Chapter 11 Evaluation of Glenohumeral, Acromioclavicular, and Scapulothoracic Joints in the Overhead-Throwing Athlete
After studying this chapter, the reader will be able to do the following:
One of the key concepts in upper extremity rehabilitation is the scapular plane concept. The scapular plane has ramifications in treatment, evaluation, and even in functional activity in sports. According to Saha,1 the scapular plane is defined as being 30 degrees anterior to the coronal or frontal plane of the body. Placement of the glenohumeral joint in the scapular plane optimizes the osseous congruity between the humeral head and the glenoid and is widely recommended as an optimal position for both the performance of various evaluation techniques, as well as during many rehabilitation exercises.1,2 With the glenohumeral joint placed in the scapular plane, bony impingement of the greater tuberosity against the acromion does not occur due to the alignment of the tuberosity and acromion in this orientation.1
Another important general concept of relevance for this chapter is that of muscular force couples. One of the most important biomechanical principles in shoulder function is the deltoid rotator cuff force couple.3 This phenomenon, known as a “force couple,” can be defined as two opposing muscular forces working together to enable a particular motion to occur, with these muscular forces being synergists, or agonist/antagonist pairs.3 The deltoid muscle provides force primarily in a superior direction when contracting unopposed during arm elevation.4 The muscle tendon units of the rotator cuff must provide both a compressive force, as well as an inferiorly or caudally directed force to minimize superior migration and minimize contact or impingement of the rotator cuff tendons against the overlying acromion.3 Failure of the rotator cuff to maintain humeral congruency leads to glenohumeral joint instability, rotator cuff tendon pathology, and labral injury.5 Imbalances in the deltoid rotator cuff force couple, which primarily occur during inappropriate and unbalanced strength training, as well as through repetitive overhead sport activities, can lead to development of the deltoid without concomitant increases in the rotator cuff strength and increase the superior migration of the humeral head provided by the deltoid, leading to rotator cuff impingement.
Additionally, the serratus anterior and trapezius force couple is the primary muscular stabilization and prime mover of upward rotation of the scapular during arm elevation. Bagg and Forest6 have shown how the upper trapezius and serratus anterior function during the initial (0 to 80 degrees of) arm elevation, providing upward scapular rotation and stabilization. Due to a change in the lever arm of the lower trapezius that occurs during the lateral shift of the scapulothoracic instantaneous center of rotation with arm elevation, the lower trapezius and serratus anterior function as the primary scapular stabilizer in phases II and III (80 to 140 degrees) of elevation.6 Knowledge of the important muscular force couples in the human shoulder and scapulothoracic region is imperative and can lead to proper evaluation and ultimately treatment via strengthening and monitoring proper strength balance of these important muscular pairings.
MUSCULAR AND RANGE OF MOTION TESTING IN THE SHOULDER IN THE OVERHEAD ATHLETE
The most clinically relevant method used to assess strength of the shoulder girdle is manual muscle testing (MMT). Since its initial development in the early 1900s during the study of muscle function in patients with poliomyelitis, MMT has become a standard practice during the physical evaluation of patients with both neurological and orthopaedic injuries.7,8 Although several limitations exist in the use of MMT in the athletic shoulder, the application of this important technique has high clinical relevance, especially in the absence of more sophisticated methodology, such as hand-held dynamometers or isokinetic testing.9
Key Positions Used for Manual Muscle Testing of the Rotator Cuff
Kelly et al10 used electromyography (EMG) to determine the optimal position for testing the muscles of the rotator cuff in human subjects. Four criteria were used to establish which position was optimal for each rotator cuff muscle. These were: maximal activation of the muscle, minimal contribution from shoulder synergists, minimal provocation of pain, and good test-retest reliability. Kelley et al10 found the optimal muscle testing position for the supraspinatus to be at 90 degrees of elevation, with the patient in a seated position. The scapular plane position was used (in this research this represented 45 degrees of horizontal adduction from the coronal plane) with external rotation of the humerus such that the forearm was placed in neutral and the thumb was pointing upward toward the ceiling. This position was termed the Full Can Testing position. Another frequently used test position to assess the strength of the supraspinatus muscle-tendon unit is termed the Empty Can Test. This test position has been advocated by Jobe11 and has been found to have high levels of supraspinatus muscular activation using indwelling EMG.12
Kelly et al10 reported the optimal position to test for infraspinatus strength is with the patient in a seated position, with 0 degrees of glenohumeral joint elevation and in 45 degrees of internal rotation from neutral. An alternative position for testing the infraspinatus has been recommended by Jenp et al.13 They recommend testing the infraspinatus in 90 degrees of elevation in the sagittal plane, with the arm in half maximal external rotation. The author of this chapter highly recommends the use of the 90-degree abducted position for testing the infraspinatus in a functionally specific position and 90 degrees of external rotation as pictured (Figure 11-1). To test the teres minor muscle, use of the Patte test to best isolate the teres minor has been recommended by both Walch et al14 and Leroux et al.15 The position of the glenohumeral joint for the Patte test16 to isolate the teres minor has been reported as 90 degrees of glenohumeral joint abduction in the scapular plane and 90 degrees of external rotation.
Finally, Kelley et al10 reported the optimal position for subscapularis muscular activation to be in the Gerber lift-off position.17 This position involves placing the dorsal aspect of the hand in lumbar lordosis and pressing posteriorly away from the back.
Relationship between Manual Muscle Testing and Isokinetic Testing
Ellenbecker18 compared isokinetic testing of the shoulder internal and external rotators to MMT in 54 subjects exhibiting manually assessed, symmetrical, normal-grade (5/5) strength. Isokinetic testing found 13% to 15% bilateral differences in external rotation and 15% to 28% bilateral differences in internal rotation. Of particular significance was the large variability in the size of this mean difference between extremities, despite bilaterally symmetrical MMT. The use of MMT is an integral part of a musculoskeletal evaluation. MMT provides a time efficient, gross screening of muscular strength of multiple muscles using a static, isometric muscular contraction, particularly in situations of neuromuscular disease or in patients with large muscular strength deficits. The limitations of MMT appear to be most evident when only minor impairment of strength is present, as well as in the identification of subtle isolated strength deficits. Differentiation of agonist/antagonist muscular strength balance is also complicated using manual techniques, as opposed to using isokinetic instrumentation.18
Use of Isokinetic Testing for the Shoulder Complex
The initial position used for isokinetic testing of the shoulder typically involves the modified base position. The modified base position is obtained by tilting the dynamometer approximately 30 degrees from the horizontal base position.19 The patient’s glenohumeral joint is placed in 30 degrees abduction and 30 degrees forward flexion into the plane of the scapula or scaption, and with a 30-degree diagonal tilt of the dynamometer head from the transverse plane. This position has also been termed the (30/30/30) internal/external rotation position by Davies.19 The modified base position places the shoulder in the scapular plane 30 degrees anterior to the coronal plane.1 The scapular plane is characterized by enhanced bony congruity and a neutral glenohumeral position, which results in a midrange position for the anterior capsular ligaments and enhances the length tension relationship of the scapulohumeral musculature.1 This position does not place the suprahumeral structures in an impingement situation and is well tolerated by patient populations.19
Isokinetic testing using the modified base position requires consistent application of the patient to the dynamometer. Studies have demonstrated significant differences in internal and external rotation strength, with varying degrees of abduction, flexion, and horizontal abduction/adduction of the glenohumeral joint.20–22 The modified base position uses a standing patient position on many dynamometer systems, which can lead to compromises in both glenohumeral joint isolation and test-retest reliability. Despite these limitations, valuable data can be obtained early in the rehabilitative process using this neutral, modified base position, which is a safe, comfortable position for most patients with most pathologies and postsurgical considerations.9,19 Knops et al23 conducted a test-retest reliability study of the modified neutral position for internal/external rotation of the glenohumeral joint. This position of testing produced high test-retest reliability, with intraclass correlation coefficients ranging from 91 to 96.
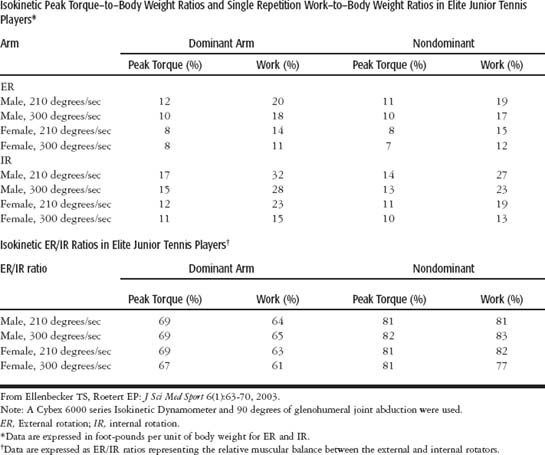
The most functionally specific isokinetic testing position for the assessment of internal and external rotation strength is performed with 90 degrees of glenohumeral joint abduction (Figure 11-2). Specific advantages of this test position are greater stabilization in either a seated or supine test position on most dynamometers, as well as placement of the shoulder in an abduction angle corresponding to the overhead-throwing position used in many sport activities.24 Utilization of the 90-degree abducted position of isokinetic strength assessment will more specifically address muscular function required for overhead activities.25 Descriptive data profiles for throwing athletes,26,27 as well as for elite junior tennis players,28 are listed in Tables 11-1 through 11-3. These data provide objective information regarding the normal torque to body weight ratios, as well as external/internal rotation ratios used in the interpretation of instrumented upper extremity strength testing. Muscular imbalances due to the repetitive and forceful internal rotation during the acceleration of the throwing motion, tennis serve, and forehand can lead to unilateral muscular imbalances on the dominant arm between the external and internal rotators and jeopardize optimal muscular stabilization.26–28 Use of instrumented testing is an important part of a comprehensive evaluation of the throwing athlete.9
Table 11-1 Isokinetic Data from the Biodex Isokinetic Dynamometer from Professional Baseball Pitchers for Shoulder Internal/External Rotation
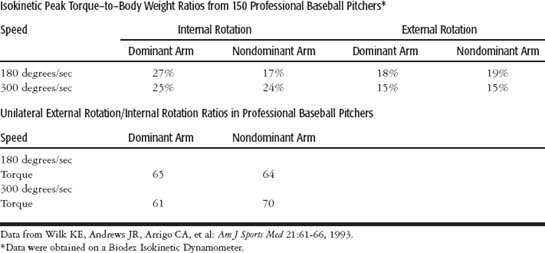
Table 11-2 Isokinetic Data from the Cybex Isokinetic Dynamometer from Professional Baseball Pitchers for Shoulder Internal/External Rotation
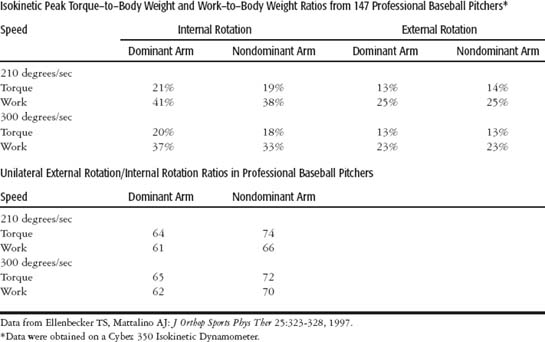
Table 11-3 Isokinetic Data from the Cybex 6000 Isokinetic Dynamometer for Shoulder Internal/External Rotation
Isokinetic dynamometers have also been extensively used in the measurement of muscular fatigue.29,30 Isokinetic muscular fatigue tests typically consist of measuring the number of repetitions of maximum effort that are required to reach a 50% reduction in torque, work, or power from the beginning to the end of a certain time period or number of contractions. Relative fatigue ratios consist of comparing the work in the last half of a preset number of muscular contractions with the work performed in the first half.19,30
Relative fatigue ratios have been studied in elite tennis players and have produced clinically applicable information. Ellenbecker and Roetert29 measured the relative fatigue response in the internal and external rotators of 72 elite junior tennis players, using 20 maximal effort concentric testing repetitions at 300 degrees per second in the supine position, with 90 degrees of glenohumeral joint abduction. They found the external rotators to fatigue to a level of 69%, while the internal rotators only fatigued to a level of 83%. This is significant, due to the substantial contribution the external rotators play in humeral deceleration during overhead throwing and serving activities,24 as well as dynamic stabilization of the humeral head in the glenoid.25 Because the external rotators appear to fatigue more quickly and to a greater extent than the internal rotators, this further supports the current concepts of preventative conditioning and balancing of the shoulder external rotators in unilaterally dominant upper extremity athletes.
Range of Motion Testing
Discussing range-of-motion testing in depth is beyond the scope of this chapter; however, the measurement of one of the most important movement patterns (humeral rotation) will be covered, along with the concept of total rotation range of motion (ROM). A thorough objective documentation of the cardinal movements of the glenohumeral joint is recommended, and the reader is referred to two texts31,32 for a more complete discussion.
Technique for Measurement of Humeral Rotation
Several important principles should be discussed to optimize the measurement of humeral rotation in the overhead-throwing athlete. One of these is the contribution of the scapulothoracic joint to glenohumeral motion, which has been widely documented.3,33 This is one of the variables that can lead to extensive variation of rotational measurement in the human shoulder. In a study by Ellenbecker et al,34 active rotational ROM measures were taken bilaterally in 399 elite junior tennis players using two differing measurement techniques and a universal goniometer. Two hundred fifty-two subjects were simply measured in the supine position for internal and external rotation with 90 degrees of glenohumeral joint abduction using no attempt to stabilize the scapula. One hundred forty-seven elite junior tennis players were measured for internal and external rotation active ROM in 90 degrees of glenohumeral joint abduction using scapular stabilization. This stabilization was provided by a posteriorly directed force applied by the examiner’s hand placed over the anterior aspect of the shoulder, over the anterior acromion and coracoid process (Figure 11-3). Results of the two groups showed significantly less internal rotation ROM when using the measurement technique with scapular stabilization (18% to 28% reduction in ROM). Changes in external rotation ROM were smaller between groups, with 2% to 6% reductions in active ROM measured.
One common finding confirmed in this research is the finding of significantly less (≈10 to 15 degrees) dominant arm glenohumeral joint internal rotation in elite junior tennis players.35,36 The significance in this present research, however, lies in the fact that this difference between extremities in internal rotation ROM was only identified in the condition where the scapula was stabilized. Failure to stabilize the scapula did not produce glenohumeral joint internal rotation ROM measurements that identified a deficit. Only measuring this population with scapular stabilization identified the characteristic ROM limitation in internal rotation. This study clearly demonstrates the importance of using consistent measurement techniques when documenting ROM of glenohumeral joint rotation. On the basis of these study results, the author of this chapter highly recommends the use of scapular stabilization during the measurement of humeral rotation to obtain more isolated and representative values of shoulder rotation.
Total Rotation Range of Motion Concept
One final concept to be discussed in this section on ROM measurement is the total rotation ROM concept. This concept simply combines the glenohumeral joint internal and external rotation ROM measure by summing the two numbers to have a numerical representation of the total rotation ROM available at the glenohumeral joint. Recent research by Kibler et al37 and Roetert et al38 has identified decreases in the total rotation ROM arc in the dominant extremity of elite tennis players correlated with increasing age and number of competitive years of play. Most recently, Ellenbecker et al39 measured bilateral total rotation ROM in professional baseball pitchers and elite junior tennis players. The findings of this study showed the professional baseball pitchers to have greater dominant arm external rotation and significantly less dominant arm internal rotation, when compared with the contralateral nondominant side. The total rotation ROM, however, was not significantly different between extremities in the professional baseball pitchers (145 degrees dominant arm, 146 degrees nondominant arm). This research shows that, despite bilateral differences in the actual internal or external rotation ROM, or both, in the glenohumeral joints of baseball pitchers, the total arc of rotational motion should remain the same.
In contrast, Ellenbecker et al39 tested 117 elite male junior tennis players. In the elite junior tennis players, significantly less internal rotation ROM was found on the dominant arm (45 degrees vs. 56 degrees), as well as significantly less total rotation ROM on the dominant arm (149 degrees vs. 158 degrees). The total rotation ROM did differ between extremities (Table 11-4). Approximately 10 degrees less total rotation ROM can be expected in the dominant arm of the uninjured elite junior tennis player, as compared with the nondominant extremity.
Table 11-4 Bilateral Comparison of Isolated and Total Rotation Range of Motion from Professional Baseball Pitchers and Elite Junior Tennis Players
| Subjects | Dominant Arm | Nondominant Arm |
|---|---|---|
| Baseball Pitchers | ||
| ER | 103.2 ± 9.1 (1.34) | 94.5 ± 8.1 (1.19) |
| IR | 42.4 ± 15.8 (2.33) | 52.4 ± 16.4 (2.42) |
| Total rotation | 145.7 ± 18.0 (2.66) | 146.9 ± 17.5 (2.59) |
| Elite Junior Tennis Players | ||
| ER | 103.7 ± 10.9 (1.02) | 101.8 ± 10.8 (1.01) |
| IR | 45.4 ± 13.6 (1.28) | 56.3 ± 11.5 (1.08) |
| Total rotation | 149.1 ± 18.4 (1.73) | 158.2 ± 15.9 (1.50) |
ER, External rotation; IR, internal rotation.
From Ellenbecker TS, Roetert EP, Bailie DS, et al: Med Sci Sports Exerc 34(12):2052-2056, 2002. All measurements are expressed in degrees. Standard error of the mean in parentheses.
Utilization of normative data from population specific research, such as this study, can assist clinicians in interpreting normal ROM patterns and identify when sport-specific adaptations or clinically significant maladaptations are present. The data in this table contain the descriptive data from the professional baseball pitchers and elite junior tennis players.39 Further research on additional subject populations is necessary to further outline the total rotation ROM concept.
This total rotation ROM concept can be used as illustrated to guide the clinician during rehabilitation, specifically in the area of application of stretching and mobilization, to best determine what glenohumeral joint requires additional mobility and which extremity should not have additional mobility, due to the obvious harm induced by increases in capsular mobility and increases in humeral head translation during aggressive upper extremity exertion.
Burkhart et al5 describe this loss of internal rotation ROM as GIRD, or g lenohumeral i nternal r otation d eficit. Because a loss of internal rotation in the dominant shoulder is common in the glenohumeral joint of the elite thrower, Burkhart et al5 have further described what they term as an acceptable level of GIRD as less than 20 degrees of limitation of internal rotation compared with the nonthrowing shoulder, or less than 10% loss of total rotation ROM compared with the contralateral shoulder. Burkhart et al5 further state that approximately 90% of all throwers with symptomatic GIRD (>25 degrees of internal rotation loss compared with the contralateral nonthrowing shoulder) respond favorably to a compliant posterior-inferior capsular stretching program and reduce GIRD to the acceptable levels. Use of the “sleeper stretch” has been advocated by these authors5 and consists of the athlete sidelying on the dominant shoulder in varied positions of glenohumeral joint abduction while internally rotating the glenohumeral joint, using body weight to stabilize the lateral border of the scapula. Further research using controlled experimental designs is necessary to better understand the effectiveness of stretching for the throwing shoulder.
The loss of internal rotation ROM is significant for several reasons. The relationship between internal rotation ROM loss (tightness in the posterior capsule of the shoulder) and increased anterior humeral head translation has been scientifically identified.40,41 The increase in anterior humeral shear force reported by Harryman et al42 was manifested by a horizontal adduction cross-body maneuver, similar to that incurred during the follow-through of the throwing motion or tennis serve. Tightness of the posterior capsule has also been linked to increased superior migration of the humeral head during shoulder elevation.43
Recent research by Koffler et al44 studied the effects of posterior capsular tightness in a functional position of 90 degrees of abduction and 90 degrees or more of external rotation in cadaveric specimens. They found, with imbrication of either the inferior aspect of the posterior capsule or imbrication of the entire posterior capsule, that humeral head kinematics were changed or altered. In the presence of posterior capsular tightness, the humeral head will shift in an anterior superior direction, as compared with a normal shoulder with normal capsular relationships. With more extensive amounts of posterior capsular tightness, the humeral head was found to shift postero-superiorly. These effects of altered posterior capsular tensions experimentally representing in vivo posterior glenohumeral joint capsular tightness highlight the clinical importance of using a reliable and effective measurement methodology to assess internal rotation ROM during examination of the shoulder. Additionally, Burkhart et al5 have clinically demonstrated the concept of posterior superior humeral head shear in the abducted externally rotated position with tightness of the posterior band of the inferior glenohumeral ligament.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree