Evaluation and Management of Nerve Injuries Following Soft Tissue and Bony Trauma
Susan E. Mackinnon
Renata V. Weber
Nerve injuries associated with orthopaedic trauma are usually due to avulsion, crush, or direct laceration of the affected nerve. The extent of the injury can vary from focal lacerations to diffuse nerve root avulsions. In general, the greater the local soft tissue destruction, the more complex the nerve injury and the less likely for return of normal function.
Table 5-1. Typical Nerve Injury Patterns | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Classification of Nerve Injuries
Nerve injuries can occur with varying degree of soft tissue injury and may be isolated to the nerve(s) or associated with fractures, dislocations, or fracture-dislocations. From an evaluation and treatment perspective, nerve injuries can be grouped as (a) stretch and avulsion injuries, (b) crush and compression injuries, and (c) penetrating injuries. Table 5-1 lists the typical nerve injury patterns and their significance with respect to assessment and treatment.
Originally, peripheral nerve injuries were described by Sir Herbert Seddon in 1943 as neurapraxia, axonotmesis, and neurotmesis (1). The classification was later expanded by Sunderland and further defined by Mackinnon to include six degrees of injuries (Table 5-2) (2). First degree (neurapraxia) and second degree (axonotmesis) injuries recover spontaneously, the latter at the classic rate of 1 in/month or 1 to 1.5 mm/day (3). Third degree injuries must regenerate through some amount of scar tissue, thus recovery is variable and less than normal depending on the amount of scar tissue around the nerve. In fourth degree injuries, also known as a neuroma-in-continuity, regeneration is blocked by scar tissue within the fascicles and recovery is usually very poor or does
not occur. A fifth degree nerve injury (neurotmesis) is a transection of the nerve, which always will require surgical repair, while the sixth degree nerve injury encompasses a variety of nerve injuries within a single nerve. The difficulty with surgical correction of a sixth degree injury is limiting the repair to the fascicles affected by fourth and fifth degree damage and not damaging the fascicles with the potential for spontaneous recovery (Fig. 5-1).
not occur. A fifth degree nerve injury (neurotmesis) is a transection of the nerve, which always will require surgical repair, while the sixth degree nerve injury encompasses a variety of nerve injuries within a single nerve. The difficulty with surgical correction of a sixth degree injury is limiting the repair to the fascicles affected by fourth and fifth degree damage and not damaging the fascicles with the potential for spontaneous recovery (Fig. 5-1).
Table 5-2. Classification of nerve injury | ||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
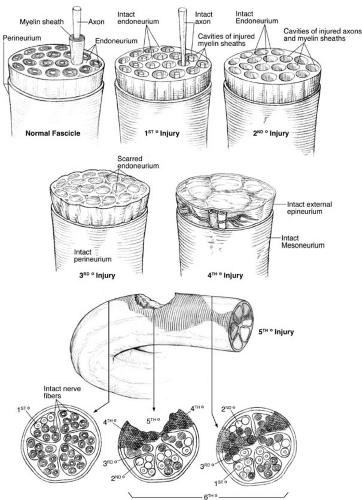 FIGURE 5-1 Schematic depiction of nerve injuries from first through sixth degree. (By permission of Mayo Foundation for Medical Education and Research. All rights reserved.) |
Stretch and Nerve Avulsion Injuries
Traction on a nerve can result in a mild stretch injury to the axon with preservation of the basal lamina. The Schwann cells around both myelinated and unmyelinated fibers may be locally injured and, until the cells are replaced from surrounding Schwann cells, will cause a conduction block. Such injuries are classified as first degree injuries and recover completely. As the pulling forces increase across the nerve, the basal lamina, the endoneurium, and perineurium become injured. As the nerve heals, internal scaring of the nerve may occur in some of the fascicles, leading to incomplete recovery. Grossly, the nerve will appear intact as the epineurium is usually not violated. Occasionally, neurolysis or even an internal neurolysis of the injured nerve may improve recovery as long as there is evidence that the nerve recovery is being hindered by scar surrounding the nerve, rather than internal scar to the fascicles.
Nerves that are stretched beyond the breaking point will avulse, resulting in gross disruption of the epineurium, perineurium, and endoneurium. A neuroma will typically form at the proximal end, and these injuries are treated with excision of the neuroma and primary repair when possible. Often, if the time from injury is greater than 2 weeks, even excessive mobilization of the nerve ends will not be enough to overcome the resulting gap that occurs when the unhealthy neuroma tissue at both ends is resected. A nerve graft is then needed to repair the gap.
In extreme cases, nerves can be avulsed from their insertion into the spinal cord. In the past, these injuries were treated conservatively. Once no further nerve recovery was noted, tendon transfers were used to restore the residual functional deficits (4). More recently, the introduction of nerve transfers allows for rewiring of nonfunctioning nerves by using local uninjured nerves to restore electrical continuity to the deinnervated muscles (5). Tendon transfers may be used to augment the nerve transfers once maximum recovery is achieved (6).
Nerves avulsed at the neuromuscular junction present a different problem. Nerves that are injured just prior to entering the muscle, or shortly thereafter, may still be repaired or grafted in most cases as long as a large enough nerve stump is found. Motor nerves that are avulsed from the muscle bellies are treated by implanting proximal nerve, when available, directly into the muscle with the hope that some of the fibers will find a neuromuscular junction and reinnervate at least part of the muscle. Some studies (7) show as good as M4 motor recovery 1 to 2 years after direct nerve to muscle neurotization; however, experimental studies do not support these findings. Rather, recovery is much less than a nerve coaptation would produce (8).
Crush Injuries
Crush injuries comprise the most common peripheral nerve injury to the extremity. External compression may be complicated by increased internal pressure from hematomas, fractures, and local tissue edema. When minor, this may cause a temporary neurapraxia, but with greater compression the likelihood of permanent injury increases. The most severe consequence of a crush injury is the progression to compartment syndrome. Often an early sign of impending compartment syndrome is a decrease in vibration sensibility (9). Compartment syndrome of the upper extremity and lower extremity are surgical emergencies and are reviewed separately within this text.
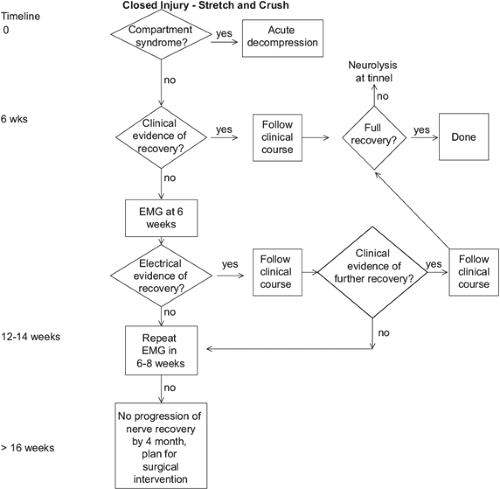
Nerve compression injuries may also develop distal to the actual soft tissue trauma. Local edema and inflammation after injury can exacerbate a preexisting condition, such as a mild carpal tunnel turning into an acute event after a distal radius fracture. Occasionally, on a case by case basis, surgical decompression is necessary, even though the majority will resolve spontaneously. Likewise, an anterior cruciate ligament tear of the knee requiring reconstruction or repair may precipitate an acute foot drop postoperatively despite the deep peroneal nerve being usually uninjured. Some surgeons postulated that intraoperative positioning of the limb may be a factor in the late development of palsy (10); however, we believe that local tissue inflammation probably exacerbates a preexisting condition that manifests itself as a postoperative foot drop. When conservative nonoperative measures do not lead to sufficient improvement in nerve function after 2 to 3 months, decompression of the peroneal nerve should be considered (11). Figure 5-2 shows an algorithm for treatment of closed nerve injuries.
Penetrating Injuries
Blunt penetrating trauma is usually more locally destructive than a sharp injury. Often nearby structures such as blood vessels and tendons are injured in addition to the nerve. However, the size of a sharp laceration, such as with glass or a knife, can mislead the surgeon into underestimating the extent of injury. A seemingly small skin laceration may in fact extend under the surface and result in
a bigger injury than would be expected from the external size of the wound. Exploration is imperative if a nerve palsy is present, as the likelihood that the nerve is partially or completely transected is high. It is recommended to explore these injuries semi-electively within the first 2 weeks. The further from the time of injury, the more likely a nerve graft will be needed to overcome the resulting nerve gap. In the event of a penetrating trauma with an associated vascular injury, immediate exploration is warranted. Often the nerve injury is overlooked and not identified in the face of a more urgent vascular injury. In such cases the functional deficit may be first noticed postoperatively, when it is unclear if the nerve injury is from the inciting event, iatrogenic during the repair of the vascular injury, or secondary to edema or hematoma. While a CT scan or MRI may be helpful to evaluate for the latter, internal scarring of the nerve may not always be seen.
a bigger injury than would be expected from the external size of the wound. Exploration is imperative if a nerve palsy is present, as the likelihood that the nerve is partially or completely transected is high. It is recommended to explore these injuries semi-electively within the first 2 weeks. The further from the time of injury, the more likely a nerve graft will be needed to overcome the resulting nerve gap. In the event of a penetrating trauma with an associated vascular injury, immediate exploration is warranted. Often the nerve injury is overlooked and not identified in the face of a more urgent vascular injury. In such cases the functional deficit may be first noticed postoperatively, when it is unclear if the nerve injury is from the inciting event, iatrogenic during the repair of the vascular injury, or secondary to edema or hematoma. While a CT scan or MRI may be helpful to evaluate for the latter, internal scarring of the nerve may not always be seen.
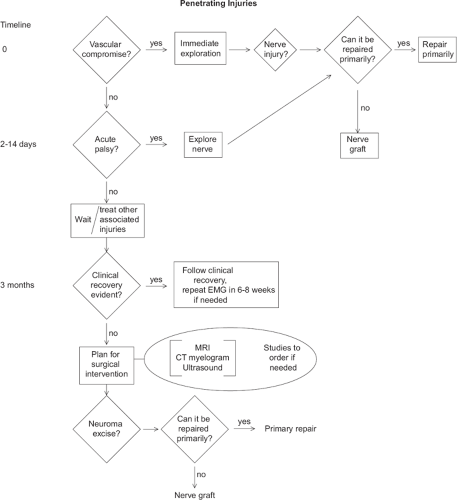
Blunt penetrating injuries are initially treated conservatively, similar to closed crush and stretch injuries, because they are may recover spontaneously. The local tissue edema often causes a neurapraxia that resolves; however, those that do not recover after 3 months should be evaluated by electrodiagnostic studies and treated as a traction injury. Figure 5-3 shows an algorithm for managing nerve injuries and the timing of additional studies.
Two specific blunt penetrating injuries deserve special mention: gun shot wounds and electrical injuries. Gun shot injuries present a unique problem since the trajectory of the bullet is unpredictable. The type, caliber, and velocity of the bullet each play a role in tissue destruction (12). The belief that the higher velocity bullet causes more tissue destruction can lead to early massive debridement; however, current recommendations are for judicious debridement and staged exploration,
as in crush injuries (13). In fact, a low velocity bullet like a slug that fragments and stays in the soft tissue will more likely lead to infection and local tissue destruction than an Army issue missile that passes through the tissue with relative ease (14).
as in crush injuries (13). In fact, a low velocity bullet like a slug that fragments and stays in the soft tissue will more likely lead to infection and local tissue destruction than an Army issue missile that passes through the tissue with relative ease (14).
Electrical injuries that are not severe enough to cause death from heart arrhythmia and respiratory paralysis cause vigorous nerve stimulation which leads to paralysis and vasospasm. Massive muscle contractions due to nerve stimulation or the direct triggering of striated muscles can cause muscle rupture, ligamentous tears, fractures, and joint dislocations (15). In addition, electric current damages tissue from direct thermal heating; the coagulation necrosis is similar to a burn and is managed in the same manner (16).
One long term sequelae of gun shot wounds to the peripheral nervous system known as causalgia (complex regional pain syndrome I) was first described during the Civil War by Silas Weir Mitchell. The patients present with burning pain, paresthesias, skin atrophy, and temperature changes typical of the syndrome. This condition is also seen in electrical injury patients who survive the electrical contact. Axonal injury is usually from the direct thermal injury. Myelin injury is from direct thermal contact as well as from the electrical destruction of the myofibrils in the muscle. Post-neurological symptoms to the peripheral nervous system can vary from neuropathy to reflex sympathetic dystrophy (complex regional pain syndrome II) (17).
Paresthesias are thought to be due from perineurial fibrosis resulting in symptoms of a compressive peripheral neuropathy (18); surgical decompression can sometimes ameliorate the symptoms. Sympathectomy has been used to provide relief in those patients that respond to sympathetic blocks (19). In general nerve injuries associated with gun shot and electrical injuries are treated as closed nerve injuries.
Nerve Injury Associated with Soft Tissue Avulsion Injury
Not to be confused with an avulsion of the nerve itself, a soft tissue avulsion or degloving injury presents a unique problem of coverage. Nerves that are exposed will need coverage to prevent desiccation. The type of soft tissue coverage will depend on the location of the injury and is addressed elsewhere in this book. The coverage can be as simple as replacing missing skin with a skin graft to something more extensive that requires fascia or muscle with skin graft, and ultimately a musculocutaneous or fasciocutaneous flap. If the soft tissue is missing directly over the nerve repair, a flap is needed to cover the nerve repair; this can be either local or a free tissue transfer. The use of vacuum assisted closure dressings has changed our management of complex open fractures and may be used to cover a wound with exposed nerves as well. If the nerves are exposed but uninjured, a protective dressing that keeps the nerves from desiccation may be used, such as a layer of AlloDermw with or without a wound vacuum assisted closure dressing, or one of the various hydrogels on the market that provides enzymatic debridement at the same time as it absorbs excess fluid from the wound. If the nerves are injured and need to be repaired, primarily or with a nerve graft, the definitive repair should be staged so that it is done at the time of the soft tissue.
Nerve Injury Associated with Bony Injury
Nerve injuries resulting from isolated closed fractures are most often due to compression from surrounding tissue edema or are due to, though less frequently, nerve laceration from the fracture ends. Iatrogenic nerve injury may also occur in the course of fracture fixation (20,21).
The anatomic positions of the radial, median, and ulnar nerves and their major branches make them vulnerable at several sites as they course the upper extremity, which explains the typical relationship seen between particular nerve injuries and fracture patterns (22). The more common nerve injuries with associated fracture patterns are listed in Table 5-3 and include the distal humeral shaft fractures and radial nerve palsy (23




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree