Stage
Grade
Location
Distant metastasis
IB
Low grade
Intracompartmental
No
IB
Low grade
Extracompartmental
No
IIA
High Grade
Intracompartmental
No
IIB
High Grade
Extracompartmental
No
III
Low or High
Intra or extra-compartmental
Yes
Other Prognostic Factors
More proximal site of primary disease, tumour volume >100 mL, and presence of metastatic disease indicate poorer prognostic outcome. In OSA and EWS, a high LDH is also considered to be a poor prognostic indicator [56].
Treatment
The cornerstone to all malignant bone tumours is a combination of chemotherapy and wide-margin excision. This requires a multidisciplinary approach in order to create the best management plan. The medical and surgical team should include a musculoskeletal oncologist, a bone pathologist, paediatric oncologist, paediatric medical specialist, radiation oncologist and radiologist.
The major concept of modern treatment is neoadjuvant therapy. This means that systemic treatment is initiated rapidly after diagnosis (chemotherapy), local control treatment can be planned and tailored for specific circumstances (radiation therapy and/or limb salvage/ablation surgery) and then ongoing treatment can further tailored depending on tumour factors such as necrosis rates and margins.
Chemotherapy
Chemotherapy Principles
Chemotherapy has drastically improved the survival rates of cancer patients, when combined with complete tumour resection. Chemotherapy response is the most significant factor in local recurrence. A successful chemotherapeutic response is considered to be 90 % tumour necrosis. Those with less than 90 % necrosis have a higher rate of relapse in the first two years [44]. Protocols for chemotherapy are based on those of the Children’s Oncology Group (COG). These are implemented in over 200 centres in the USA, Canada, Europe, Australia and New Zealand that treat children with cancer. Chemotherapy is not routinely required for low-grade intramedullary or surface OSAs and is variable for periosteal for low-grade periosteal OSAs [56]. All high-grade or metastatic OSA, Ewing’s and neuroblastomas require chemotherapy according to local protocol.
Complications from chemotherapy are a significant issue for patients. Mucositis and ototoxicity are the most common, but renal damage and cardiac damage can occur and function of these organs should be monitored. Ototoxicity is especially challenging for neuroblastoma patients. The damage is not only bilateral and irreversible, but affects detection of high-frequency sounds required to hear human speech. As nearly 90 % are under the age of 5 and receiving ototoxic agents while language skills are developing, this can have severe implications on social and academic development [57].
Fertility should also be addressed before initiating chemotherapy. Some chemotherapy agents can have irreversible effects on fertility and tends to affect males more than females [58]. Patients may need to be referred for sperm banking/embryo freezing.
OSA
Therapy is a multi-agent regime including various combinations of doxorubicin, cisplatin, methotrexate, cyclophosphamide, ifosfamide, carboplatin, etoposide and vincristine [2]. The COG protocol is pre-operative high-dose methotrexate with doxorubicin and cisplatin. Patients undergo several cycles before surgical excision. Post-operatively, patients with more than 90 % necrosis are divided into two groups. Half receive the same post-operative medications and the other half receives the same post-operative medications with an added pegylated form of interferon alpha 2b. If tumour necrosis is less than 90 %, post-operative chemotherapy is the same as pre-operative as well as randomly assigned ifosfamide or etoposide [59].
Ewing’s Sarcoma
Multiagent therapy for Ewing’s sarcoma is for at least 12 weeks in duration and those with metastatic disease should receive treatment for 6-months to a year. Combinations may include doxorubicin, ifosfamide, vincristine and etoposide. Dactinomycin and cyclophosphamide may also be incorporated. VAC/IE is the preferred regimen for local disease and VAdriaC for those with metastases [56]. Restaging with MRI or PET should be done following initial treatment, to determine if local control with surgery is appropriate.
Neuroblastoma
Platinum-based therapy with cisplatin, doxorubicin, cyclophosphamide, teniposide and etoposide is the basis of neuroblastoma treatment [57]. Chemotherapy may be used with the intent of myeloablation followed by autologous bone marrow transplant.
Radiation Therapy
The role of radiation in sarcoma management has diminished as chemotherapy and surgical technique has improved. Currently, it is indicated for patients with very large tumours, or for tumours that cannot be fully resected [12, 44]. It may also be used as an adjunct for marginal control.
There is an increasing evidence and acceptance for the use of Radiation therapy as sole local control therapy for Pelvic Ewings Sarcoma. This is, at least in part, due to the significant morbidity associated with pelvic resection surgery. Several studies have demonstrated equivalence in terms of local recurrence and disease free survival.
The risk of radiation in children is subsequent development of secondary tumours. Radiation is the most significant risk factor for secondary development. The excess relative risk of secondary OS is 1.4 per Gy [7]. Patients who have radiation treatment for a primary tumour require thorough follow-up to facilitate early detection of further tumours.
Surgical Treatment
Surgery should be considered for all patients, even those with metastatic disease. However, paediatric patients pose unique challenges for the operating surgeon. As chemotherapy has increased the survival rate for most childhood cancers, most children who develop OSA and EWS or secondary tumours can expect have a long life expectancy. The fundamental difference in a paediatric population is the potential for the immature skeleton and patient to heal, grow and adapt to the surgical manipulations available. The corollary of this is that the surgical reconstruction needs to be durable potentially able to withstand a ‘lifetime’ of use.
To decide the best surgical option for a patient, there are multiple factors that must be considered. Complete tumour resection is the priority and any reconstruction must accommodate for this. Other crucial considerations are the patient’s age and future growth, the location of the tumour, and the consequences the procedure will have with regards to functional outcome and quality of life.
Finally, quality of life (QOL) is a major influence on treatment choice. This is a broad, ill-defined concept, but encompasses a number of facets that need consideration. QOL includes social, emotional, and physical components. Measuring these can especially be difficult when managing young children. Expectations around quality of life come primarily from parents and may not be congruent with the best surgical option. For example, while amputation carries a very negative preconception, amputees have faster acceptance and better quality of life based on patient surveys. In fact, there is minimal data to support that limb salvage is in any way better than amputation with regards to QOL [60].
Planning
Successful surgical management requires scrupulous pre-operative planning and multi-disciplinary input. Communicate with oncology and medical teams to coordinate care, as surgery cannot interfere with chemotherapy. Discussion with surgeons from other specialties such as general, plastics, vascular or neurosurgery may be necessary depending on tumour location and tissue involvement.
MRI studies will be the guide surgical approach and precise excision. T1-weighted images are preferred. They correspond more closely to pathologic findings than STIR images, as STIR images can overestimate tumour extent [61]. MRI is highly accurate at determining neurovascular involvement, which will influence surgical management. Nerve involvement is rare but devastating. In these cases, the only likely option is amputation, as there is little value in sparing a limb if the nerve is resected [62]. The most frequent cause of nerve contamination is from pathological fracture. Vascular involvement is variable as diseased sections can be resected and vessels anastomosed.
If the growth plate has tumour involvement, the age and future growth of the patient are also important factors. A full workup of bone age and estimated adult height is useful when planning surgical measurements.
Ultimately, there is no standard algorithm for planning the correct procedure. It is a complex decision and must be tailored to the situation of the patient. Furthermore, even with extensive pre-operative planning, there are always unforeseen factors. The definitive surgical decision will ultimately be made intra-operatively and alternative plans should be in place.
Resection
En-block resection of all diseased tissue, previous biopsy tracts and adjacent soft tissue is required to consider treatment as curative. Adequate margins are a fundamental component of surgical treatment for sarcomas, and the second most important factor influencing local recurrence, after chemotherapeutic response [63]. It is universally accepted that positive margins are associated with increased risk of recurrence; however, exactly what is a ‘safe’ margin is not well established. It is usually defined in quantitative measurements, with recommendations varying between 2 mm and 7 cm of normal tissue surrounding a tumour [64]. Some consider the measurement to not be relevant; the margin is adequate as long as the quality of surrounding tissue is good. Regardless of margin width, there are uncontrollable factors such as tumour location, size, grade and metastasis that will have influence overall prognosis [65]. The final excision biopsy should be assessed for margins, overall tumour necrosis, as well as the size and dimensions of the tumour to ensure complete removal and to guide post-operative chemotherapy [56].
Reconstruction
There are fundamental questions that must be asked when considering limb salvage. First, is limb salvage possible? This is primarily based on location of the tumour and neurovascular involvement. Second, is limb salvage functionally desirable? This will be based on age and future growth, any future reconstruction that may be required and what the functional outcome of reconstruction will be. Currently, over 90 % of patients diagnosed with OSA can be treated with some form of limb salvage. However, it is important to be aware that this is accompanied by a 60 % complication rate and 75 % revision rate.
Following the resection of some bone tumours, reconstruction offers no functional benefit. Examples of this include the proximal fibula (Fig. 44.1), individual ribs, the clavicle and parts of the scapula.
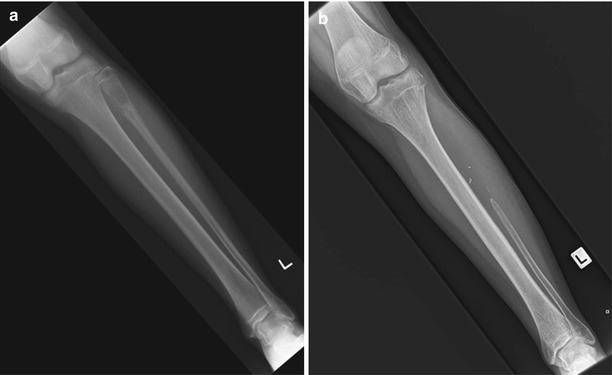
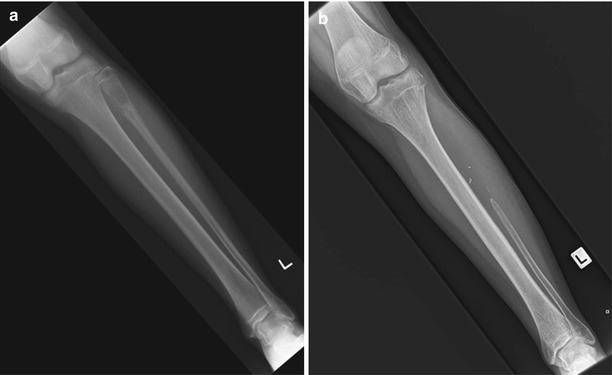
Fig. 44.1
Osteosarcoma of the proximal fibula. Thirteen year female presenting with osteosarcoma of the left proximal fibula; (a) presentation film and (b) resection of the proximal half of the fibula without reconstruction
Biologic Reconstruction
Autograft
Autograft can either be involved tumour bone that has been sterilised or unaffected host bone. Unaffected host bone can either be vascularised or non-vascularised.
Irradiated or pasteurized autografts of the patients affected bone have a variable success rate. Experimentation using cryosurgery with liquid nitrogen of the autograft has also been trialled [66]. In order to consider using autograft tumour bone, there must be less than one-third cortical bone destruction, tumour confinement to one compartment and osteoblastic pattern [66, 67]. Positive features include the fact that no foreign material is used and a perfect fit is achieved at reconstruction [68]. Mid-term survivorship is comparable to other methods; however, non-union and infection rates are still very high.
Other biologic autografts may be used. The most common donor site for vascularised grafts is the fibula (Fig. 44.2), followed by the tibia and iliac crest. These can be combined with fascial, muscle and cutaneous components. If the bone defect is greater than 6 cm, vascularised autograft is preferable. As it is the patient’s own vascular bone, excellent integration and healing is typically seen, and for these reasons they are often combined with allograft usage.
Fig. 44.2
Osteofibrous dysplasia right fibula. Osteofibrous dysplasia right tibia; (a) presentation age 6 with pathologic fracture. (b) following union and observation, deformity and further pain developed age 12. (c) following resection and intercalary allograft reconstruction augmented with an ipsilateral vascularised fibula transport
Non-vascularised autograft is typically particulate graft harvested from the iliac crest. This provides good osteoinductive properties but limited osteoconductive properties.
Distraction Osteogenesis
Following tumour resection, a temporary spacer placement can be utilised to encourage vascularised membrane formation followed by a delayed secondary grafting procedure. This technique was popularised by Masquelet and colleagues. They describe excellent longterm results with this technique [69, 93].
Distraction Osteogenesis utilises a similar principle to achieve biologic filling of a bony defect [94].
Intercalary Allograft
Allografts can be composed of either cancellous bone or cortical bone. The use of intercalary allografts for metaphyseal and diaphyseal lesions (with or without vascularized fibula) can provide excellent outcomes and sparing of the growth plate eliminates the issues of limb length discrepancy [4, 70] (Fig. 44.3). Consolidation time is long, averaging 6.5 months at the metaphyseal and 16 months in the diaphyseal osteotomy sites and overall survival rate of the graft is approximately 76 % at 10-years. The most significant risk is non-union, thus adequate fixation of cortical grafts is vital, achieved with plates. Allograft collapse is also a possibility; therefore, the number of screw holes placed in the graft should be minimal to prevent structural compromise. Intramedullary nails have also been used for fixation but non-union of the diaphyseal junctions are higher with nail fixation, likely due to inadequate compression between graft and host bone [71]. Some studies using compressible intramedullary devices have shown improved rates of union [72].
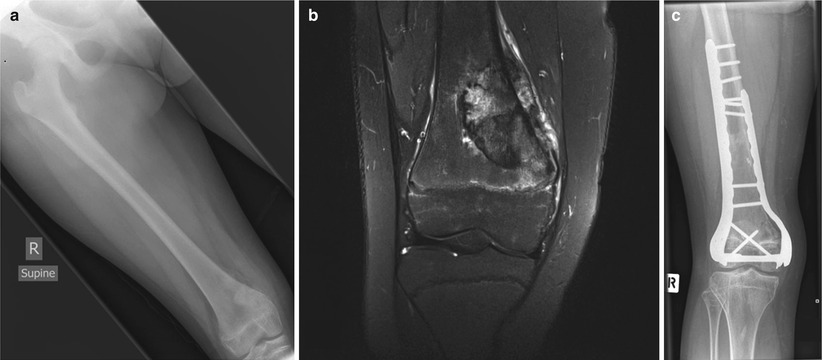
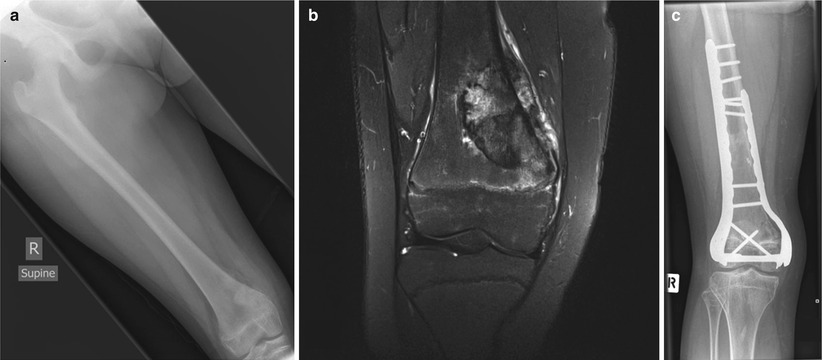
Fig. 44.3
Right distal femoral osteosarcoma. A 13 year. female with right distal femoral osteosarcoma; (a) Presentation film, (b) Coronal MRI demonstrating tumour extent and oedema at the level of the physis, (c) Following transepiphyseal resection and intercalary allograft reconstruction
Osteoarticular Allograft
Osteo-articular allografts are an option when the joint cannot be preserved. Fracture, non-union, joint instability, articular degeneration, and infection are common, thus it is utilised as a temporary solution for patients who still have significant growth [73]. Graft survival is 37–71 % at 5–10 years [73]. It carries a very high re-operation rate. Once skeletal maturity is reached, a conversion to a composite endoprosthetic joint can be performed.
Transepiphyseal Resection
Transepiphyseal resection may be considered a safe method of limb salvage for patients with juxta-articular lesion. If there is no indication of tumour involvement within the joint on MRI and a safe margin can be obtained, an osteotomy can be made through the epiphysis to preserve the articular portions. Reconstruction has been achieved with epiphyseal fragments as little as 0.5–2 cm, with no reported incidences of AVN or epiphyseal non-union. Reconstruction is with an intercalary graft with or without vascularised fibula [74]. Fixation is achieved with a lateral plate and screws. Diaphyseal fixation is with a plate or with rod.
Complications include deep infection, joint stiffness, diaphyseal non-union and stress fractures. In follow-up studies of patients receiving a transepiphyseal resection (82 patients in 5 studies over an average follow-up time of 54.2 months), there were no cases of local recurrence. Functional outcome is very good, with no restrictions of physical activity [74–76].
Arthrodesis
Arthrodesis is utilised primarily for the salvage of a failed allograft or failed ER. It usually is not desirable as it removes the joint function. However in certain circumstances it is a useful treatment option. Joints which can be arthrodesed with minimal functional loss include the wrist, shoulder, hip and ankle. Arthrodesis of the knee greatly decreases gait efficiency, but it is durable and functional with 86 % of patients achieving independent ambulation [60, 77]. In general, patients with arthrodesis have reasonable functional outcomes with average MSTS scores of 77 % [77] (Fig. 44.4).


Fig. 44.4
Chondroblastic osteosarcoma right distal fibula. A 17 year. female with chondroblastic OSA right distal fibula; (a) presentation films and (b) following fibula resection and tibiotalar arthrodesis
Prosthetic and Alloprosthetic Reconstruction
Endoprosthetic Reconstruction
At first glance, endoprosthetic reconstruction appears to be the silver bullet for limb salvage surgery (LSS). They can be modular or custom made while the patient is undergoing pre-operative chemotherapy. It enables early mobility and is aesthetically desirable to patients (and parents) as it recreates the entire limb. It creates a mechanical joint for patients who have joint involvement and for many has very good functional outcomes in the short term. MSTS scores are very high with ER in the first post-operative years.
Its downfall is in longevity and durability and for growing patients, a lack of dynamicity. Paediatric patients have many decades of active life ahead of them, and it is unlikely that an endoprosthetic reconstruction will withstand a lifetime of wear and tear. Implant survival is variable and can be anywhere from 50 % to 90 % at 5–10 years [78, 79]. ER has a high complication rate including aseptic loosening, mechanical failure, periprothetic fracture and infection [79]. Thus, when performing an ER on a young patient, one should anticipate and plan for future revisions. Surprisingly LSS does not correlate with significantly improved levels of quality of life when compared to other options such as rotationplasty or amputation.
Children with more than 2–3 cm of growth should not be considered for ER, as there is much anticipated growth and the limb length discrepancy will be too significant [44]. This has been challenged with the advent of telescopic devices that “grow” and extend with the child. Newer versions use an electromagnetically driven gearbox that turns a drive screw to extend the prosthetic rod. Lengthening is a non-invasive outpatient procedure and avoids subsequent surgeries. Short term outcomes are attractive but are still fraught with risk [80]. Infection rates between 25 % and 40 % are the most common complication, but implant breakage, gearbox failure and loosening also can occur, leading to high rates of revision [60, 81, 82].
For all endoprosthetic devices, infection risk is high. A significant contributing factor to infection is poor soft-tissue coverage and sufficient coverage of implants is essential. This may be through the use of muscle flaps. For example, in tibial reconstruction, introducing a gastrocnemius flap reduced the risk of infection from 36 % to 12 % [83] (Fig. 44.5).
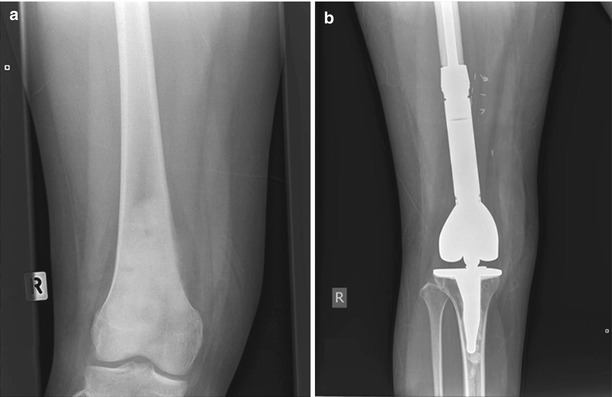
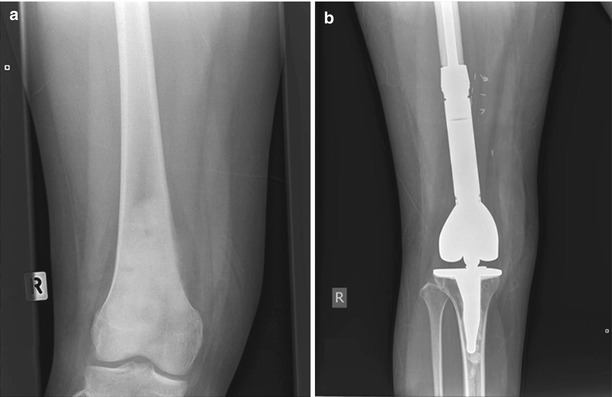
Fig. 44.5
Right distal femoral OSA. A 14 year. female with right distal femoral OSA, metastatic at presentation; (a) presentation film and (b) following resection and distal femoral endoprosthetic reconstruction
Allograft Prosthetic Composite
APC techniques replace the necessary bone stock with frozen allograft combined with a metallic implant. The allograft provides soft tissue attachments and the metallic joint implant provides better stability and function than osteoarticular allografts. Common sites for APC are the distal femur and proximal tibia, proximal femur and proximal humerus. APCs pose the same complication risks as ER and allograft, but can provide excellent functional results in the reconstruction of difficult soft tissue organs such as the extensor mechanism (Fig. 44.6).


Fig. 44.6
Osteosarcoma of right proximal tibia. A 13 year. male with OSA right proximal tibia; (a) presentation film and (b) following resection and allograft-prosthetic reconstruction
Rotationplasty
Rotationplasty is a modified amputation reserved for patients for which limb salvage is not feasible. It involves the resection of the tumour site and rotation of the distal limb portion, creating a biological recreation of a joint. Pre-operative planning is imperative in this operation as children undergoing rotationplasty are young. The remaining growth of the child needs to be taken into consideration to minimize limb length discrepancies. Contraindications include compromise of the sciatic nerve, poor ankle or foot function, or limb infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







