Chapter 12 Evaluation of the Trunk and Hip CORE
Evaluation of the athlete presents unique challenges to the rehabilitation professional. Even in an injured state, athletes can often outperform many uninjured subjects in standard tests and measures. Thus the examination tools must be sensitive enough to measure higher levels of performance. On the other hand, research demonstrates that the recurrent nature of athletic injuries is often secondary to previously unidentified relative weaknesses or residual impairments from previous injuries.1–3 Therefore the sports therapist must use tests and measures specific enough to identify the underlying impairments that preclude an athlete to injury or reinjury.
This chapter describes select methods to evaluate the performance of the trunk and hip CORE structures identified in Chapter 11. The goal of this chapter is to describe evaluation methods geared toward identifying the CORE impairments that predispose athletes to injury or reinjury. Whenever possible the authors have attempted to provide valid and reliable tests. However, many evaluation tools still lack evidence as to their efficacy. In these cases the authors attempted to discuss the theories behind assessment techniques to allow the reader to judge their worth as clinical tools.
Providing a comprehensive evaluation of the trunk and hip is not the goal of this chapter. The authors refer the reader to numerous excellent references, such as Magee’s Orthopedic Physical Assessment, ed 3, McGill’s Low Back Disorders: Evidence-Based Prevention and Rehabilitation, Lee’s The Pelvic Girdle, ed 3, and the American Physical Therapy Association’s (APTA’s) Guide to Physical Therapy Practice.4–7
HISTORY
A thorough history is a crucial first component of any evaluation. The authors assume that the reader will perform a comprehensive systems screening to rule out conditions not appropriate for therapy as described by the APTA’s Guide to Physical Therapy Practice.6
With trauma, the interview should obtain the mechanism of injury. A description of training habits or lack thereof is often helpful for evaluating chronic injuries. Changes in training programs, environment, event, or position often precede injury. Does the athlete allow enough recovery time between bouts of exercise to adapt to training? Likewise, poor- or ill-fitting equipment can also contribute to injury. As with all patients, a description of current symptoms, location, severity, and provoking factors will be helpful in evaluating athletes.4
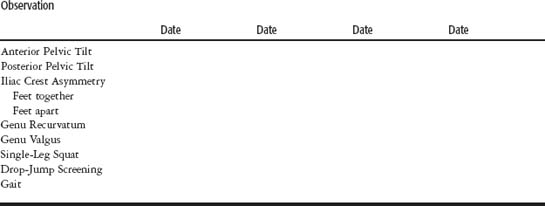
OBSERVATION
Along with history, a thorough observation of biomechanics is crucial to any physical therapy examination. This chapter focuses on observations commonly seen in athletes who have impairments of the trunk and hip CORE. The relationship of core impairments to abnormal lower extremity biomechanics was previously described in Chapter 9. Observation of the lower extremity during CORE evaluation will guide the therapist in his or her selection of CORE tests and measures.
Sagittal Plane
Abnormalities observed in lumbo-pelvic posture are a hallmark of impairment in trunk and hip motion, strength, and stabilization. Patients with normal alignment of the pelvis in the sagittal plane will demonstrate the anterior superior iliac spine at 15 degrees lower than the posterior sacroiliac spine (Figure 12-1, A).7 Comparisons of the superior iliac spines should use this normal as reference for determining anterior or posterior pelvic tilt.
An anterior tilted pelvis suggests poor recruitment of abdominal stabilizers (Figure 12-1, B). It may also suggest weak hamstrings, weak gluteales, and relative shortening of the rectus femoris. Increased lumbar lordosis will usually accompany anterior tilted pelvis. A posterior tilted pelvis suggests possible relative shortening of the hamstrings (Figure 12-1, C).8–11
Impairments in the trunk and hip CORE may also cause irregularities distally in the closed kinetic chain. Athletes with an anteriorly tilted pelvis will often display hyperextended knees or genu recurvatum.8,9
Transverse and Frontal Planes
Observation of the iliac crest will provide a rough estimate of the alignment of the pelvis in the frontal plane. Comparisons should first be made in normal stance (Figure 12-2, A). Comparisons with feet together (Figure 12-2, B) and feet apart (Figure 12-2, C) provide a quick method to screen for functional leg-length differences.7 The presence of obvious lateral trunk shifting should also be noted and warrants further testing to rule out lumbar disk pathology.4,12
Weakness in hip abductors can manifest as genu valgus or “knock knees” (Figure 12-3). Likewise, weakness of the hip external rotators can lead to excessive femoral internal rotation in stance and with gait.8,9,13–16
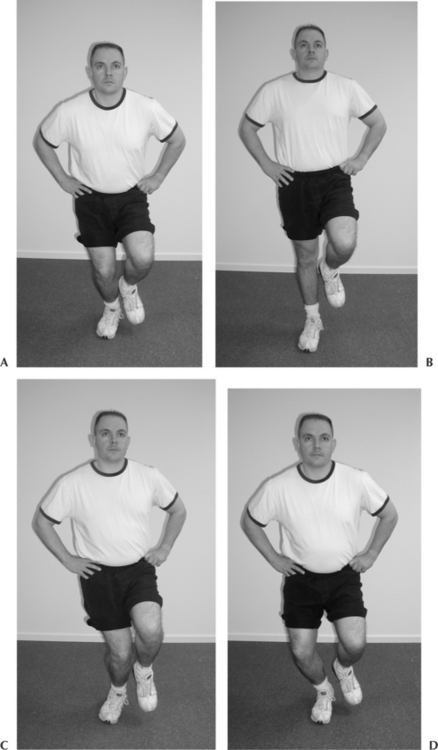
The single-legged squat is an excellent screening test for this same pattern of excessive genu valgus or hip internal rotation, or both, during lower extremity closed kinetic chain motion (Figure 12-4). Zeller et al,17 using surface electromyography (EMG) and video motion analysis, demonstrated that female college athletes exhibited greater genu valgus than male subjects with single leg squatting. Although their study does not demonstrate the validity or reliability of unassisted observation of single leg squatting as a clinical test, it does suggest it is a useful screening tool to identify athletes who require detailed motion and strength testing of the hip.17
Similarly, Noyes et al18 used computer-assisted digital video analysis to study lower extremity motion in the frontal plane during a drop-jump screening test (Figure 12-5). Subjects were fitted with markers of hip, knee, and ankle joint centers and then videotaped while performing a depth jump from a 12-inch–high box, immediately followed by a maximal vertical jump. They found this method to have excellent test-retest and within-test reliability in measuring relative hip, knee, and ankle motion in the frontal plane. Again, not everyone has access to video analysis systems, but their work suggests that observation of drop-jump for excessive genu valgus will guide the clinician to further test hip strength.18
Gait
Athletes with relative shortening of the hip flexors and accompanying weakness of hip extensors will exhibit decreased hip extension at terminal stance phase or “toe off.” Athletes who lack hip extension may also exhibit related limitation in great toe extension. Often these athletes will show decreased wear under the great toe aspect of their shoe sole and relative increased wear under the more lateral toes. These athletes may also demonstrate increased hip flexion at initial contact or “heel strike” in an effort to make up for the shorter stride length caused by limited hip extension. In patients with knee instability this will contribute to hyperextension or “giving way” of the knee.13
Athletes with marked weakness of the hip abductors will exhibit the classic Trendelenburg gait pattern. Hallmarks of the Trendelenburg gait pattern are depression of the swing phase pelvis (as the stance phase hip abductors cannot resist the pull of gravity on the unsupported side of the body).4,8,13 Athletes often find ways to compensate for a relative weakness, such as with a compensated Trendelenburg gait pattern. With this pattern the athlete exhibits increased deviation of the body in the frontal plane toward the stance leg. This causes a decrease in the moment arm of gravitational forces pulling on the unsupported half of the body and a relative decreased load on the stance phase hip abductors (Table 12-1).8,13
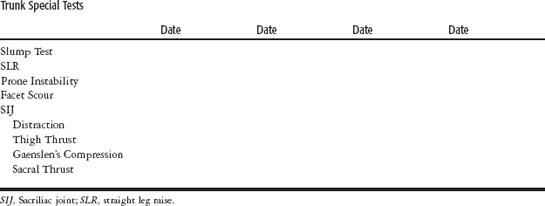
TRUNK SCREENING
Trunk Motion
Trunk flexion, extension, and side bending can be measured with goniometry, tape measure along the spinous processes, inclinometry, or visual estimation of motion. Disagreement regarding the intratester and intertester reliability of all methods currently used to measure trunk motion exists in the literature.19 Still, an attempt should be made to quantify trunk motion during evaluation. McKenzie also endorses performing knees to chest and prone prop or the sphinx position to further assess trunk flexion and extension, respectively (Figure 12-6).12,20
Peripheralization/Centralization Phenomenon
The therapist should note the presence of peripheralization (lower extremity symptoms moving distally) or centralization (moving proximally) with any of trunk motions described earlier (Table 12-2). The presence of either or both phenomena is commonly associated with lumbar disk derangement.4,12,20–22
Slump Test
Butler21 hypothesized that pathologies of the nervous system restrict the normal motion of neural tissues. These researchers advocate the slump test to detect this “adverse neural tension” via the combined movements of the trunk and lower extremity. The patient sits in full gross trunk flexion (chin to chest, slouched, bent-forward posture). The patient then slowly extends the knee and notes any reproduction of symptoms. The patient then dorsiflexes the ankle and again notes reproduction or worsening of symptoms. Many patients, even if they are healthy, will experience pain with these tests as they stress neurological tissues. The slump test is considered positive only if it reproduces the patient’s complaint of symptoms.4,21,22
Confirmation of positive testing is to see if reproduction of symptoms can be increased or decreased by manipulating the “sensitizing” aspects of the test. For example, reproduction of posterior lower extremity pain and “numbness” with slump testing would be considered a positive test. Elimination of these symptoms with plantarflexing the ankle (desensitizing the neural tissues) would further confirm a positive slump test (Figure 12-7).21
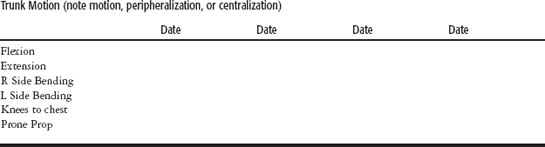
Straight Leg Raise Testing
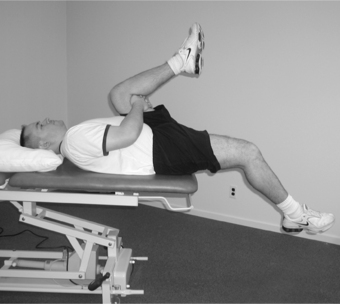
Passive straight leg raise testing is the most commonly used test for lumbar discopathy and nerve root irritation. The patient lies supine while the therapist passively raises the patient’s leg. Reproduction of low back pain with radiating pain to the posterior thigh noted before 60 degrees of elevation is associated with disk protrusion. Back pain with motion past 70 degrees is typically associated with the sacroiliac or lumbar spine joints because this range of motion causes negligible further nerve root deformation.4,20–23
Another useful special test is the opposite straight leg raise or well-leg raising test (Figure 12-8). The test procedure is the same as described earlier, but a positive test is reproduction of symptoms with raising the unaffected leg. The opposite straight leg raise has low sensitivity but high specificity for lumbar disk herniation. Thus positive testing does not rule in a significant intervertebral disk protrusion, but negative testing is useful in ruling out disk protrusion.4,20,22,23
Prone Instability Test
This test for segmental spinal instability relies on the stabilizing action of the iliocostalis lumborum pars thoracis described in Chapter 11. To perform the test, the patient is positioned in prone position on a plinth, with hips at the edge of the plinth and feet touching the floor. The therapist then applies a posterior to anterior pressure through the lumbar spinous process to be tested. The same procedure is repeated with the patient lifting his or her feet off the floor to activate the iliocostalis and thus stabilize the segment. The test is considered positive with reproduction of pain with the first position, which is reduced or eliminated with feet off the floor. Unlike the posterior shear test, the prone instability test has been shown to have good reliability (Figure 12-9).4,24
Facet Scour
Also known as the lumbar quadrant test, this test can be used as a screening tool for lumbar facet joint pathology and radiculopathy. The patient sits with arms folded across his or her chest. The therapist guides the patient into combined lumbar extension and rotation, increasing compression and shear in the facet joints. Reproduction of localized low back pain suggests possible facet joint pathology, but evidence as to the accuracy of this test is lacking.4,23 Reproduction of radiating lower extremity pain is typically associated with narrowing of the lumbar neural foramen.
Sacroiliac Joint Tests
The following sacroiliac pain provocation tests have been found to have good to excellent interrater reliability. The authors have listed multiple tests because confirmation of three or more positive provocation tests greatly improves the likelihood index with diagnosis. All of the following tests are considered positive if they reproduce the patient’s pain.20
Distraction Test
With the patient in supine position the therapist applies an anterior to posterior force to both anterior superior iliac spines (Figure 12-10).
Thigh Thrust
The patient is positioned in supine lying with one hip flexed to 90 degrees and slightly adducted. The therapist hand stabilizes the sacrum by cupping in from underneath. Using the other arm and the body, the therapist applies pressure to axially load the femur into the table, thus producing the posterior shear force on the sacroiliac joint (Figure 12-11).
Gaenslen’s Test
The patient lies supine with one leg hanging over the edge of the table. The therapist flexes the other hip and knee toward the patient’s chest. The therapist then applies firm pressure to move the legs apart and torsion the sacroiliac joint (Figure 12-12).
Compression
In sidelying, the patient flexes his or her hips and knees to 90 degrees. The examiner applies force down through the top iliac crest to compress the sacroiliac joints (Figure 12-13).
TESTS OF SACROLIAC JOINT DYSFUNCTION
Estimations of sacroiliac joint alignment or symmetry via visual estimation, palpation, inclinometry, and the assistance of calipers have all been found unreliable.24 Likewise, studies of tests commonly used to determine sacroiliac “joint dysfunction” or “positional diagnosis” show them to be unreliable (Table 12-3).25,26
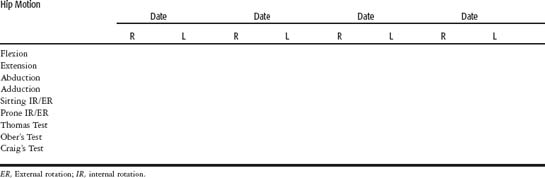
HIP TESTING
Hip Motion
Unlike trunk motion, goniometry of the lower extremity joints has been shown to be reliable to within 5 degrees of motion (Table 12-4).19 A thorough description of all hip goniometry is provided by Norkin and White.19
Table 12-4 The American Academy of Orthopedic Surgeons’ Established Mean Normal Values for Hip Motion
| AAOS Hip Range of Motion Normal Values | |
| Flexion | 120 degrees |
| Extension | 30 degrees |
| Abduction | 45 degrees |
| Adduction | 30 degrees |
| Medial Rotation | 45 degrees |
| Lateral Rotation | 45 degrees |
Stabilization of the pelvis to prevent compensation is key to obtaining accurate measurement of true hip motion. Likewise, observation of compensations often provides as much information as the actual goniometry. The authors also recommend testing of hip rotation in both the sitting and prone positions to assess the impact of hip extension on hip rotation.
Thomas Test
The authors have found that hip extension in athletes is most commonly limited by adaptive shortening of the rectus femoris. The Thomas test can be used to determine the impact of rectus femoris tightness on hip and knee position.4,8,9,11,19
The patient lies supine with his or her hips nearly off the edge of the plinth. The patient is cued to hold the contralateral knee into his or her chest to prevent lumbar hyperextension and anterior pelvic tilt compensations. With a negative test the down thigh will stay on the plinth while the knee remains flexed. With a positive test the down thigh will rise from the plinth and may be accompanied by knee extension. The therapist can record the hip and knee position with goniometry to further quantify the Thomas test (Figure 12-15). The therapist should also watch for hip abduction of the down leg or “J-sign,” which suggests iliotibial band tightness.4,11
Ober’s Test
This test assesses tissue extensibility in the iliotibial band and tensor fascia latae. The patient is positioned in sidelying with the test side up. The down leg is positioned in hip and knee flexion to stabilize the patient. The therapist extends and abducts the hip while stabilizing the pelvis to prevent a “rolling back” compensation. The Ober test was originally described with the test leg in knee flexion, but on the basis of recent anatomical studies that show knee extension further tensions the iliotibial band, the authors recommend using knee extension (Figure 12-16). The therapist then slowly allows the up leg to fall with gravity. With a positive test the up leg will remain abducted even after support has been removed.4
Craig’s Test
Craig’s test is a clinical measure of femoral antero/retroversion or the degree to which the femoral neck angulates forward or backward in the transverse plane in relation to the plane of the femoral condyles (Figure 12-17).
To perform the test the patient lies prone with the knee flexed to 90 degrees. The therapist palpates the greater trochanter of the hip while passively rotating the hip via the lower leg, stopping when the trochanter is parallel to the floor. The angle of the lower leg in relation to vertical will provide a clinical estimate of femoral anteroversion/retroversion. When the lower leg points laterally (internal hip rotation), the patient has anteroversion. The normal amount of femoral anteroversion in the adult is 8 to 15 degrees. When the lower leg points medially (hip external rotation), the patient has retroversion (Table 12-5).4
HIP AND TRUNK CORE STABILIZATION TESTS
Local Stabilization Tests
As described in Chapter 11, there has been extensive recent research into the role of the local stabilizers transversus abdominis, lumbar multifidus, and pelvic floor in preventing and rehabilitating low back pain, sacroiliac pain, and groin pain. Delays in muscle activation of these muscles are thought to allow excessive motion between bony segments of the CORE, leading to increased shear forces and inefficient use of mobilizer muscles. The majority of the research used fine-wire EMG alone or in combination with diagnostic or real-time ultrasound (RTUS) to identify abnormal muscle activation patterns in patients with low back and sacroiliac pain.27–30 However, there is a relative lack of evidence supporting many commonly used clinical assessments of local stability not dependent on technology.
Richardson et al27 propose a three-tiered system consisting of simple screening tests, clinical measures, and diagnostic measures to assess neuromuscular control of the local stabilization system.
Screening Tests
Richardson et al27 describe a “clinical assessment” of the abdominal drawing in action without spinal or pelvic motion based on observation and palpation. Although this is a commonly used evaluation method, even primary researchers acknowledge further research is necessary to validate these screening tests as evaluation tools.
Clinical Measures of Local Stability
Abdominal Drawing-in Test
This test is similar to the screening test described earlier with the addition of the use of pressure biofeedback and positioning the patient in prone. Richardson et al27 recommend instructing the patient in the motor skill to be tested by cueing the patient to “draw in the abdominal wall” and educating the patient in the corset-like anatomy of the transversus abdominis. It may also be necessary to begin by instructing the patient in the kneeling-on-all-fours position before actual testing.
According to Richardson et al,27 a correct isolated transversus abdominis contraction will reduce pressure in the biofeedback unit by 6 to 10 mm Hg as the drawing-in action of the transversus abdominis moves the abdominal wall away from the pressure bladder. A drop in pressure less than 6 mm or an increase in pressure indicates a “poor” transversus abdominis contraction. If correct recruitment of the transversus abdominis is observed, then muscular endurance is assessed with 10-second isometric holds for up to 10 repetitions.
Hodges et al31 examined the relationship between laboratory study of local stabilizers and clinical testing used to assess local stabilization patterns. They reported “good agreement” between subjects with a poor ability to decrease pressure with the drawing-in test and those with delayed transversus abdominis activation in the laboratory. However, to the authors’ knowledge Hodges et al did not statistically demonstrate this relationship.31
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree