CHAPTER 122 Epidemiology of Back Pain in Pregnancy
INTRODUCTION
Low back pain is an important and commonly occurring public health problem with high impact to the person, family, and society. Prevalence figures of low back pain vary considerably across studies because of various factors, including case definition. In a prospective Danish study 40% of women, 25–34 years of age, reported low back pain during 1 year with a point prevalence of 20%, regardless of the degree of pain intensity or disability.1 When disability of low back pain was taken into consideration, in a Canadian study, 50% of the population had experienced low-intensity/low-disability low back pain (including the sacral area) and 10% had experienced high disability low back pain in the previous 6 months, with a small age variation. Interestingly, women experienced almost twice the rate of high-disability low back pain compared with men.2
EPIDEMIOLOGY
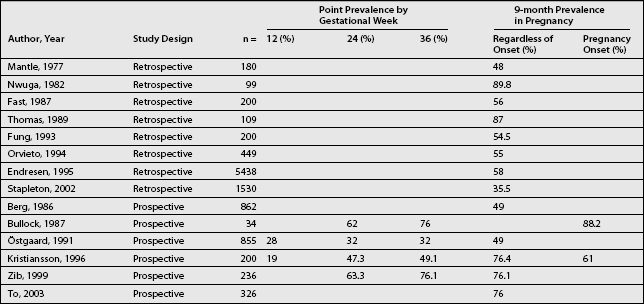
In comparison to the 1-year prevalence of back pain among women from the general population, a reported 9-month prevalence rate of back pain during pregnancy, regardless of its onset, on average about 55% (range, 35.5–89.8%) has been reported.3–16 The 9-month prevalence rate of back pain during pregnancy varies substantially among different studies with a mean prevalence rate within retrospective studies of 54% (range, 36–90%),3,5,6,8,9,11,13,15 and in prospective studies 58% (range, 49–88%) (Table 122.1).4,7,10,12,14,16 A true difference in prevalence of back pain between pregnant and nonpregnant women is strengthened by data from an Australian study where the odds ratio of having low back pain in pregnancy was 3.5 times higher than that of nonpregnant women.12 Thus, it appears that back pain is more common during pregnancy than in the nonpregnant state or in men.
When back pain with onset during current pregnancy was considered, prevalence rates of between 61%7 and 88%14 was observed. The onset of back pain during pregnancy was fairly evenly distributed over the pregnancy period in most studies.5,7,8,13–15 The obvious conclusion derived from this information is that most women develop pregnancy-related back pain long before the commencement of abdominal enlargement or postural alterations. Among women developing back pain during pregnancy about 16% had reported a new location of back pain during the first 12 gestational weeks, 67% at 24th gestational week, and 93% at week 36. Thus, the largest proportion of pregnant women were experiencing new low back pain before their fifth month of pregnancy and a smaller proportion of pregnant women develop low back pain during the major growth period of the fetus.
Among women with back pain with onset during pregnancy, sacral pain is by far the most common location, reported by about 50% of women, followed in order by lumbosacral, lumbar, and thoracic pain. Cervical axial pain rarely manifests during pregnancy.7,10 This is in contrast to pregnant women with back pain with onset prior to pregnancy when the lumbar and thoracic pain were the most common.7 Nearly every second women (45.5% and 46.8%) with pregnancy-related low back pain experiences symptoms that refer to the buttocks and thighs, occasionally down the legs,5,6 but only rarely reaching the feet.5 True sciatica with pain below the knee was found in only 1%.10 Regardless of the symptom location in the lower extremity, a duration of 1–3 months is common. However, 5–10% of women report pain duration in pregnancy of more than 5 months where sacral pain is dominating.4,7
Pain intensity among women with onset of back pain during pregnancy significantly increased over the duration of pregnancy. This is reflected by the duration of pain and not simply an increase during the later stages of pregnancy. This means that the longer the duration of back pain related to pregnancy the higher the reported pain intensity. In addition, there is a significant indirect correlation between pain intensity and age in several studies. Younger women reported higher pain scores than older women.3,7,17
Among women with back pain during pregnancy the intensity of pain varied during the day and between days. One study showed that 16% of the pregnant women suffered from pain hourly, 66% daily, and 18% weekly.5 Among women with daily back pain, one-third reported increased pain toward the end of the day and one-third experienced increased pain during the night.5,8 In the study by Mantle et al., nearly half of the women reported most troublesome backache in the morning.8 An explanation of this variation of back pain intensity could be that the intensity of back pain emerges over time during or after strain applied to the spine from various workloads, and then pain is relieved following rest. The specific load on the back initiates pain in susceptible women, leading to the greatest pain intensity later in the day, at night,5,6,13 or the following morning.8 Back pain may result in an impaired sleep pattern as is demonstrated by decreased periods of rapid eye movement sleep.18 About one-third19 of pregnant women arose at night because of a backache, experiencing even more severe pain than during the day.6
Pregnancy-related back pain has a great impact on women, particularly those suffering from high-intensity pain when compared to pregnant women without pain at all. In prospective studies, about 30–35% of women with back pain describe the pain as a severe problem compromising normal, everyday life.7,10 They preferentially describe difficulty with heavy physical work, heavy lifting, running, or physical exercise. They can also experience trouble with walking, sitting for longer than a few minutes, carrying a bag, or activities that require slight forward flexion while in the standing position (such as making the bed). This indicates that back pain during pregnancy causes restricted physical activity over and above that caused by pregnancy itself.7 The impact of pregnancy-related back pain is also highlighted by the fact that among previously pregnant women, one of five from the general population, as well as among women with scoliosis, refrain from becoming pregnant again due to fear of developing back pain during pregnancy.20,21
Back pain related to pregnancy appears to be a global problem that occurs in developed as well as developing countries. High prevalence rates of back pain during pregnancy have been reported in Europe, America, Australia, China, including the mountainous region of Taiwan and Africa’s rural areas as well as among upper-class women in Nigeria.6,7,11–13,22,23
Back pain during pregnancy has been reported from different ethnic groups.5,6,7,9,13,22 Although the distribution of back pain during pregnancy seems to differ among certain ethnic groups, this could, however, be a reflection of socioeconomic status. In a study from Israel9 on consecutive women referred for an antenatal ultrasonographic examination Sephardic women with origin in Africa and Asia had a much higher prevalence of low back pain during pregnancy as compared to those of other origin such as Ashkenazi, mixed, and Arabic (64.5% as compared with 27.5%, 5.5% and 2.5%, respectively). In an American retrospective interview study5 in a maternity ward the ratio of Caucasians was much higher in the back pain group compared with the nonpain group (34% versus 15%). The opposite was true for Hispanics compared to the nonpain group (13% versus 26%).
For many mothers, back pain related to pregnancy resolves in the first months after delivery, but for some it may continue for several months or years. In a prospective study, where the onset of pain was not accounted for, the prevalence of low back pain following delivery showed a rapid decline from 65% at 1 month postpartum to 37% at 6 months after delivery. Thereafter, the recovery rate was slow,24 up to the end of study 18 months postpartum when 7% still had persisting serious back problems. This is in agreement with a study of women with onset of back pain during pregnancy, in which women were clinically classified during pregnancy and follow-up. Among those women, 8% were still classified as experiencing daily low back pain 2 years after childbirth.25
Characteristics of women with a slow regression of back pain following delivery include longer periods of back pain during pregnancy, high intensity of back pain during pregnancy, older age, and unskilled work during pregnancy.24,25 In addition, women with back pain during previous pregnancies and multipregnant women are more likely to experience persistent back pain following the current pregnancy.24 No association has been identified linking postpartum back pain and mode of delivery or epidural anesthesia.26 Women with continuing back pain after delivery report adverse effects from the pain similar to those during pregnancy. In addition, among women with persisting severe back pain related to pregnancy, 25% changed occupation because of the pain, compared to 3% in the control group.21
Back pain before, and particularly during previous pregnancy, is a strong predictor for the development of back pain in pregnancy.6,9,10,16,21,27 Almost all women with low back pain in an index pregnancy, identified and documented with a neurologic and musculoskeletal examination, developed low back pain during the subsequent pregnancy,21 indicating an extremely high risk for these women. Conflicting results have been reported regarding the possible association between prevalence of back pain in pregnancy and the number of previous pregnancies, the number of previous deliveries, and age. The differences are most likely a consequence of methodological issues. However, the number of pregnancies influenced the duration17 and the number of deliveries the severity of back pain in a subsequent pregnancy.13 In addition, multiparity increased the incidence of back pain after delivery.16 An environmental factor that is associated with pregnancy-related back pain is a heavy workload.10 Among pregnant women in a rural area of Taiwan, 85% of pregnant women who performed very heavy work reported low back pain compared to 49% among pregnant women performing light work.13 Factors that showed no association to back pain in pregnancy were body height and body weight during early pregnancy and weight gain during pregnancy, infant’s birth weight, and postural change.
Thus, it appears that back pain emerges more often among women during pregnancy than in the nonpregnant state or in men. However, the reason for this is still unclear. During pregnancy there are hormonal, biomechanical, circulatory, and psychosocial changes. Any of these factors, or a combination, may be involved in the pathophysiology of axial back pain. Generally, back pain in pregnancy is assumed to be related to a combination of mechanical stressors and hormone-induced changes in the ligamentous support of the spine.
During pregnancy there is a significant change in magnitude of lumbar lordosis and thoracic kyphosis. This change in posture occurs during the fifth and ninth months of pregnancy.14 Yet, no relationship between posture and pregnancy-related back pain has been reported. The absence of any proof of an association between posture and back pain during pregnancy suggests that some factor other than posture must play an important role in pain production.14
Lumbar disc herniation as a cause of back pain in pregnancy is unusual, with an estimated prevalence rate of 1 in 10 000 pregnancies.28 However, a disc bulge or prolapse is common and can occur in as many as every second woman of childbearing age, whether pregnant or not.29 In Chinese pregnant women undergoing magnetic resonance imaging pelvimetry a disc bulge or prolapse was seen infrequently during the last trimester, whereas a significant correlation was shown with current reported low back pain.23 However, as the majority of those women with back pain had no disc bulge this was not the only cause for back pain in pregnancy.23 Interestingly, it was also shown that a higher signal intensity in the uterine cervix correlated with back pain during pregnancy, which may represent indirect evidence for a relationship between pregnancy effects on soft tissue and back pain in pregnancy.23 Furthermore, in general, women experiencing symptoms of a herniated lumbar disc had had more pregnancies resulting in live births than women of similar age without known herniated discs. This observation suggest that a full-term pregnancy may be a cause of radicular pain due to a focal protrusion.30
Women with adolescent idiopathic scoliosis experienced no adverse biomechanical alterations from pregnancy such as progression of the scoliosis curve.20 A progression of scoliosis was not detected in women treated with a posterior spinal fusion or with conservative treatment including wearing an orthosis.20 Furthermore, the rate of complications during pregnancy, including back pain, for women with adolescent idiopathic scoliosis of different degrees was not higher than in the general population.31
The influence of pregnancy on the ligamentous and osseous support of the spine and pelvis, as a cause of pregnancy-related back pain, has been studied in women with congenital defects of collagen synthesis. In a retrospective study of women with osteogenesis imperfecta, a disorder causing fractures and increased fragility of connective tissue, the most common musculoskeletal problem during pregnancy was back pain, while the prevalence of back pain during pregnancy was not higher than among healthy women.32 However, a high proportion of pregnant women reported severe back pain in pregnancy causing a disruption of activities of daily living with no identified cause of the pain in most cases.32 Ehlers-Danlos syndrome is a heterogeneous collection of inherited disorders of the connective tissue. In a retrospective study of previously pregnant women affected by Ehlers-Danlos syndrome as many as 27% were suffering from severe low back pain in the sacral area compared to 7% in a control group of unaffected women.33
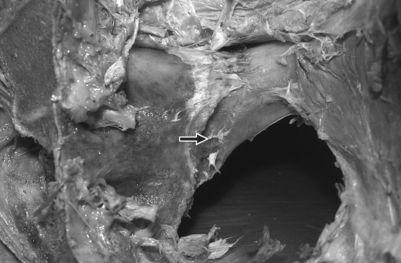
Results from several studies indicate that there is an obvious influence of pregnancy on tissue of ligament and bone in the low back region. In anatomic studies, variably deep grooves at the insertions of ligaments at os ilium and os sacrum have been demonstrated. It was also demonstrated that a groove, adjacent to the inferior end of the sacroiliac joint on os ilium, constitutes the insertion of the anterior sacroiliac ligament (Fig. 122.1).34 In radiologic studies, this bone resorption has been demonstrated among 25% of examined women while not present in men.35,36 Furthermore, the deep grooves were displayed only in women with previous deliveries.35 In addition, there was a relationship between the presence of these grooves and osteitis condensans ilii. This latter entity is believed to be a manifestation of bone remodeling in response to stress across the sacroiliac joints associated with a previous pregnancy.35 However, their correlation with back pain has not been studied. Further evidence of the influence of pregnancy on the spine is a doubling of the incidence of degenerative spondylolisthesis in parous women with low back pain compared to men and nulliparous women with back pain.37 Women who had borne children had the highest incidence of degenerative spondylolisthesis (28%), especially at level L4–5, compared to nulliparous women (17%) and men (7.5%).37
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree