Fig. 50.1
Atlanto-axial instability in a child with Down’s syndrome
Hip Instability in Down’s syndrome
Hip dysplasia and instability is not common in children with Down’s syndrome; about 1 to 7 % develops hip instability between walking age and adolescence. Although this is usually attributed to the generalized ligament laxity and hypotonia, other anatomical abnormalities may play roles [1]. Femoral anteversion is moderately increased and there is usually a near normal neck shaft angle [2–4]. The acetabulum is retroverted in part due to a deficient posterior wall (Fig. 50.2). Over time the centre-edge angle reduces and the tear drop widens as the hip starts to sublux [2, 4, 5]. If the hip remains untreated, a stiff, dislocated and painful hip will cause significant functional impairment (Fig. 50.3) [6, 7].
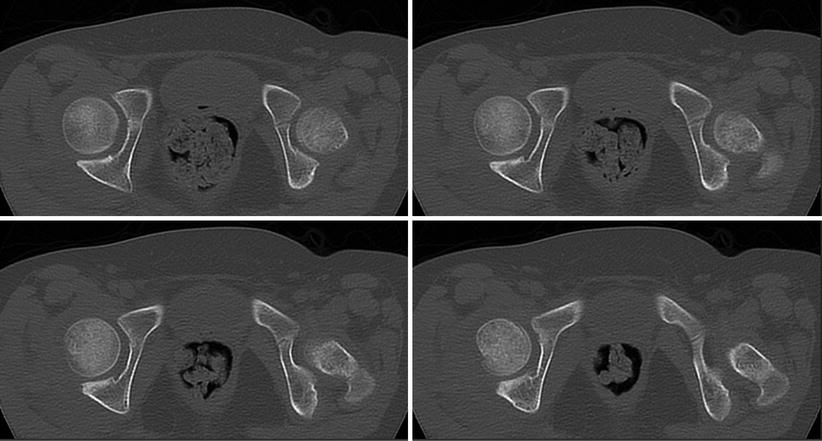

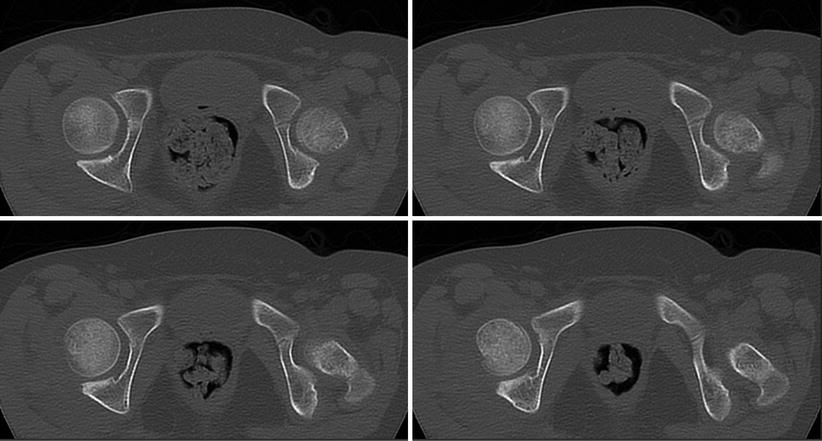
Fig. 50.2
Left acetabular dysplasia in a child with Down’s syndrome

Fig. 50.3
Long-standing dislocated hips in a child with Down’s syndrome
Hresko et al. [6] studied the natural history of hip dysplasia in Down syndrome in 65 adults and found walking ability decreased markedly with age. Even in those with normal hips, 12 of 13 were still able to walk at the age of 40 years, but by the age of 60 to 70 years only half were community ambulators. In contrast, patients with hip disease could not function as community ambulators after the age of 30 years.
Bennet et al. [7] recognised three phases in the natural history of hip subluxation in Down’s syndrome. Initial phase (<2 years old): the hips are stable but there are features of hypermobility, and walking is usually delayed. Dislocation phase (2–10 years): the hip spontaneously begins to dislocate in a particular position without trauma and tends to spontaneously reduce (Fig. 50.4). Children may be brought for treatment at this stage because of clicking, an increasing limp or a complaint of giving way. Subluxation phase (>10 years): the hip starts to decentre and progressive acetabular dysplasia develops. Fixed phase (>15 years): if untreated, the hip invariably develops a painful fixed dislocation by the time the patient is in his late ‘teens or early twenties.
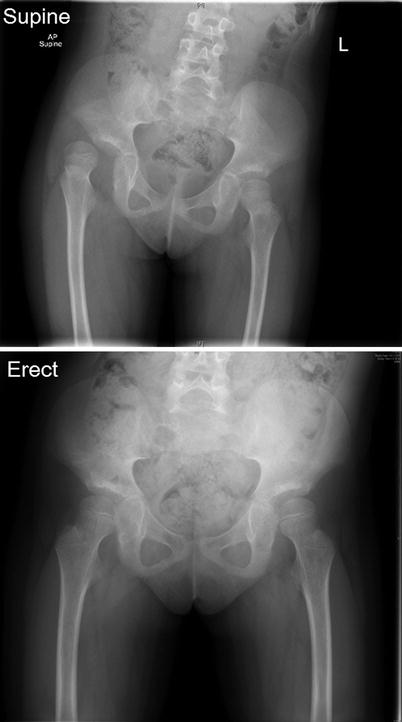
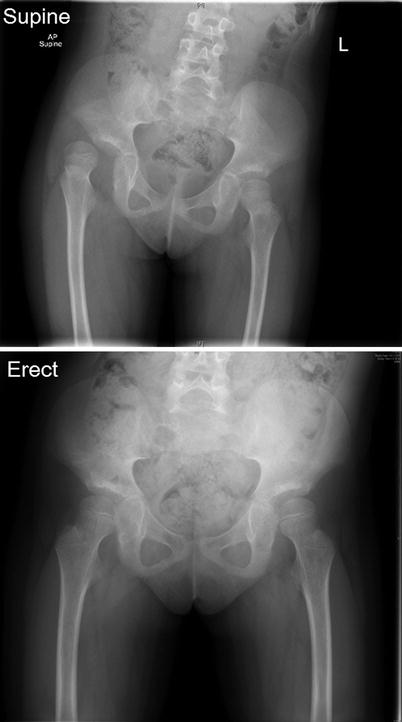
Fig. 50.4
Dislocatable right hip in a child with Down’s syndrome
Bennet reviewed a series of 28 patients (45 hips) with Down’s syndrome who were treated for hip dislocations. A variety of methods were utilized including closed reduction and hip spica [5], capsular plication [2], femoral osteotomy and capsular plication [3]; Innominate osteotomy and capsular plication [4], Chiari osteotomy [4], Schantz osteotomies [1] femoral osteotomies [9], one in conjunction with a double pelvic osteotomy. Infection rate was high at 19 % and treatment was successful in only half of cases. They concluded that a bony procedure in isolation is insufficient. Capsular plication combined with femoral +/− pelvic osteotomy yielded the best results but even this was associated with a 50 % failure rate. They also found open operative intervention is required following poor results with closed reduction and spica and that Knight et al. [8] published a single surgeon series of 9 children (16 hips) with Down’s syndrome. Patients were 5–7 years old at surgery with a mean follow-up of 5 years. All had a femoral varus derotation osteotomy to reduce the neck shaft angle (NSA) from a mean of 166° to 106°. In 2 hips, intra-operative instability remained, requiring immediate periacetabular osteotomy and capsulorraphy. Postoperatively, all patients demonstrated an asymptomatic waddling gait, which persisted in 1 individual. Two patients had implant-related fractures, one hip developed arthritis and no hips redislocated. They concluded that performing a varus osteotomy to reduce the NSA to around 105° is effective treatment for hip dislocation in children with Down’s syndrome who are under 7 years old. Implants should be removed at the appropriate time.
Sankar et al. [9] reviewed their experience of 35 hips in 29 patients (mean age 11.8 years). Twenty-five hips underwent a redirectional pelvic osteotomy (periacetabular or triple osteotomy) and 10 hips underwent a varus femoral osteotomy +/− Dega or shelf acetabuloplasty (Fig. 50.5). Although hips that underwent a redirectional pelvic osteotomy were radiologically worse, they had a better outcome with 92 % remaining stable. In contrast to 50 % only of dislocated hips remained stable following femoral osteotomy +/− acetabuloplasty.
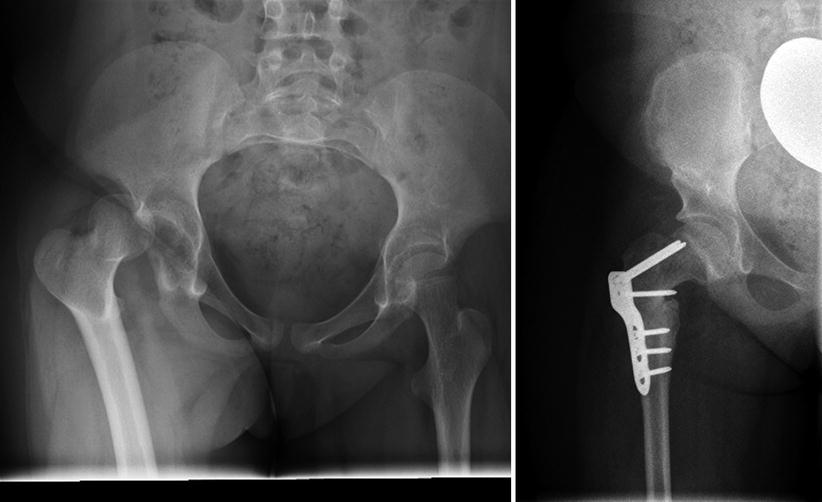
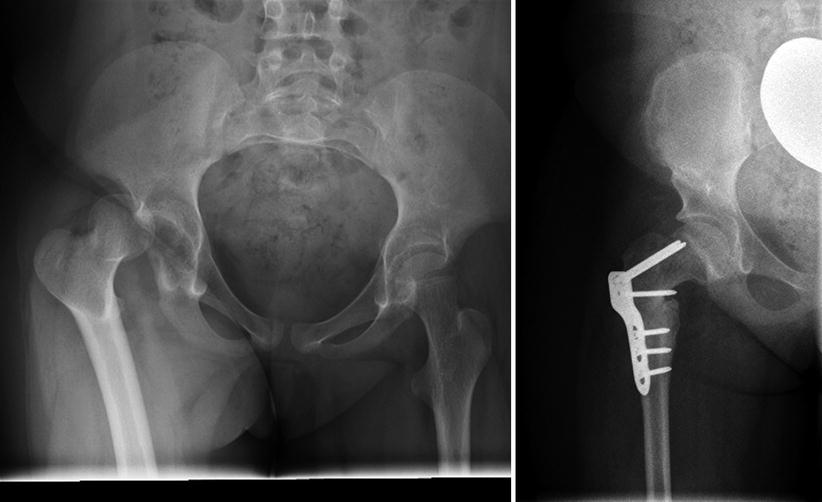
Fig. 50.5
Dislocatable right hip in a child with Down’s syndrome treated with femoral VDRO and Dega pelvic osteotomy
In summary, hip instability and subsequent dislocation in children with Down’s syndrome is an extremely challenging condition. Strong evidence to support various interventions or no intervention is lacking. Ambulation would be poor if hips are left unreduced (grade C). Closed reduction of the dislocated hip is insufficient, as is isolated capsular plication (grade B/C). In a young child (<7 years of age), a femoral varus osteotomy with judicious derotation, combined with an acetabular procedure (should instability persist) is recommended. In the older child, a redirectional pelvic osteotomy is required due to the deficient posterior wall and acetabular retroversion +/− femoral varus osteotomy (grade C). Post-operative infection is higher than normal and implants should be removed to minimize the risk of an implant-related fracture.
Patellofemoral Instability in Down’s Syndrome
Patellofemoral instability prevalence children with Down’s syndrome ranges between 4 and 8 % and it can be debilitating [10, 11]. It often causes recurrent falls, pain, poor quality of life. As with many other musculoskeletal manifestations of Down’s syndrome, ligamentous laxity, hypotonia, and joint hypermobility are thought to be primary causes. An increase in the Q angle and dysplasia of the trochlear groove may also play a role [11, 12].
Dugdale and Renshaw [11] divided patellofemoral instability in patients with Down’s syndrome into different grades by the degree of laxity (Table 50.1). Aside from this original paper, other have used this classification system [13, 14] when studying patellofemoral instability/dislocation in Down syndrome.
Grades | Description |
|---|---|
I | Stable patellofemoral joint |
II | Unstable or subluxed patella: patella subluxates laterally more than one half the patella width but does not dislocate |
III | Dislocatable patella: the patella may be dislocated during examination |
IV | Dislocated reducible patella: the patella is already dislocated, but the condition reversed manually |
V | Dislocated irreducible patella: permanent loss of normal patellofemoral articular relationship, that cannot be reduced manually |
Is There Any Role for Non-operative Treatment?
There is limited published evidence regarding non-operative treatment for this condition. In a review article detailing orthopaedic manifestations of Down’s syndrome, Caird et al. [15] generally recommend non operative treatment for patellofemoral instability in Down’s syndrome patients as a first line treatment, especially in the initial phases, with low degrees of patellofemoral instability (grade II), no pain, and scarce functional disability. The treatment modalities include the knee sleeve and activity modification. Additionally, if pes planus is a component of the problem, arch supports are recommended. Quadriceps strengthening exercises and patellar stabilising braces may be of benefit to some individuals.
Mendez et al. [16] found that nonsurgical treatments, including physical therapy and orthotics, were effective in maintaining or improving ambulation in most patients who were ambulatory before treatment. In this particular retrospective study, twenty-six dislocatable or dislocated patellae (type III, IV and V) were seen in 16 patients with Down’s syndrome. Non operative treatment either maintained or improved the ambulatory status in 67 % of these knees with either fair or good ambulation. However, 80 % of the knees with poor ambulation did not improve. Operative treatment resulted in good ambulatory ability in 86 % of the knees with fair or poor preoperative ambulatory status. As such, in knees without significant deformity, the authors recommended surgical treatment, with attention paid to soft-tissue balancing and repositioning of the insertion of the patellar tendon. They did caution that degenerative arthritis eventually developed in patients with underlying deformities, despite the method of treatment of patellofemoral instability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







