].
If the exposure is still difficult, a number of other more invasive exposures can be used to facilitate the exposure and protect the extensor mechanism. These can be divided into proximal and distal exposure techniques. Proximal exposures include the rectus snip, the V-Y quadricepsplasty, the medial epicondylar osteotomy, and the femoral peel technique. The osteotomy of the tibial tubercle is the most commonly used distal exposure technique.
For a more extensive approach in TKR revision, proximal and distal exposure enlargement techniques can be used. Proximal exposure techniques include the rectus snip, V-Y-quadricepsplasty, the medial epicondylar osteotomy, and the femoral peel technique. The most important distal technique is the tibial tubercle osteotomy.
43.3 Quadriceps Snip
The quadriceps snip [6] is an excellent surgical maneuver to facilitate exposure of revision TKR without high risk of extensor lag noted in quadriceps turndown procedures (Fig. 43.4). The classic quadriceps snip is an oblique superior-lateral extension to the standard medial parapatellar arthrotomy. It is made at an angle of 45°. Care should be taken to maintain a significant part of the lateral vastus muscle, including the lateral retinaculum. The medial vastus muscle and the adjacent portion of the rectus femoris tendon should remain untouched. Performing an oblique snip as opposed to a transverse snip shows the advantage that a side-to-side suturing is stronger than end-to-end suturing. Performing a transverse quadriceps snip could weaken the tendon and increase the risk of extensor tendon tear. Finally, the quadriceps snip is closed in the routine fashion of a medial parapatellar arthrotomy. If a wider exposure is necessary, it can also be used in combination with a tibial tubercle osteotomy. The results after quadriceps snip extension are equivalent to those of patients undergoing a standard medial parapatellar arthrotomy [7]. There is no need for any change in the postoperative rehabilitation. Only a few complications have been reported. In a study comparing a quadriceps snip with the standard medial parapatellar approach, no significant difference was observed in terms of outcome, and no associated complications were reported [8]. The quadriceps snip has minimal associated complications and should be the first technique employed when a more invasive exposure is required in revision TKR.
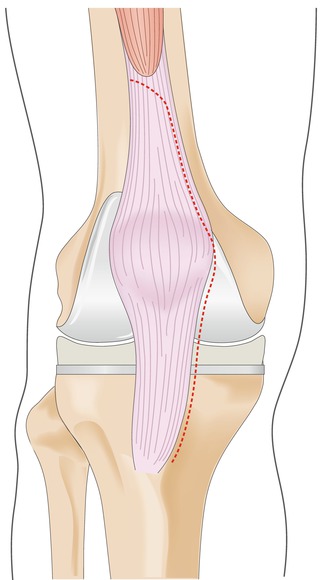
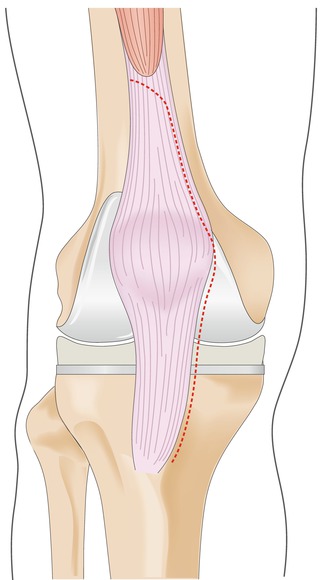
Fig. 43.4
Medial approach for revision TKR using the quadriceps snip technique in order to achieve better exposure to the knee. An oblique incision is performed at the proximal part of the quadriceps tendon
The quadriceps snip facilitates exposure in revision TKR. The classic snip is an oblique superior-lateral extension to the standard medial parapatellar arthrotomy. It is made at an angle of 45°. Care should be taken to maintain a significant part of the lateral vastus muscle, including the lateral retinaculum. The medial vastus muscle and the adjacent portion of the rectus femoris tendon should remain untouched.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








