CHAPTER 2 Examination and classification of instability
 Traumatic anterior events account for 80% of all instability and result in a predictable pattern of pathologic changes.
Traumatic anterior events account for 80% of all instability and result in a predictable pattern of pathologic changes. Thorough physical examination is imperative to include instability-specific tests such as apprehension, relocation, and load-shift.
Thorough physical examination is imperative to include instability-specific tests such as apprehension, relocation, and load-shift.Introduction
Definitions
It is also important to adequately define the terms used to describe instability. A glenohumeral dislocation event is a complete instability event in which no contact remains between the articular surfaces. This usually results in the humeral head coming to rest in the dislocated position, requiring a manual reduction by a trained provider. However, a spontaneous reduction is possible, especially in the case of glenoid or combined bone loss. The presence of a manual reduction maneuver in a patient’s history has often been used to ensure that a dislocation has occurred for research purposes.1,2 The definition of an incomplete instability event has been elusive in the literature. Most clinicians use the term “subluxation” to refer to all events that fall short of being complete events (dislocations), and that is the definition preferred by the authors. However, a subluxation event should not be confused with a microinstability event, which is a microtraumatic overuse-type injury mostly seen in throwing athletes.
Pearls
Pitfalls
Classification historical background
Among the earliest means of differentiating shoulder instability was direction, with most dislocations being anterior. In 1952, McLaughlin reported on patients with posterior events and found them to comprise only 4% of all dislocations.3 This breakdown by directionality has held true over time, with a recent prospective cohort study showing 5% of dislocations in young athletes were posterior in direction.4 However, while complete instability events (dislocations) in the posterior direction are rare, posterior subluxation events are more common, comprising 11% of all subluxation events.4
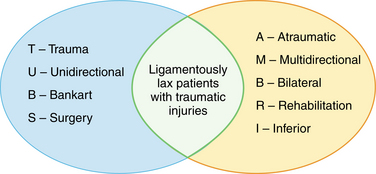
The most commonly used dichotomy of instability events (both dislocation and subluxation) is related to mechanism of injury. Rowe was the first to use traumatic versus atraumatic mechanisms to classify dislocations and found a higher recurrence rate in atraumatic patients.5 Rockwood classified subluxations into traumatic and atraumatic injuries as well as separate voluntary instability patients,6 and showed good results with nonsurgical management of atraumatic and voluntary patients.7 Thomas and Matsen continued this theme and produced the most useful classification system to date: AMBRI and TUBS (Table 2-1).8 The authors separated shoulder instability into two broad categories, the first of which was made up of patients with Atraumatic, Multidirectional, Bilateral involvement, and who were treated initially with Rehabilitation or Inferior capsular shift. The second broad category included patients with a Traumatic dislocation, Unilateral direction, and who had commonly sustained a Bankart lesion requiring Surgery (TUBS). These two descriptors accurately describe both ends of the instability spectrum but do not address the gradations between.
Table 2-1 Thomas and Matsen Classification of Instability
| T – Trauma | A – Atraumatic |
| U – Unidirectional | M – Multidirectional |
| B – Bankart | B – Bilateral |
| S – Surgery | R – Rehabilitation |
| I – Inferior (capsule) |
Gerber and Nyffeler parted from previous authors division of shoulder instability based on direction or mechanism and proposed a classification scheme based on static and dynamic shoulder instabilities.9 The authors identified three separate groups of instability: static, dynamic, and voluntary. The static group is subdivided by directionality and the dynamic group is subdivided based on the presence or absence of ligamentous laxity. Patients with voluntary instability comprised the third category.
Algorithmic approach
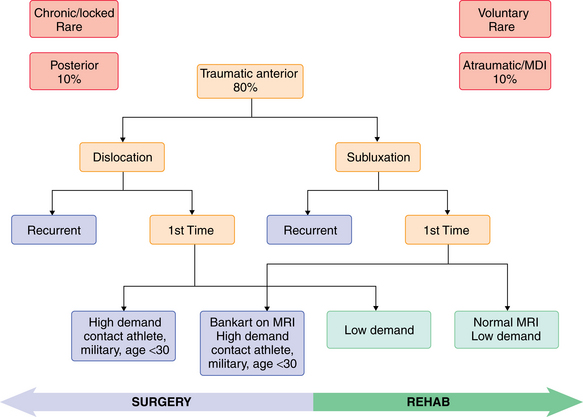
Because of the multitude of etiologies, mechanisms, directions, and contributing factors to glenohumeral instability, no encompassing classification scheme accurately accounted for patients’ unique instability. As a result, several authors have gone to a logarithmic or descriptive approach of shoulder instability.10,11 The variables in the algorithmic tree are acuity, direction, presence of trauma, degree of instability, and volitional control of the instability episodes. The algorithmic approach assists the surgeon in assessing the important variables in the patient’s condition, which identifies the presumed pathologic lesion and therapy.
The four variables from the patient history that are commonly linked to the shoulder pathology and subsequent treatment are direction of instability, etiology, frequency, and degree. These four elements of shoulder instability are not independent variables, but describing each characteristic of a patient’s condition allows for the most accurate and precise description. Many algorithmic approaches fail in rare circumstances, such as a patient with a traumatic Bankart and unilateral findings of an inferior sulcus sign associated with multidirectional instability.10
While many algorithmic approaches encompass the entire spectrum of glenohumeral instability, we offer a simplified algorithm that focuses on traumatic anterior instability that represents 80% of instability that occurs.4 We also have attempted to provide general treatment recommendations (surgery vs. rehabilitation) based on the characteristics of the instability (Fig. 2-2).
Physical exam
Although a patient’s history may guide the examiner to focus on specific aspects of the physical exam, a generalized upper examination is important to avoid missing contributing pathology that was misrepresented or omitted from the history. The physical exam of shoulder instability follows the same routine of thorough musculoskeletal exams with inspection, palpation, range of motion assessment, testing of motor strength, neurovascular examination, and specialized tests for shoulder instability. Examination of the shoulder should be preceded by an examination of the neck and cervical spine. The patient should have both shoulders completely exposed, and the examination should begin at each phase with the asymptomatic shoulder.
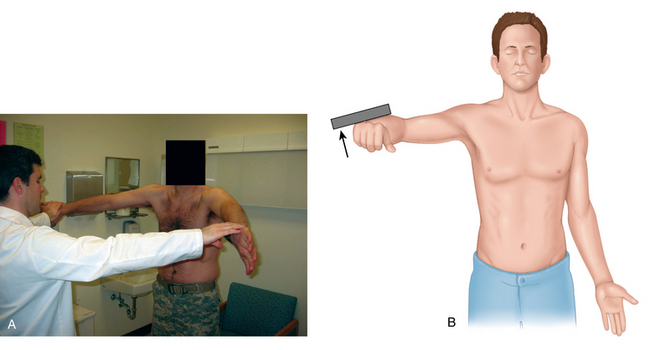
Inspection
During inspection of the shoulder girdle, muscular contour should be evaluated for asymmetry indicative of muscular atrophy of the deltoid, supraspinatus, or infraspinatus muscles. Squaring of the lateral shoulder border with a prominent acromion may represent deltoid atrophy from an axillary nerve injury (Fig. 2-3). Atrophy of the supraspinatus above the scapular spine may represent a large rotator cuff tear or suprascapular nerve entrapment at the suprascapular notch. Atrophy of the infraspinatus below the scapular spine may likewise represent a massive rotator cuff tear in an older patient or could indicate suprascapular nerve entrapment at the spinoglenoid notch in a throwing athlete, commonly from a ganglion cyst.
Palpation
Palpation of the shoulder girdle for warmth, pain, and crepitus is important and should include assessment of the coracoid, biceps tendon, acromioclavicular joint, and Codman point. Codman point, anterior to anterolateral corner of acromion with the patient’s hand on their buttocks, classically is a site of tenderness for supraspinatus or infraspinatus tendon pathology and impingement syndrome. In the setting of instability, tenderness over the greater tuberosity also may indicate a tuberosity fracture after dislocation or secondary impingement due to microinstability. Palpation of the acromioclavicular joint and the acromion could indicate acromioclavicular synovitis or a symptomatic os acromiale. Palpation circumferentially inferior to the acromion border also will confirm the position of the humeral head relative to the glenoid. A hollow sulcus is often palpable inferior to the lateral border of the acromion after an anterior glenohumeral dislocation. Patients often have posterior capsule tenderness even after reduction of an anterior dislocation. This portion of the exam should conclude with palpation around the circumference of the scapula. Patients with multidirectional instability may complain of pain diffusely around the scapula. Finally, palpation of the quadrilateral space should be performed for compression of the axillary nerve.
Muscular strength testing
The rotator cuff muscles also should be assessed specifically for strength. Jobe’s empty can test isolates the supraspinatus muscle (Fig. 2-4). The test is performed with the arm flexed to 90 degrees in the scapular plane, thumb pointed down, while the examiner applies a downward force. Pain or weakness resisting the downward pressure indicates pathology in the supraspinatus muscle. The “full can” test also can isolate the supraspinatus with the thumb pointed up, which may be less painful in patients with impingement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree