TABLE 38.2 Common Nonarticular Causes of Pain After TKA
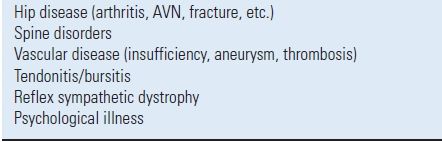
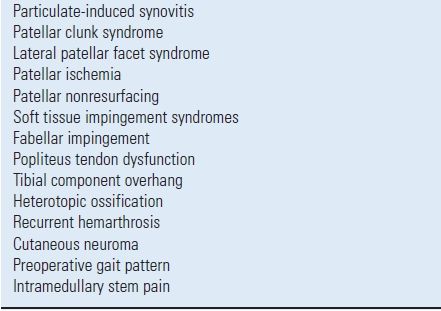
TABLE 38.3 Less Common Causes of Pain After TKA
INVESTIGATIVE METHODS
To completely evaluate the painful TKA, one needs to perform a thorough history and physical examination as well as both laboratory and radiographic testing.
History and Physical Examination When obtaining historical information, it is important to precisely define the character of the pain that the patient is experiencing. One needs to determine the exact location of the pain and whether it is well-localized or radiating. Additionally, it should be determined when the pain most commonly occurs, how long it lasts, are there any exacerbating or ameliorating phenomena, and lastly, how intense is the pain.
It is also valuable to investigate the pain pattern. If the patient was free of pain initially following TKA and developed pain months to years later, diagnoses such as component loosening or failure, late ligamentous instability, or a hematogenously based infection should be considered. If the patient was never pain free following TKA, diagnoses such as acute infection, instability, prosthetic malalignment, or nonarticular causes should be entertained. A patient with prosthetic loosening typically has increased pain with weight bearing, which is reduced with rest. Those with infection will commonly present with pain both with rest or activity and may have experienced fever, chills, or recent invasive procedures, particularly involving the dentition, gastrointestinal, or genitourinary tracts. Factors associated with an increased infection risk include advanced age, poor nutrition,1 obesity,2 corticosteroid use,3 skin ulcerations, prolonged preoperative hospitalization, and various medical conditions including rheumatoid arthritis,4 diabetes mellitus,5 psoriatic arthritis,6 and a previous knee infection.7
Physical examination should include a careful examination of the skin, particularly looking for erythema or warmth. The knee should be examined for alignment, stability, range of motion, and the presence of effusion or crepitus. The knee should also be palpated to discern areas of point tenderness, which may represent conditions such as tendonitis, bursitis, or cutaneous neuromata. Lastly, one must study the patient’s gait pattern for limp or coronal plane thrust, which may be indicative of malalignment or ligamentous instability. Gait analysis before and after TKA has demonstrated an increased incidence of anterior knee pain following TKA in those subjects with higher preoperative external flexion moments during the early midstance phase of gait.8 The spine and hip should be thoroughly examined to rule out conditions that may cause referred pain to the knee. Lastly, a complete neurological and vascular examination is imperative.
Laboratory Analysis The primary focus of laboratory analysis is to distinguish between septic and aseptic causes of the knee pain. Commonly utilized laboratory tests include a complete blood count (CBC) with differential, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and knee aspiration for cell count and culture. The ESR is typically elevated for 3 to 6 months following an uncomplicated total joint arthroplasty.9 Barrack et al.10 evaluated the use of preoperative ESR in a series of revision TKA patients. In those with documented infection, the average ESR was 57 mm/h in contrast to 27 mm/h in noninfected patients. An ESR of >30 mm/h demonstrated a sensitivity of 80%, specificity of 62.5%, a positive predictive value of 47.1%, and a negative predictive value of 88.2% for diagnosis of infection.
CRP is an acute phase protein, which is another measure of inflammation. Its advantage over an ESR is that it routinely returns to normal values by 3 weeks following TKA. CRP sensitivity and specificity values are similar to an ESR. The value of CBC, ESR, and CRP testing is enhanced when used in combination.11 If all three tests are elevated, the likelihood of infection is substantial.
Knee aspiration has been shown to be a valuable tool in evaluation of the painful TKA. To maximize the accuracy of knee aspiration, early plating on culture media is critical. It is wise to consider multiple knee aspirations for culture if the index aspiration is negative, yet the suspicion of infection is high.10 Barrack et al.10 also studied the value of knee aspiration in determination of infection in 69 cases of revision TKA and observed a sensitivity of 65.4%, a specificity of 96.1%, an accuracy of 85.7%, a positive predictive value of 89.5%, and a negative predictive value of 84.5%. Mason et al.12 evaluated preoperative knee aspirates of 86 patients undergoing revision TKA, evaluating white blood cell counts and percentage of polymorphonucleocytes (PMN). Infection was diagnosed in 36 cases while 50 patients were not infected. A high likelihood of infection was noted if the aspirate contained >2,500 white blood cells per high-powered field in conjunction with a differential count of >60% PMN. Using these criteria, this evaluation demonstrated a sensitivity of 98% and a specificity of 95% for diagnosis of infection. In an additional evaluation of knee aspiration, Duff et al.13 reported on 43 knee aspirations of 19 infected and 24 noninfected TKAs. They observed a 100% sensitivity, specificity, and accuracy in determination of knee infection, further supporting the use of this procedure in the evaluation of the painful TKA.
Radiographic Evaluation Available radiographic options for evaluation of the painful TKA include plain radiographs, stress views, arthrography, nuclear medicine scanning, and magnetic resonance imaging (MRI). Routine standing anteroposterior and lateral radiographs should be obtained in each case to assess component fixation, position, sizing, the presence of component failure, or periprosthetic osteolysis. A Merchant patellar view14 is important to assess for longitudinal patellar fractures, centralization of the patella, and osseous coverage of the patella by the implanted patellar component. The author also recommends a full-length radiograph of the affected lower extremity to detect distant osseous problems such as malunion, tumor, stress fracture, etc., that would not be detected on routine knee radiographs. Additional radiographs to consider are views of the pelvis to detect hip pathologic conditions such as stress fracture or medial hip osteoarthritis which has been shown to cause referred pain to the knee (via the obturator nerve). If knee pain is unexplained, it is wise to review the original prearthroplasty radiographs to ensure substantial arthritic change was present preoperatively to confirm that the knee is the true source of pain. A key in evaluation of plain radiographs is sequential analysis over a period of years, looking for progressive radiolucent lines at the fixation interface, component migration, osteolysis, or other radiographic changes.
Stress radiographs can be helpful to detect subtle ligamentous instability. Varus and valgus stress views are helpful to diagnose collateral ligamentous instability. Posterior cruciate ligament (PCL) laxity can often be detected by obtaining weight-bearing lateral views in both full extension and maximum flexion. If the femorotibial contact position in deep flexion is positioned substantially more anteriorly than in full extension, some degree of instability of the PCL is present. This finding can similarly be determined with the use of weight-bearing video fluoroscopy15 (Fig. 38-1). Patients with chronic PCL instability typically present with chronic pain, often during deep flexion activities such as stair descent or chair transfer. Examination of these subjects often demonstrates an intra-articular effusion, posterior tibial subluxation (posterior sag sign), and anterior tenderness over the extensor mechanism, pes anserinus tendon complex, and the distal iliotibial band.16 Fehring and McAvoy17 have demonstrated that fluoroscopically guided radiographs are often required to detect subtle component loosening. The fluoroscope is used to facilitate x-ray beam placement perfectly tangential to the fixation interface in order to determine the status of prosthesis fixation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








