A Diagnosis Evaluation requires integration of clinical, imaging, and laboratory findings.
Establishing Rapport
The goal is to reduce the fear in the child and establish confidence with the parents and family [B].
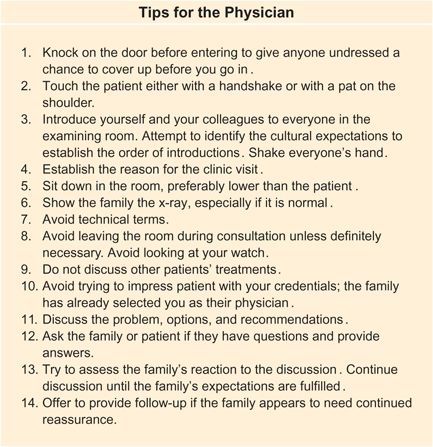
B Suggestions for establishing rapport
Dress
Studies have shown that casual dress promotes approachability and more formal dress enhances confidence. Dress in a way that suggests you have good judgment and are appropriate for the situation. More formal dress may be more appropriate in a major referral center than elsewhere. Avoid making a statement by dress. This usually translates into selecting conservative clothing that promotes an image of good taste.
Initial Introduction
On entering the examination room, acknowledge everyone in the room. Consider the cultural background of the family and conform to gender order for introductions. Shake hands with everyone, including the child. Determine the relationship of each person with the patient.
Be professional, yet friendly. Establishing a good rapport with everyone in the family may be critical to properly managing the child. Later, when difficult management decisions must be made, having rapport with every member of the family is necessary to avoid pressure on the parents to seek additional opinions. Once started, serial consultations usually end with some unnecessary treatment of the child.
Calming the Child
Reducing the child’s fear is the next objective. Consider examining the infant or younger child on the parent’s lap [A]. Ask the child on whose lap he or she wishes to sit. Children will often select the family member who they believe will offer the greatest safety.

A Efficient, comfortable examination Positioned on the parent’s lap, the infant or child is most secure and quiet.
Be friendly with the child. Suggest that this will be a game. Make some positive statements about the child, such as “Mary, you are such a nice child.” Ask some child-oriented questions, such as “What is your pet’s name?”
Start gently examining the child while taking the history from the family. This first step is to convince the child that the examination will not be painful. This is the time for the screening examination, starting with the area most removed from the problem. Being gentle often results in the child becoming less threatened and more cooperative.
Sometimes, these measures fail and the infant or young child remains aggravated and uncooperative. This is the time to move to strategy two—a firm approach [B].

B When coaxing fails Perform the examination without the cooperation of the child.
Present Problem
The concerns usually fall into the categories of deformity, altered function, or pain. Assessment of these complaints should take the patient’s age into consideration. For example, the toddler usually manifests discitis (an intervertebral disc space infection) by altered function in the form of an unwillingness to walk. The child with discitis may primarily show a systemic illness, whereas the adolescent often complains of back pain.
A common pitfall in diagnosis is inappropriately attributing the child’s problem to trauma. Although trauma is a common event in the life of a child, serious problems such as malignant tumors or infections may be mistakenly attributed to an injury [C].
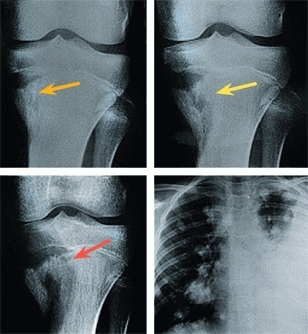
C Attributing problem to trauma A 12-year-old boy gave a history of knee trauma and pain. The initial radiograph was considered normal, but a lesion was present (orange arrow). One month later, the lesion had enlarged (yellow arrow). A diagnosis of Osgood–Schlatter disease was made. A radiograph 2 months later showed further expansion of the lesion (red arrow). A radiograph of the chest just prior to death showed multiple pulmonary metastases.
In addition, graciously deal with questions and concerned by the “worried well” in an attempt to dispel unnecessary concern.
Worried Well
Is a common problem. Deal with this problem by taking their concerns seriously, seeing the source of the concern, performing a screening examination, providing reassurance and written material if available. Suggest any appropriate links to YouTube videos such as What Parents Should Know about common problems.
Deformity
Positional deformities such as rotational problems, flatfeet, and bowlegs are common concerns but seldom significant [D and E]. More significant problems, such as congenital or neuromuscular deformities, require careful evaluation. Inquire about the onset, progression, and previous management. Are there old photographs or radiographs that document the course of the deformity? Is there associated pain or disability? Does the deformity cause a cosmetic problem and embarrass the child? Is it noticeable to others? Finally, be cautious about relying solely on the family’s estimation of the time of the deformity’s onset. Often a deformity originates long before it is first noticed.

D Developmental variation This child with femoral antetorsion shows the classic sitting posture.

E Familial flatfeet Since the father has flatfeet, it is more likely that the child’s flatfeet will persist into adult life.
Altered function
Function can be altered by deformity, weakness, or pain. Pain is a common cause of altered function in the infant and child; the most common example is a limp. A toddler’s fracture of the tibia may manifest itself by a limp or an unwillingness to walk. The young child with toxic synovitis may simply limp; the older child might complain of pain. The newborn whose clavicle is fractured during delivery shows a loss of arm movement on the affected side. This may be confused with a birth palsy. Altered function due to trauma, inflammation, or infection without neurologic damage is referred to as pseudoparalysis.
Pain
The expression of pain is age related. The infant may simply avoid moving the painful part, may fuss and cry, or cry continuously if the pain is severe. The child may show altered function, avoid moving the affected part, or complain of discomfort [A]. The adolescent usually complains of pain.
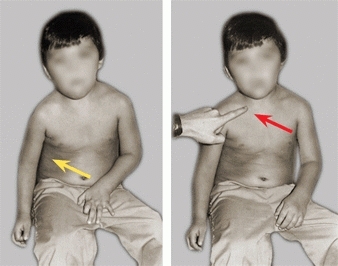
A Pseudoparalysis Use of the arm (yellow arrow) is restricted because of pain. A painful lesion of the right clavicle (red arrow) was due to a leukemic infiltrate.
If the pain responds to rest, it is most likely less serious and an important feature to explore while taking the history and may help with making the diagnosis.
The perception and expression of pain differs widely among individuals, particularly as adolescents grow more adult-like in their responses. A young athlete might minimize his discomfort to improve his chances of participating in the next sporting event. Others might exaggerate the problem. Some adolescents minimize pain by pain-relieving positioning. A herniated disc or an osteoid osteoma may cause scoliosis. This scoliosis results from positioning the spine in a pain-relieving posture. This secondary deformity rather than the underlying condition may be the focus of the evaluation. Unless the underlying condition is identified by the physician, a serious diagnostic error can occur.
History
The past history is essential, not only for understanding the background and general health of the child but also for gaining insight into the current problem. Important aspects of past history include the following:
Birth history
Was the pregnancy and delivery normal?
Development
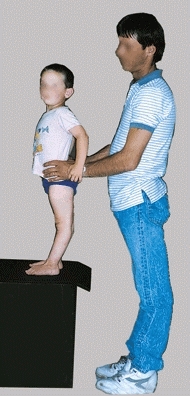
Have the developmental milestones been met at the appropriate ages? When did the infant first sit and walk? About one-third of late walkers are pathologic. In children with conditions such as cerebral palsy, walking is always delayed, and this may be important in establishing whether the condition is progressive [B].
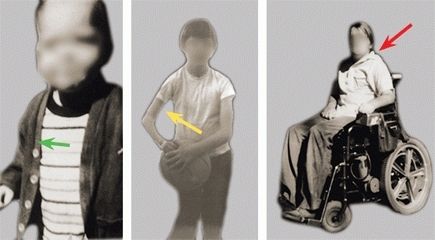
B Importance of medical history This boy had normal function of his right arm (green arrow) as an infant. During early childhood, he developed weakness of the arm (yellow arrow), and a diagnosis of cerebral palsy was made. The weakness increased, and finally during adolescence, he was found to have a tumor involving the cervical spinal cord (red arrow). He became quadriplegic. The progressive nature of the condition is inconsistent with a diagnosis of cerebral palsy. A medical history of progression would have prompted an earlier diagnosis and may have prevented this disastrous outcome.
Mother’s intuition
The mother’s intuition is surprisingly accurate [C]. For example, the mother’s sense that something is wrong with her infant is one of the most consistent findings in infants with cerebral palsy. Take the mother’s concerns seriously.


C Mother’s intuition The mother with painful degenerative arthritis from developmental hip dysplasia (red arrow) sensed something was abnormal about her infant’s hip. Her concern, based on intuition, was discounted by the primary physician, and the asymmetry present on examination was attributed to the child’s mild hemiparesis. This resulted in a delay in diagnosis of developmental hip dysplasia until 18 months of age (yellow arrow).
Family history
Do others have problems similar to those of the patient? If so, what disability is present? A surprisingly large number of orthopedic problems run in families, and knowledge of the disability, or absence of disability, provides information regarding the patient’s prognosis.
Physical Examination
Examination of the musculoskeletal system should include two steps: (1) a screening examination and (2) a complete musculoskeletal evaluation performed to assess a specific complaint. The history and physical examination provide the diagnosis in most cases. It should be thorough and carefully performed. With the proper approach, it is usually possible to perform an adequate examination even without the cooperation of the infant or child.
Approach
Approach the child in a friendly and gentle fashion. Examining the child on the mother’s lap is helpful. If the child is still nervous, keep your distance while obtaining the history. Reassure the child that all you plan to do is to watch her walk or move her legs. If the child is still nervous, examine the parent or sibling first. The child may find it reassuring for you to go through the examination with the parent first. If the child will not cooperate in walking, carry her to the opposite side of the room. The child will usually walk or run back to the parents. If the child has pain, always examine the painful site last.
Screening Evaluation
Examine the adolescent in a gown [A] or, even better, in a swimsuit. It is essential to see the whole child to avoid missing important clues in diagnosis such as a skin dimple that may accompany an underlying spinal deformity [B].

A Examination Examine the adolescent in a gown.

B Sacral dimple A midline skin lesion such as a sacral dimple suggests the presence of a congenital spinal dysraphism.
Perform the screening examination [C] first before focusing on the principal complaint. This screening ensures that you do not miss any other orthopedic problems and will provide a general overview of the musculoskeletal system necessary to understand the specific problem. For example, knowledge of the degree of generalized joint laxity is valuable in assessing a flatfoot or a dysplastic hip. The examination of the back is an essential part of an evaluation of foot deformities. A cavus foot deformity is a common feature of diastematomyelia.
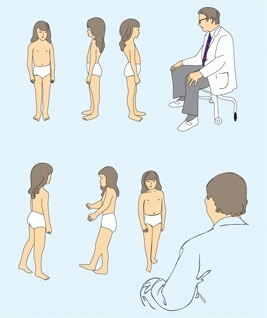
C Screening Inspect from front, side, and back. Observe the child walking normally, then on heels and toes.
Infant screening
Examine the infant on the mother’s lap. First, observe the general body configuration. Next, observe the infant’s spontaneous movement patterns for evidence of paralysis or pseudoparalysis [D]. Any reduction of spontaneous movements is an important finding. For example, the only consistent physical finding of the neonate with septic arthritis of the hip is a reduction in spontaneous movement of the affected limb. Finally, systematically examine the limbs and back for joint motion and deformity. Always perform a screening hip examination to rule out developmental hip dysplasia.

D Importance of observation This infant shows reduced spontaneous movement of the left leg and an abducted position of the left hip. The infant has septic arthritis of the left hip.
Examining the child and adolescent
The examination requires several steps:
General inspection
Does the child look sick [E]? With the child standing in the anatomic position, observe her from the front, side, and back. Look at body configuration, symmetry, and proportions and for specific deformities.

E Ill child.
Pelvis and back
Place your hands on the iliac crests—are they level? A pelvic tilt usually results from a limb length difference. Next, ask the child to raise one leg at a time. A drop in the pelvis on the opposite side indicates a weakness of the hip abductors found in conditions such as hip dysplasia and cerebral palsy. With the child facing you, assess thoracic and lumbar symmetry for evidence of scoliosis by the forward-bending test. Observe the sagittal alignment of the spine [A].


A Sagittal alignment Note the increased lordosis (red arrow) and dorsal kyphosis (blue arrow).
Assessing gait
Ask the child to walk slowly across the room and back first with normal gait and then repeated on her toes and heels. Observe the gait for evidence of asymmetry, irregularity, or weakness. Any abnormal or questionable findings discovered during the screening examination should prompt a more complete evaluation of the problem. For example, a finding of in-toeing should prompt an assessment of the rotational profile.
Specific Evaluations
The history and findings of the screening examination serve as guides to more in-depth evaluation.
Joint laxity
Joint mobility is greatest in infancy and gradually declines throughout life. Joint laxity, like other traits, varies widely among individuals and is usually genetically determined [B]. Extremes in joint laxity are seen in certain disorders, such as Ehlers–Danlos and Marfan syndromes.
B Familial joint laxity Note hyperextension of the knee in both the child and father.
Assess joint laxity by testing the mobility of the ankles, knees, elbows, thumbs, and fingers [C]. Excessive laxity in four or all of the five joints tested occurs in about 7% of children. Joint laxity is a contributing factor in the pathogenesis of hip dysplasia, dislocating patellae, and flatfeet, and it increases the risk of injuries such as sprains. In general, excessive joint laxity suggests the possibility of other problems.
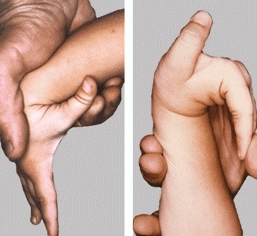
C Finger tests for joint laxity The ability to approximate the thumb and the forearm and extend the fingers to a parallel relationship with the forearm suggests an excessive degree of joint laxity.
Range of motion (ROM)
The normal values of joint motion change with age. Generally, the arc of motion is greatest in infancy and declines with age. Specific joints are affected by intrauterine position. For example, lateral hip rotation is greatest in early infancy and declines during the first 2 or 3 years of growth. In assessing ROM, a knowledge of normal values is helpful. Make certain that the position of the pelvis is determined by palpation when assessing hip abduction [D].

D Assessing hip abduction Stabilize the pelvis with one hand (arrow) and abduct the hip with the other. Assess abduction using the anterior iliac spines as points of reference.
Contractures
of diarthrodial muscles are common in children and sometimes require lengthening. For example, contracture of the gastrocnemius and gracilis occur in cerebral palsy. By proper positioning of the joints above and below the contracture, it is possible to differentiate contractures of these muscles from adjacent elements of the same muscle group.
Hip flexion motion
is difficult to measure due to compensatory motion of the lumbar spine. Measure the range of motion by the Thomas or prone extension tests. The prone extension test has been found to be more reliable. ROM measurements of most joints are reproducible within about ±4°.
Deformity
Deformity is classified as either functional or structural. Functional deformity is secondary to muscle contracture or spasm-producing fixation of a joint in an abnormal position. For example, a fixed hip adductor contracture elevates the pelvis on the affected side, producing a functional shortening of the limb. This deformity is commonly seen in cerebral palsy and Perthes disease. In contrast, structural deformity originates within the limb. An example is the limb shortening associated with fibular hemimelia.
Assess deformity in reference to body planes with the body in the anatomic position [B]. Frontal or coronal plane deformity is most easily observed and creates the most significant cosmetic disability. Sagittal plane deformity produces problems in the plane of motion. Finally, transverse or horizontal plane deformity is most difficult to visualize and had often been overlooked in the past. Currently, CT and MRI studies allow visualization and documentation of this plane and increase the appreciation of transverse plane problems. In assessing and documenting deformity, it is essential that each plane be separated clearly and described independently [A]. For example, in tibia vara, deformity occurs in both the frontal and transverse planes. Failure to clearly separate these planes may result in serious errors if operative correction is undertaken.


A Differentiate transverse and frontal plane deformity This child compensates a severe genu valgum deformity by walking with the feet laterally rotated (red arrows). When the legs are placed in the anatomic position, the valgus deformity of the knees becomes apparent.

B Cubitus varus deformity This deformity is secondary to a malunited fracture. The child is unaware of any problem.
Altered Function
Function may be impaired by many mechanisms. The impairment is most obvious when the onset is acute and recent. The parents are aware when the pseudoparalysis is due to their child’s “pulled” or “nursemaid’s” elbow [C]. Conversely, long-standing changes in function may be overlooked or just considered as an unusual characteristic of the child. A child’s bilateral abductor lurch from dislocated hips may go unappreciated for years. Limping of recent origin is usually obvious to the parents. Sometimes the examination is normal, and imaging studies are necessary to establish the diagnosis [D].

C Pseudoparalysis This child has loss of spontaneous movement of the left arm from a “pulled elbow.”
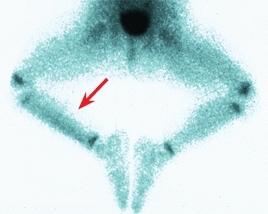
D Limp This child had an obscure limp. The bone scan demonstrated increased uptake over the tibia consistent with a toddler’s fracture (arrow).
Evaluate altered function of recent onset for evidence of trauma or infection. Look for deformity, swelling, or discoloration. Palpate to determine if tenderness is present. Finally, evaluate joint motion for stiffness or guarding. For example, inflammatory and traumatic hip disorders cause a loss of medial hip rotation and guarding of the joint. Evaluate chronic problems for evidence of deformity and an underlying disease. The chronic problem is much more likely to be serious and require a complete and thorough evaluation.
Functional disability is more significant than deformity. Deformity is static; function is dynamic. Deformity is most significant when it adversely affects function. This concept is becoming more universally accepted with time. In the past, handicapped children with conditions such as cerebral palsy were subjected to endless treatments to correct deformity. Often, deformity was corrected at the expense of function. The net effect was harmful.
Some alteration in function is subtle and not readily apparent. For example, a malunited bone forearm fracture may cause a permanent reduction of forearm rotation in the older child. The child compensates for the deformity by rotating the shoulder and may not be aware of any problem. This loss of motion can be detected by physical examination. Determine the degree of disability by functional tests that focus on activities requiring pronation and supination.
Pain
Pain in the child is usually significant. For example, the majority of adults experience back pain, but rarely does it require active treatment. In contrast, back pain in children is much more likely to be organic. Pain in the adolescent is more likely to have a functional basis, as is so common in adults. The most common cause of pain in children is trauma. Trauma may result from acute injury or from the so-called microtrauma or overuse syndromes. Overuse syndromes account for the majority of sports medicine problems in children and adolescents.
Point of Maximum Tenderness
The most useful test in establishing the cause of pain is determining its anatomic origin by locating the point of maximum tenderness (PMT) [A]. Localization of the PMT, together with the history, often establishes the diagnosis. For example, a PMT over the tibial tubercle in a 13-year-old boy very likely means the boy has Osgood–Schlatter disease [B]. A PMT over the anterior aspect of the distal fibula [C, upper], together with a history of an ankle injury, probably points to an ankle sprain. A PMT over the tarsal navicular in a 12-year-old girl suggests the diagnosis of an accessory ossicle [C, lower].


A PMT about the hip The anterior iliac spine (red arrow) and the greater trochanter (yellow arrow) are useful landmarks for determining the PMT about the hip.


B PMT about the knee The PMT is easily determined about the knee. The tibial tubercle (red arrow) is tender in Osgood–Schlatter disease. Medial joint line tenderness (yellow arrow) is found with meniscal injuries.


C PMT about the foot Because bone and joints of the foot are subcutaneous, the PMT is very accurate and an especially valuable sign. The PMT over the lateral malleolus (red arrow) and over the navicular (yellow arrow) are readily localized.
The examination to establish the PMT should start distant from the problem. Palpate gently, moving progressively closer to the site of discomfort. Watch the child’s face for signs of discomfort. Often a change in facial expression is more reliable than a verbal response. Be gentle. Ask the child to tell you where the tenderness is greatest. With gentleness, patience, and sensitivity, the PMT can usually be established accurately with minimal discomfort.
The PMT is a useful guide in ordering radiographs. A PMT over the tibial tubercle suggests the diagnosis of Osgood–Schlatter disease. If confirmation is necessary, order a lateral radiograph of the knee. Similarly, order oblique radiographs of the elbow if the PMT is over the lateral condyle and the AP and lateral views of the elbow are normal. Fracture of the lateral condyle may be demonstrated only on the oblique radiograph.
The PMT is helpful in evaluating the radiographs. For example, locating the PMT aids in differentiating an accessory ossification center from a fracture. Only a fracture will be tender. To determine if a subtle cortical irregularity in the contour of the distal radius represents a buckle fracture, locate the PMT. If the cortical irregularity represents a fracture, the PMT and the questionable radiographic change will coincide exactly in location.
Spondyloarthropathy
Seronegative spondyloarthropathies in the incipient stage are associated with a PMT in specific locations. These are referred to as enthesopathies. Common sites include the metatarsal heads, plantar fascia, achilles tendon insertion, greater trochanter, and sacroiliac joints.
Leg Aches
Leg aches, or growing pains, are discomforts of unknown cause that occur in 15–30% of otherwise normal children. Headaches, stomachaches, and leg aches, in that order, are the common pains of childhood. Leg aches characteristically occur at night, are poorly localized, have a long duration, and produce no limp or apparent disability. Spontaneous resolution occurs, without sequelae, over a period of several years.
Because the pain of leg aches is so diffuse and nondescript, the differential diagnosis includes most painful disorders of childhood. The conditions a physician must rule out include neoplastic disorders such as leukemia, hematologic problems such as sickle cell anemia, infections such as subacute osteomyelitis, and various inflammatory conditions. The diagnosis of growing pains is one of exclusion, relying primarily on the medical history and the physical examination. Rarely are a CBC and ESR or radiographs necessary. Evaluation and management of growing pains is discussed in greater detail in Chapter 8.
Muscle Testing
Muscle testing is done to determine the strength of muscle groups [D]. Testing is performed for neuromuscular problems such as poliomyelitis and muscular dystrophy. The grades can be further subdivided by a plus or minus designation.
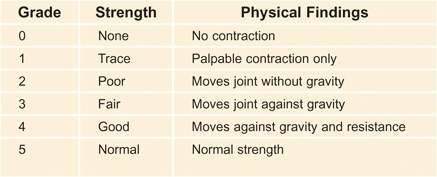
D Muscle grading Manual muscle testing is useful in documenting and classifying muscle strength into six categories.
Clinical Tests
Various tests are useful to supplement the general physical examination in children. Some of the more commonly used tests are described below, presented in alphabetical order.
Abdominal Reflex
Stimulate each quadrant of the abdomen [A]. Normally the umbilicus moves toward the side being stimulated. This test is commonly used to assess a neurologic basis for spinal deformity.
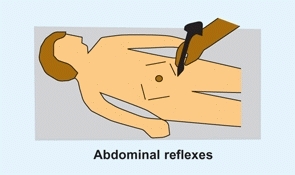
A Abdominal reflexes The abdomen is stroked in all four quadrants. This stimulation causes the umbilicus to move toward the quadrant stimulated. The absence of this response is abnormal.
Anvil Test
This tests for the localization of discitis. Percussion on top of the head causes pain at the site of discitis.
Barlow Maneuver
This maneuver is a provocative test for hip instability in developmental hip dysplasia. See Chapter 11.
Coleman Block Test
This tests for hindfoot flexibility. Ask the child to stand on a block positioned under the lateral side of the foot. With weight bearing, the failure of the heel to assume a valgus position is indicative of a fixed deformity.
Tibial Length
This test assesses the tibia–hindfoot length [B, left]. With the patient supine, flex the knees fully. The difference between the knee heights indicates the amount of shortening. This test can also be performed with the child prone. This allows the knees to be flexed to a full 90°.
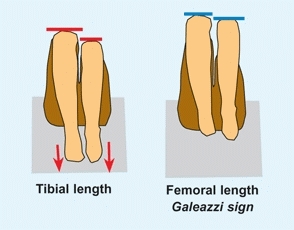
B Assessing femoral and tibial lengths Note the difference in tibial and femoral lengths as observed at the flexed knee. With the feet on the table, tibial length differences are apparent (red arrows). With the hips flexed and the feet free, note the differences in femoral lengths (blue lines).
Ely Test
This test assesses for rectus contracture [C]. Place the child prone and flex the knee. If the rectus is spastic or contacted, the pelvis will rise.
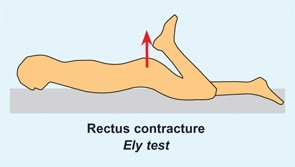
C Rectus femoris contracture evaluation With this contracture, flexion of the knee causes elevation of the pelvis (red arrow).
Foot-Progression Angle
This test assesses the degree of in-toeing or out-toeing (see Chapter 8).
Forward Bend Test
This assesses the functional and structural stiffness and deformity of the back. While observing the patient from the back and again from the side, ask the patient to bend forward as far as possible. Note asymmetry and stiffness. The normal child should show symmetrical flexion and be able to extend the fingers to at least the knee. The spine should show an even flexion of the thoracic spine and reversal of the lumbar lordosis. The thorax should be symmetrical as viewed from the back and front. Spinal cord tumors, inflammatory lesions, spinal deformity, and hamstring contractures all cause abnormal findings.
Galeazzi Sign
This tests for shortening due to developmental hip dysplasia [B, right]. Flex both hips and knees to a right angle. Note any difference in apparent length of thighs.
Goldthwaite Test
This test detects lumbar spine inflammation, as occurs with discitis. Position prone with hips extended and knees flexed. Moving the pelvis from side to side causes a synchondrous movement of the lumbar spine.
Gower Test
This tests for general muscle weakness [D]. Ask the patient to sit on the floor and then stand up without external supports. With trunk weakness, the child uses his hands to climb up his thighs for support.
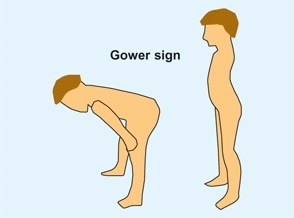
D Gower sign The Gower sign tests for generalized muscle weakness.
Hip Rotation Test
This test screens for inflammatory or traumatic hip problems [E]. Place child in prone position, knees flexed to 90°, and medially rotate both hips. A loss of medial rotation is a positive sign.
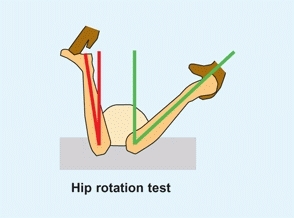
E Hip rotation test This screens for traumatic or inflammatory hip problems. A reduction of medial rotation (red angle compared with normal green angle) is significant, as hip rotation is usually symmetrical in children.
Nélaton’s Line
This test is useful in clinical assessment of hip dislocation. The tip of the trochanter should fall below a line connecting the anterior iliac spine and the ischial tuberosity.
Ober Test
This tests for tensor fascia contracture [A]. Position the patient on one side with the lower knee and hip flexed to a right angle. Abduct and fully extend the upper hip. While maintaining the hip extended, allow the leg to fall into full adduction. An abduction contracture is present if the thigh fails to fall into adduction. The degree of contracture equals the abducted position above the neutral or horizontal position.
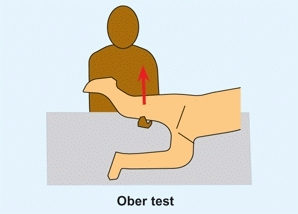
A Ober test This tests for tensor fascia contracture. Abduct and extend the leg, then allow it to fall. A failure of adduction is positive for a tensor contracture.
Ortolani Maneuver
This maneuver tests for hip instability in developmental dysplasia of the hip (DDH). See Chapter 11.
Patellar Apprehension Sign
This test is for patellar instability. With the knee extended, gradually apply pressure to laterally displace the patella while observing the patient’s facial expression. Apprehension indicates previous experience with patellar dislocation.
Patrick or Faber Test
This test detects sacroiliac (SI) inflammation [B]. Place the ipsilateral foot over the opposite knee. While holding down the opposite ilium, apply a downward force on the flexed knee. Pain at the SI joint is a positive finding.
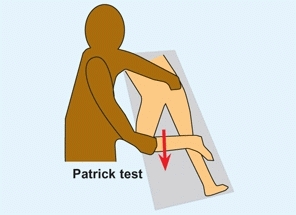
B Patrick test This test is performed by positioning the leg across the other and applying downward pressure. This elicits pain in the ipsilateral sacroiliac joint region.
Pelvic Obliquity Test
This differentiates suprapelvic from infrapelvic obliquity. Position the child prone with the pelvis on the edge of the examining table, allowing the lower limbs to flex. Windswept positioning of the legs brings the pelvis to neutral if the obliquity is infrapelvic in origin.
Phelps Gracilis Test
This test is a measure of gracilis spasticity or contracture. Position the patient prone and abduct the hip with the knee flexed. Passive knee extension causes hip adduction if the gracilis is contracted.
Popliteal Angle Measure
This measures hamstring contracture [C]. With the patient supine, flex the hip to a right angle and the knee to a comfortable maximum. The contracture equals the degree of lack of full knee extension.
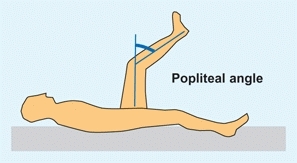
C Popliteal angle With the hip flexed, extend the knee. The degrees short of full extension equal the popliteal angle (blue arc).
Prone Extension Test
This tests for hip flexion contracture [D]. Position the patient prone with the thigh over the edge of the examining table. With one hand on the pelvis and other holding onto the leg, extend the leg until the pelvis starts to elevate. The horizontal–thigh angle demonstrates the degree of contracture.
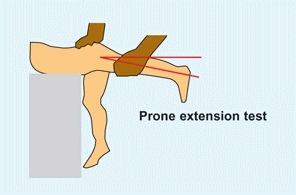
D Prone extension This test assesses hip flexion contracture. With the contralateral hip flexed, extend the ipsilateral side to the degree that causes the pelvis to elevate. The degrees short of full extension equal the degrees of contracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








