Chapter 27 Epicardial Ventricular Tachycardia
Electrophysiological Substrate
In patients with nonischemic CMP, detailed epicardial electroanatomical substrate mapping has identified large confluent low-voltage areas consistent with myocardial scar. The epicardial scar areas are typically larger than the endocardial left ventricular (LV) scar areas and have a typical distribution similar to that for endocardial LV scars, usually located in basal lateral areas of the LV adjacent to the mitral valve annulus. Epicardial ablation is needed more often in patients with sustained monomorphic VT associated with dilated, nonischemic CMP than in patients with prior MI.1
In patients with ARVD, sizable low-voltage areas often involve the infundibulum, free wall, and basal perivalvular regions, constituting the endocardial substrate. More recently, extensive epicardial low-voltage areas, often with fractionated and late electrographic recordings, have been identified. The epicardial scar is consistently larger than that on the endocardial surface. In patients with ARVD and VT refractory to endocardial ablation, the origin of VT defined on the epicardium is frequently noted beyond the endocardial-defined scar.2 In a recent report, the highest prevalence of epicardial VTs was observed in patients with ARVD (41%) and nonischemic CMP (35%), followed by patients with ischemic heart disease (16%).3
Small series have also reported successful ablation of epicardial VTs following a failed endocardial ablation in patients with idiopathic outflow tract VTs. Often underrecognized, the incidence of an epicardial origin in idiopathic VT may be as high as 14%. Idiopathic outflow tract VTs with epicardial origins can originate close to the anterior interventricular vein, great cardiac vein, and middle cardiac vein; and successful ablation from within these structures has been reported. When this approach fails, percutaneous epicardial mapping and ablation have been reported to be feasible and successful.4
Electrocardiographic Features
Several ECG findings can suggest an epicardial origin of the VT with right bundle branch block (RBBB)–like configuration, all of which generally rely on the late engagement of His-Purkinje fibers by exits on the epicardium, resulting in intramyocardial delay of conduction and a slurred initial part of the QRS complex: (1) pseudo-delta wave (so called because of its similarity to the slurred upstroke delta wave observed during ventricular preexcitation) greater than 34 milliseconds (measured from the earliest ventricular activation to the earliest fast deflection in any precordial lead) has a sensitivity of 83% and a specificity of 95%; (2) long R-wave peak time in lead V2 (i.e., interval from the beginning of the QRS complex to the time of initial downstroke of the R wave after it has peaked [previously known as the intrinsicoid deflection]) greater than 85 milliseconds has a sensitivity of 87% and a specificity of 90%; (3) shortest RS complex duration (measured from the earliest ventricular activation to the nadir of the first S wave in any precordial lead) equal to or greater than 121 milliseconds has a sensitivity of 76% and a specificity of 85%; and (4) QRS duration greater than 200 milliseconds (see Fig. 22-8).4,5
These criteria, however, do not seem to apply uniformly to all LV regions or to VTs originating from the right ventricle (RV). Other site-specific criteria have been suggested for identifying an epicardial origin for LV VTs: (1) the presence of a Q wave in lead I for basal superior and apical superior VTs; (2) the absence of a Q wave in any of the inferior leads for basal superior VTs; and (3) the presence of a Q wave in the inferior leads for basal inferior and apical inferior VTs. Also, measurement of the maximal deflection index (defined as the time from QRS onset to maximal deflection in precordial leads divided by the QRS duration) can help identify epicardial VT originating in the LV outflow region. A delayed shortest precordial maximal deflection index (≥0.55) identifies epicardial VT remote from the aortic sinus of Valsalva with high sensitivity and specificity. This observation is consistent with slower spread of activation from a focus on the epicardial surface relative to the endocardium and delayed global ventricular activation resulting from later engagement of the His-Purkinje network.6,7
Epicardial VTs originating close to the proximal segment of the great cardiac vein typically display RBBB morphology, whereas VTs originating close to the distal segment have left bundle branch block (LBBB) morphology. This may be explained by a location within the basal-lateral myocardium for the former and a more anterobasal location for the latter arrhythmias. If the site of origin is in the proximal segment of the great cardiac vein, the initial vector is directed toward lead V1, accounting for the RBBB morphology. As the site of origin moves toward the distal part of the great cardiac vein, closer to the anteroseptal myocardium, the initial vector is directed away from V1, resulting in LBBB morphology. An R-wave width greater than 75 milliseconds in lead V1 is useful for differentiating epicardial idiopathic VTs from endocardial arrhythmias. The broader R wave is explained by a more posterior position relative to lead V1 compared with the RV outflow tract (RVOT). However, because of a more anterior position relative to lead V1, the epicardial arrhythmias that are located within the distal part of the great cardiac vein have a narrow R wave in lead V1, making them impossible to distinguish from RVOT VT.7,8 Epicardial VTs that appear to follow the anterior interventricular vein often have a characteristic loss of R wave from leads V1 and V2 with broad R waves in leads V3 through V6.
Although various ECG characteristics have been used to predict whether an epicardial approach may be required based on the VT morphology, it is important to understand that the QRS morphology is related solely to the VT exit site and this does not imply that some other component of the circuit (such as the critical isthmus or entrance site) cannot be ablated from the endocardium, even when an epicardial exit is implied by the ECG characteristics. Therefore, it is unlikely that the surface ECG by itself will ever be entirely predictive of the need for epicardial access for mapping and ablation for any given VT.5 Additionally, large areas of conduction delay often present in patients with myocardial scar can produce misleading activation sequences and confound ECG prediction.9
Percutaneous Epicardial Approach
Clinical Considerations
VT originating from the subepicardium is an important cause of failure of endocardial ablation approaches. Mapping arrhythmia foci or circuits that are deep within the myocardium or in the epicardium can be attempted via the coronary sinus (CS) or pericardial space. The CS approach, however, has important limitations. Catheter manipulation is limited by the anatomical distribution of the cardiac veins, and epicardial circuits may be identified only when the vessel cannulated happens to be in the region of the circuit. An alternative epicardial approach involves inserting an introducer sheath percutaneously into the pericardial space in the manner used for pericardiocentesis. The subxiphoid approach to the epicardial space allows extensive and unrestricted mapping of the epicardial surface of both ventricles, and has been used most commonly for VT mapping and ablation (far less so for supraventricular arrhythmias). Nonetheless, mapping of the CS and accessible coronary venous branches can be performed prior to the percutaneous epicardial approach to look for clues of an epicardial origin of the VT circuit, and has been particularly useful in idiopathic outflow tract VTs.4,9
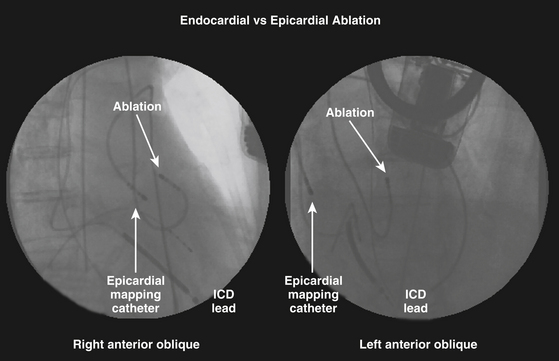
Catheter ablation from the epicardium is often required for elimination of VTs due to nonischemic CMP and is occasionally useful for VTs in a variety of other diseases, as well as some idiopathic VTs. Nonetheless, despite the increasing recognition that ventricular arrhythmias may originate from epicardial foci, epicardial VT ablation remains a specialized procedure and is performed at relatively few centers. In the majority of reported cases, percutaneous epicardial VT ablation has been performed only after failure of a thorough endocardial mapping and ablation session, at a separate setting or during the same setting after exhausting endocardial mapping efforts. Simultaneous endocardial and epicardial mapping can have several advantages (Fig. 27-1), such as a better chance to map and ablate all inducible VTs, reduce the number of procedures required for patients with suspected epicardial VTs, and an opportunity to acquire more expertise with the technique.4 Also, epicardial mapping and ablation may be useful as a first procedure when endocardial mapping is not an option because of intraventricular thrombi or in patients with metallic prostheses in the aortic and mitral valves.4
There are several conditions that can significantly limit the feasibility of percutaneous epicardial mapping and ablation. Previous cardiac surgery usually results in significant pericardial fibrosis, and the pericardial space is often, but not always, virtually replaced by fibrotic adhesions. In this setting, percutaneous cannulation of the pericardial sac is very difficult; even when percutaneous cannulation is successful, manipulation of the instruments is extremely limited and difficult. Additionally, pericardial venous varices have been reported in patients with SVC and azygous venous occlusion. Thus, catheter manipulation and ablation inside the pericardial space of a patient with pericardial varices can result in severe bleeding complications. When pericardial varices are suspected, the diagnosis can be made by three-dimensional (3-D) computed tomography (CT) angiography. Also, the presence of a large hiatal hernia can predispose to inadvertent perforation (and subsequent mediastinal infections) during cannulation attempts. Congenital absence of the pericardium is a rare congenital anomaly (approximately 1 in every 10,000 autopsies) that is most often asymptomatic and can be an incidental finding after the patient is referred for a pericardial procedure. In the preprocedural evaluation, this rare anomaly may be suspected by an abnormal cardiac rotation or silhouette on the chest x-ray film. Definitive diagnosis can be made by CT or magnetic resonance (MR) imaging.10
Preablation Evaluation
Careful analysis of the ECG during VT or premature ventricle complexes (PVCs) is essential. As noted, different ECG criteria for recognizing an epicardial origin of arrhythmia have been proposed. Additionally, MR imaging can help identify epicardial substrate in cardiomyopathies.3 Furthermore, evaluation should include comprehensive clinical assessment and imaging studies to recognize any preexisting contraindications, and to minimize complications. Chest radiograph, echocardiography, and cardiac CT or MR imaging have proven to be useful for screening these patients.
Contrast-Enhanced Magnetic Resonance Imaging
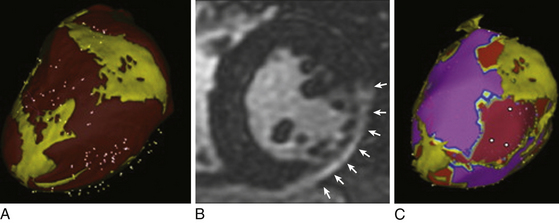
Delayed contrast-enhanced MR imaging delineates regions of scar tissue potentially forming part of the arrhythmia substrate in patients with ischemic and nonischemic CMP, and enables the depiction of transmural and nontransmural scars with high spatial resolution, allowing determination of whether the scar is endocardial, intramyocardial, or epicardial (Fig. 27-2).
The suspicion of an epicardial VT substrate can facilitate planning of VT ablations, such as for a combined endocardial and epicardial approach, especially given the fact that visualization of epicardial or intramyocardial scar on preprocedure delayed enhancement MR imaging was found to be predictive of failure of the endocardial approach and of the need for the epicardial approach for VT ablation.11
Cardiac MR imaging can also help determine the underlying etiology of nonischemic CMP in some patients, such as myocarditis, sarcoidosis, and ARVD, which can be associated with a higher susceptibility for VT. Furthermore, in patients undergoing epicardial mapping and ablation procedures, registration of preacquired MR images with real-time electroanatomical mapping allows visualization of ventricular anatomy and obstacles to procedural success, such as epicardial fat, which can be helpful during the mapping procedure in differentiating the cause of low epicardial voltages (fat versus scar).11
Contrast-Enhanced Computed Tomography
A contrast-enhanced CT scan enables detailed and comprehensive evaluation of LV myocardium using triple, multimodality imaging based on anatomical, dynamic, and perfusion parameters to identify abnormal substrate (myocardial scar and border zone) with high spatial (≤1 mm) and temporal resolution, which can be derived from a single CT scan. Areas of CT hypoperfusion correlate best with areas of abnormal voltage (<1.5 mV) rather than scar alone (<0.5 mV). Perfusion imaging from CT enables characterization of the transmural extent and intramyocardial location of scar tissue and visualization of surviving mid- and epicardial myocardium in the regions of scar, which can help identify areas potentially involved in the VT substrate. Such preprocedural information can help the operator plan an appropriate mapping and ablation strategy and better inform the patient about the risks, benefits, and chances of procedural success.12
The 3-D CT-defined abnormal myocardium can be accurately extracted and embedded in clinical mapping systems displaying areas of abnormal anatomical, dynamic, and perfusion parameters for substrate-guided VT ablations.12 Additionally, CT epicardial fat imaging can be used to characterize the extent of fat tissue by extracting and integrating epicardial fat information into the 3-D electroanatomical voltage map, thereby helping to distinguish epicardial fat from scar tissue.13
Anatomical Considerations
The pericardium is a double-walled, flask-shaped sac that contains the heart and the roots of the great vessels, superior vena cava (SVC), and pulmonary veins (PVs). By separating the heart from its surroundings—the descending aorta, lungs, diaphragm, esophagus, trachea, and tracheobronchial lymph nodes—the pericardial space allows complete freedom of cardiac motion within this sac.10
The pericardium consists of two sacs intimately connected with one another: an outer fibrous envelope (the fibrous pericardium) and an inner serous sac (the serous pericardium). The fibrous pericardium consists of fibrous tissue and forms a flask-shaped bag, the neck of which is closed by its fusion with the external coats of the great vessels, while its base is attached by loose fibroareolar tissue to the central tendon and to the muscular fibers of the left side of the diaphragm. The fibrous pericardium is also attached to the posterior sternal surface by superior and inferior sternopericardial ligaments.10 These attachments are essential to maintain the normal cardiac position in relation to the surrounding structures, to restrict the volume of the thin-walled cardiac chambers (right atrium and ventricle), and also to serve as direct protection against injuries.
The serous pericardium is a delicate membrane that lies within the fibrous pericardium and lines its walls; it is composed of two layers: the parietal pericardium and the visceral pericardium. The parietal pericardium is fused to and inseparable from the fibrous pericardium. On the other hand, the visceral pericardium, which is composed of a single layer of mesothelial cells, is part of the epicardium (i.e., the layer immediately outside of the myocardium) and covers the heart and the great vessels except for a small area on the posterior wall of the atria. The visceral layer extends to the beginning of the great vessels, and is reflected from the heart onto the parietal layer of the serous pericardium along the great vessels in tubelike extensions. This happens at two areas: where the aorta and pulmonary trunk leave the heart and where the SVC, IVC, and PVs enter the heart.10 The serous pericardium is also metabolically active.
At the pericardial reflections and at the posterior wall between the great vessels, the pericardial space is divided up into a contiguous network of recesses and sinuses. There are three sinuses in the pericardial space: the superior sinus, the transverse sinus, and the oblique sinus. The superior sinus (superior aortic recess) lies anterior to the upper ascending aorta and main pulmonary artery. The transverse sinus is limited by a pericardial reflection between the superior PVs and contains the right pulmonary artery. The oblique sinus is confined by the pericardial reflections around the PVs and the IVC. The postcaval recess lies behind the SVC, the right pulmonary artery, and the right superior PV. The right and left PV recesses extend between their respective superior and inferior PVs.10
The pericardial cavity or sac is a continuous virtual space that lies between the parietal and visceral layers of serous pericardium. The heart invaginates the wall of the serous sac from above and behind, and practically obliterates its cavity, the space being merely a potential one. The sac normally contains 20 to 40 mL of clear fluid that occupies the virtual space between the two layers. Because all pericardial reflections are located basally in relation to the great vessels, the entire epicardial surface is accessible from the pericardial space, except for the atrial and ventricular septa, which are not in direct contact with the pericardium. Unlike the endovascular approach, the pericardial space is notable for the absence of obstacles and the relative ease with which catheter manipulation can be performed.10 By the same token, achieving firm, stable contact with the catheter tip at the target site may be difficult.
Technical Considerations
The subxiphoid approach procedure may be performed under conscious sedation, deep sedation with the support of an anesthesiologist, or general anesthesia. Deep sedation or general anesthesia allows better control of respiratory motion, which can potentially reduce the chance of unintentional RV puncture, as well as better pain control, given the fact that epicardial radiofrequency (RF) ablation is usually associated with significant pain and patient discomfort. On the other hand, if patients are paralyzed under general anesthesia, diaphragmatic motion with phrenic nerve stimulation during pacing may not occur to warn of proximity of RF applications.4 Intravenous antibiotics should be routinely administered within an hour prior to the procedure. Previous heparin administration should be reversed before pericardial access; this is accomplished by protamine infusion to decrease the activated clotting time to less than 150 seconds.
Initially, catheters are positioned in the CS and RV apex through the femoral approach. The pericardial space is accessed using a 17- or 19-gauge Tuohy needle (Codman Inc., Raynham, Mass.), which is also used to enter the epidural space when administering epidural anesthesia (typically approximately 100 mm in overall length and a 1.5-mm outer diameter). The puncture is performed at the angle between the left border of the subxiphoid process and the lower left rib, with the needle pointing to the left shoulder. The puncture needle approaches the site with a shallow angle in order to penetrate the skin and slide under the rib cage. After crossing the subcutaneous tissue, the stylet is removed, and a 10-mL syringe containing 1% lidocaine or a nonionic contrast agent is attached to the proximal port of the needle. The needle is then advanced under fluoroscopic guidance (40-degree left anterior oblique [LAO] view or, preferably, biplane right anterior oblique [RAO] and LAO projections) until close to the cardiac silhouette. The needle angle is adjusted according to the region that the operator wishes to access. Directing the needle superiorly at a relatively shallow angle, aiming for the RV apex in the RAO projection, generally allows entry into the pericardial space anteriorly over the RV and facilitates access to the anterior aspect of the RV and LV. Directing the needle more posteriorly and toward the left shoulder allows it to enter the pericardium over the diaphragmatic portion of the heart, such that the sheath typically tracks along the posterior aspect of the LV, as observed in the LAO projection. The medial third of the RV is the preferred entry region because of the absence of major coronary vessels in this region.9,14
In the 40-degree LAO view, injection of a small amount of contrast (approximately 1 mL) can help assess the relation of the needle to the parietal pericardium (Video 21  ). If the diaphragm has not been reached, the contrast will be seen in the subdiaphragmatic area. Once tenting of the pericardium is seen, a slight advance achieves entry into the space, and often one can feel the “pop” as the needle penetrates the fibrotic parietal pericardial wall. Contact of needle with the myocardium can be suggested by tactile feedback, occurrence of ventricular ectopy, or observation of a current of injury from a crocodile clip attached to the shaft of the needle. In this setting, further advancement of the needle can result in ventricular puncture and should be avoided.15
). If the diaphragm has not been reached, the contrast will be seen in the subdiaphragmatic area. Once tenting of the pericardium is seen, a slight advance achieves entry into the space, and often one can feel the “pop” as the needle penetrates the fibrotic parietal pericardial wall. Contact of needle with the myocardium can be suggested by tactile feedback, occurrence of ventricular ectopy, or observation of a current of injury from a crocodile clip attached to the shaft of the needle. In this setting, further advancement of the needle can result in ventricular puncture and should be avoided.15
When the needle reaches the pericardial sac, aspiration without blood indicates that the needle has not entered the RV, and injected contrast will spread around the heart, restricted to its silhouette. In some cases, the needle will get close enough to the heart, but the contrast will not be clearly identified in the pericardial sac. In this situation, despite the needle being out of the pericardial sac, it is likely that a defect has been created in the membrane, through which it is possible to advance a soft-tipped guidewire and enter the pericardial sac. If the needle is not close enough to the pericardial membrane, the guidewire will move toward the subdiaphragmatic area. In these cases, the wire must be pulled back and small movements with the needle and the wire must be performed until the pericardial space is reached.9
Confirmation that the wire is intrapericardial and has not been inadvertently inserted into a cardiac chamber is obtained by observing the course of the wire in multiple fluoroscopic projections confirming that it crosses multiple cardiac chambers, hugging the edge of the cardiac silhouette in the 40-degree LAO view, circumferential to both the right and left heart, and without induction of PVCs. Observation in the RAO or anterior-posterior projection alone can be misleading, as a wire that enters the RV and passes into the right atrium (RA) or pulmonary artery can be misinterpreted as intrapericardial.9,15
Inadvertent RV puncture is not rare, but is usually benign if only the needle or wire has entered the chamber in a patient who is not anticoagulated. When the RV is inadvertently entered with the needle (indicated by aspiration of blood or contrast injection passing to the pulmonary artery), the needle can be withdrawn slightly (reentering the pericardial space after exiting the ventricle); contrast injection can then show silhouetting of the heart, and at that point the guidewire is advanced into the pericardial space. The small hole in the RV generally seals without incident. If the dilator and sheath have been passed into the RV, the larger hole may require surgical repair.4
Attempted epicardial access fails in approximately 10% of patients. The percutaneous approach to the pericardial space can be difficult in patients with pericardial adhesions (e.g., following cardiac surgery or pericarditis). In postsurgical patients, the adhesions are mostly concentrated in the anterior portion of the heart; therefore, the puncture must be directed toward the diaphragmatic area. In contrast, adhesion can be more diffuse in postpericarditis patients. Surgical creation of a subxiphoid pericardial window and manual dissection and lysis of the lesions to allow catheter mapping and ablation in the EP laboratory have been shown to be feasible in a small series.4
There is concern that abrasion or laceration of pericardial structures can occur by the edges of a stiff sheath if the sheath is left in the pericardium without a catheter protruding from the lumen. Therefore, it is recommended not to leave a large sheath in the pericardial space without a catheter in place. Also, it is important to lead with a wire or ablation catheter before advancing or moving the curl of the sheath to avoid damaging epicardial structures.9
Before introducing the mapping-ablation catheter, the sheath must be aspirated to check for bleeding. Approximately 10% to 20% of patients experience pericardial bleeding, particularly if inadvertent RV puncture has occurred. Bleeding is managed by frequent aspiration from the pericardial access sheath. It is not uncommon to aspirate 10 to 30 mL of bloody drainage from the pericardial sheath early in the procedure. At this point, anticoagulation should not have been administered; therefore, any bleeding should be self-limited and is generally considered a minor complication because it is not necessary to interrupt the procedure. Major bleeding is rare, and it can be related to the learning curve. Systemic anticoagulation with intravenous heparin is started when subsequent LV endocardial mapping, coronary angiography, or both are desired only after verifying the absence of continued pericardial bleeding.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 ). If it is necessary to insert another catheter, a second guidewire can be advanced through the sheath, which should be removed, leaving two wires inside the pericardial space. Subsequently, a separate sheath is introduced over each of the guidewires. Alternatively, a second puncture of the pericardial sac may be performed, using the same steps described for the first puncture. Before removing the dilator out of the sheath, the sheath must be pushed against the chest to ensure that the tip of the sheath is placed inside the pericardial sac. Although using a standard 15 cm, 8 Fr sheath may suffice for inferior wall VT circuits, the use of longer sheaths (e.g., Agilis; St. Jude Medical, St. Paul, Minn.) should be considered, especially in patients with a larger thoracic anteroposterior dimension.
). If it is necessary to insert another catheter, a second guidewire can be advanced through the sheath, which should be removed, leaving two wires inside the pericardial space. Subsequently, a separate sheath is introduced over each of the guidewires. Alternatively, a second puncture of the pericardial sac may be performed, using the same steps described for the first puncture. Before removing the dilator out of the sheath, the sheath must be pushed against the chest to ensure that the tip of the sheath is placed inside the pericardial sac. Although using a standard 15 cm, 8 Fr sheath may suffice for inferior wall VT circuits, the use of longer sheaths (e.g., Agilis; St. Jude Medical, St. Paul, Minn.) should be considered, especially in patients with a larger thoracic anteroposterior dimension.





