1
English version
1.1
Introduction
Though a rare occurrence, epidural lipomatosis (EL) is a possible cause of back pain. It is characterized by an accumulation of normal, unencapsulated fat in the dorsal epidural or lumbosacral space. It has been a known quantity since the description by Lee in 1975 of a patient treated with corticosteroids after kidney transplant. Since then, largely on account of the development of MRI, at least 134 cases have been published .
1.2
Clinical case
A 42-year-old patient was referred for consultation to a rehabilitation center for back pain that had been developing for 1 year. Aggravated by a standing position lasting more than 15 minutes and while walking, the pains necessitated cessation of activity. At a later stage, they were associated with lower back pain involving irradiation of the posterior right leg. He had fallen repeatedly, usually frontward, but the frequency of the falls, which were apparently related to subsidence of the muscles during ambulation, remained imprecise. No vesico-sphincter dysfunction had occurred.
He had a past history of hypertriglyceridemia, panic attacks that were being treated by psychotropic drugs, and broken tibia and fibula as well as femoral fracture after a road accident. He was not treated by corticosteroids, and was not diabetic.
His body mass index was 35.4 kg/m 2 , and he had a trunk flexion posture. Examination revealed right lumbar paravertebral contraction. Finger Floor Distance was 0 cm. The Lasegue straight leg maneuver was positive from 60° bilaterally. Neurological examination revealed no motor dysfunction of the lower limbs. Bone tendon reflexes were more pronounced in the left lower limb but they were not diffused, and there was no epileptoid trepidation or cutaneous plantar reflex abnormality. Sensitivity on examination of the “long” cerebrospinal tracts and the dermatomes from L4 to S1 was shown to be symmetrical.
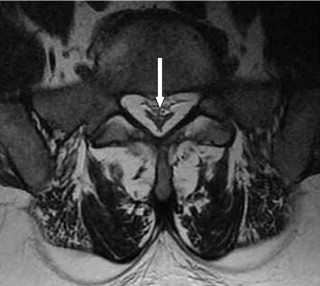
Spine MRI weighted T1 showed an abnormal accumulation (10 mm) of fat in the posterior dorsal epidural space compressing the spinal cord ( Fig. 1 ) and a circumferential accumulation in the lumbar canal with a Y-like deformation of the dural sheath in L5-S1 ( Fig. 2 ). Disc diseases L4-L5 and L5-S1 were present but remained unrelated to any nervous structure.

Morning plasma cortisol was 511.6 nmol/l (reference values: 102.1 to 535.2 nmol/l) and ultrasensitive TSH was 3.18 mU/l (reference values: 0.40 to 3.50).
A diagnosis of EL with obesity was given. At this clinical stage, conservative treatment associating weight reduction by means of hypocaloric and with management in a center of rehabilitation was recommended. Due to his state of anxiety the patient refused planned hospitalization, but he did go ahead with a diet, and the information received from his general practitioner after 10 months of evolution was reassuring; the patient had lost 17 kg, and his BMI had decreased to 30 kg/m 2 . Moreover, there was no more rachialgia or radiculalgia, nor were there additional falls.
1.3
Discussion
EL is a known but rare complication of the exogenous and occasionally the endogenous Cushing’s syndrome through which fats are redistributed in the axial area. Setting aside one case of EL associated with hypothyroidism and another case related to pituitary prolactinoma , the other previously described patients, whose condition was considered as idiopathic, were frequently obese . Obesity is currently clearly identified as one of the causes of EL, and it represents around 25% of the reported cases . Many of these patients are middle-aged men comparable to ours. Observation suggests a relationship between EL and central obesity . While accumulation of fat has been described in the dorsal and/or lumbosacral areas, it has not yet been observed in the cervical region . In fact, the clinical presentation of EL depends on the location of the fatty deposits and may consist in: dorsalgia, lumbalgia, radiculalgia, paraparesis, neurogenic claudication or, more rarely, vesico-sphincter disorders . The symptoms are at times attributed to the illness having necessitated corticotherapy, to the side effects of corticosteroids, and to excess weight , and this probably explains a certain underestimation of the number of cases in clinical practice. Some patients have these symptoms treated by a rheumatology, a neurology or a physical medicine unit before having recourse to surgery.
With MRI, a radiological diagnosis is relatively easy to achieve when there exists an abnormally abundant fatty deposit in hypersignal T1:
- •
more than 6 mm thick in the posterior epidural space of the dorsal area with compression of the spinal cord on the sagittal sections;
- •
centripetal in the lumbar area with a characteristic “Y” image of the dural sheath on the axial slices.
These radiological criteria were present in our patient. A radiological differential diagnosis must include extradural angiolipoma in a possibly dorsal location and with identical density, but the angiolipoma is usually clearly situated .
When clinical presentation permits, particularly when there is no neurological deficit, conservative treatment is to be preferred to surgical treatment. According to the etiology, it will consist in: corticotherapy reduction and associated dietetic measures , treatment of the cause of the endogenous hypercorticism treatment or weight reduction . When the responsibility of a hyperinsulinemia metabolic syndrome in obese patients suffering from EL is suggested , it appears logical to implement a low-carbohydrate diet so as to mobilize lipids and thereby reduce epidural fat volume. However, given the small number of previous observations, it is not possible to deliver precise recommendations on the best way of carrying out and accompanying weight reduction. In emergency situations such as rapidly progressive neurologic deficit or following failure of conservative treatment, decompression surgery is to be recommended, and it is usually effective .
After having diagnosed (P. Noël) three other EL cases of which two have been published , the latest case we encountered in daily practice leads us to think that this medical condition should be strongly suggested in clinical pictures associating rachialgia with neurologic signs, particularly in patients undergoing chronic corticotherapy and/or obese. In agreement with other authors , we are persuaded that EL is largely unknown in the medical profession and that it is probably underdiagnosed in daily practice, even though its diagnosis with MRI is relatively easy. Early medical management is likely to limit recourse to decompression surgery.
Disclosure of interests
The authors declare that they have no conflicts of interest concerning this article.
2
Version française
2.1
Introduction
Bien que rare, la lipomatose épidurale (LE) est une cause possible de rachialgie. Cette affection est caractérisée par l’accumulation de graisse normale, non encapsulée, dans l’espace épidural dorsal ou lombo-sacré. Elle est connue depuis la description, par Lee en 1975, d’un patient traité par corticoïdes après transplantation rénale. Depuis, au moins 134 cas ont été publiés surtout à la faveur du développement de l’IRM.
2.2
Cas clinique
Un patient de 42 ans est adressé à la consultation du centre de rééducation pour des dorsalgies évoluant depuis 1 an. Ces douleurs sont aggravées par la station debout dépassant 15 minutes et à la marche nécessitant l’arrêt de l’activité. Elles sont plus récemment associées à des lombalgies avec une irradiation à la face postérieure de la jambe droite. Il fait des chutes, habituellement en avant, dont la fréquence est imprécise. Celles-ci semblent liées à un dérobement des membres inférieurs à la marche. Il n’a pas de troubles vésico-sphinctériens.
Il a des antécédents d’hypertriglycéridémie, d’attaques de panique traitées actuellement par psychotropes, de fractures tibio-péronière et fémorale après accident de la voie publique. Il n’est pas traité par corticoïdes. Il n’est pas diabétique.
Son index de masse corporelle est de 35,4 kg/m 2 . Il a une posture en flexion du tronc. L’examen révèle une contracture para vertébrale lombaire droite. La distance doigt-sol est de 0 cm. La manœuvre de Lasègue est positive à partir de 60 degrés bilatéralement. L’examen neurologique ne révèle pas de déficit moteur aux membres inférieurs. Les réflexes ostéo-tendineux sont plus vifs au membre inférieur gauche mais non diffusés, sans trépidation épileptoïde ni d’anomalie du réflexe cutané plantaire. La sensibilité est symétrique aussi bien dans l’examen des voies longues que celui des dermatomes de L4 à S1.
L’examen IRM du rachis montre, en pondération T1, une accumulation anormale (10 mm) de graisse dans l’espace épidural postérieur dorsal refoulant le cordon médullaire en avant ( Fig. 1 ) et une accumulation circonférentielle dans le canal lombaire avec déformation en « Y » du sac dural en L5-S1 ( Fig. 2 ). Des discopathies L4-L5 et L5-S1 sont présentes mais sans relation avec une structure nerveuse.










