CHAPTER 133 Endoscopic Discectomy and Foraminal Decompression
INTRODUCTION
Endoscopic disc surgery is evolving rapidly because of improvements in surgical technique, endoscope design, adjunctive surgical tools, and instrumentation. New endoscopes and complementary surgical devices enhance the endoscopic spine surgeon’s ability also to probe spinal anatomy in a conscious patient. The surgeon can then evolve his or her diagnostic and surgical skills with this newly found ability to evaluate pathologic, anatomic, and physiologic processes causing the patient’s pain. Now that diagnostic spinal endoscopy can be performed, conditions previously not even considered for surgery may be probed, evaluated, and surgically treated, and perhaps with greater accuracy. We believe that our understanding of discogenic back pain is enhanced by this ability to endoscopically visualize lesions not previously seen intradiscally and in the ‘hidden’ extra-foraminal zone.1 Spinal endoscopy is poised to parallel the development and evolution of knee, shoulder, and ankle arthroscopy.2 Without endoscopy, spine surgeons must depend heavily on imaging systems that, while extremely sensitive in identifying pathologic conditions, do not always correlate that condition with the patient’s pain.
Interventional pain management complementing endoscopic surgery
Foraminal epidurography and foraminal therapeutic injections can be performed using a needle technique that mimics the surgical approach to the foramen and spinal canal.3 The approach differs from traditional interventional pain management ‘down the tunnel’ approaches because it is the same far lateral approach used by endoscopic spinal surgeons to access the foramen for endoscopic surgery. The tip of the needle is directed into Kambin’s triangle between the exiting and traversing nerve root, rather than at the shoulder of the exiting nerve root. If non-ionic contrast agent (i.e. Isovue 300) is injected to outline the foramen, it should be able to identify the location and position of the traversing and exiting nerves that cross each spinal level (Fig. 133.1). Anomalous configurations such as conjoined nerves or furcal nerves provide additional information regarding the anatomy of the lumbar spine. In fact, these anomalies are rarely observed with magnetic resonance imaging (MRI) but are routinely visualized with spinal endoscopy in the ‘hidden zone’ or far lateral zone of the foramen.1,18,19 Diagnostic and therapeutic information gleaned from these modified injection procedures can be used by the surgeon to better select patients for surgical intervention. Patients with symptomatic disc protrusions, annular tears, and foraminal stenosis may first be diagnosed by discography followed by foramino-epidurography, then get relief with the therapeutic foraminal injection. If the response is favorable but short lived, the diagnostic and therapeutic process will help the surgeon with patient selection. As a bonus, the epidurogram will help determine the ease and feasibility of endoscopic surgery because it allows for a trial needle placement into the foramen before surgical intervention.
Endoscopic surgery following injection therapy
Patients who experience temporary relief with injection procedures directed toward the pain generator may realize definitive relief with endoscopic or surgical correction of the pathoanatomy. Our treatment process entails directing a needle to the pain generator, desensitizing or anesthetizing it, dilating a path that will allow a tubular retractor to be inserted, followed by an operating endoscope. Evocative discography™ is helpful in identifying the disc as a pain generator in axial back pain and sciatica.4 When spinal endoscopy and probing complements discography performed with the patient in an aware state, the pathoanatomy and normal anatomy can be visually correlated with imaging studies. In the authors’ experience, new information or information different from the MRI interpretation occurs 30% of the time.4
INDICATIONS
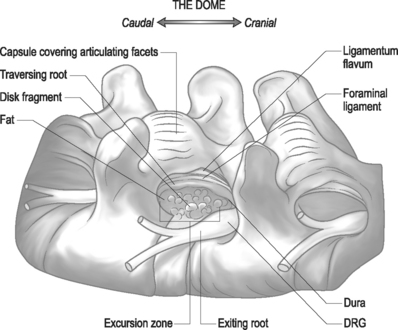
In general, the indications for diagnostic and/or therapeutic endoscopy require a pathologic lesion that is accessible, visible, treatable, or requires endoscopic confirmation through the foramen.5 Limitations of the surgeon’s skill and/or experience with the endoscopy or difficult spinal anatomic are the primary contraindications, exclusive of comorbidities such as infection or uncontrolled coagulopathy.6 For herniations from T10 to L4, the foraminal approach provides excellent access to the disc and epidural space (Fig. 133.2). At L5–S1, anatomic restrictions may cause the surgeon to opt for the posterior transcanal approach. As surgeon experience increases, anatomy that previously precluded spinal endoscopy is no longer a barrier.7 Anatomic structures within reach of the spine endoscope transforaminally are illustrated in Figure 133.3.
Disc herniation
Symptomatic disc herniation is the most common indication, with surgical decompression limited only by the accessibility of endoscopic instruments to the herniated fragment.8,9 The posterolateral foraminal approach is ideal for a far lateral, extraforaminal disc herniation. Traditional surgical approaches to far lateral, extraforaminal disc herniations are more difficult, requiring a paramedian incision through the vascular intertransverse ligament. This surgical area is often termed the ‘hidden zone.’1 Although the lateral zone of the disc can be accessed with a paramedian incision, in our view, it is easier to access the extraforaminal zone endoscopically via the posterolateral portal. A typical foraminal view of nucleus pulposus extruded past the posterior annulus is shown (Fig. 133.4). In our experience, this is the preferred approach for disc herniations in the upper lumbar and lower thoracic spine since the transcanal approach will require more extensive laminectomy that may destabilize the spinal segment if the herniation is above L3–4.
Discitis
Endoscopic excisional biopsy and disc space debridement is ideal for surgically debriding infectious discitis (Fig. 133.5).10 With this technique the surgeon will not have to be overly concerned about creating dead space for the inflamed or infected disc material to spread into the dead space created by a posterior approach. The clinical results are dramatic and, we believe, tissue biopsy is more accurate than needle aspiration in identifying the cause of discitis. In our experience, even sterile discitis will benefit from intradiscal debridement and irrigation.
Lateral recess and central stenosis
Endoscopic foraminoplasty by endoscopic techniques can be accomplished by experienced endoscopic surgeons.6,11,12 Although trephines, rasps, and burrs can be utilized, the Ho:YAG laser has enhanced the procedure technically, as laser is a very precise cutting tool for visually controlled soft tissue and bone ablation. Endoscopic laser foraminoplasty (ELF) has an inherent advantage over classic surgery as it will not produce further instability (Fig. 133.6).13 With endoscopy, the foramen can be enlarged up to 45.5% versus the 34.2% attainable with the standard posterior technique of removing only the medial one-third of the facet. As well, posterior decompression of the lamina with removal of the medial one-third of the facet will produce increased extension and axial rotation postoperatively.13 In comparison, endoscopic foraminoplasty has not been shown to cause increased instability, even in spondylolisthesis.12 The technique is most useful for lateral recess stenosis. In central spinal stenosis, when there is concomitant posterior disc protrusion, decompression of the spinal canal can be effectively accomplished by resecting the bulging annulus in a collapsed disc, thus lowering the floor of the foramen without destabilizing the spinal segment. In isthmic spondylolisthesis, when there is more leg pain than back pain, this is usually due to impingement on the exiting nerve by the pars pseudoarthrosis defect. The goal in this instance is to decompress the compromised exiting nerve by elevating the dome formed by the undersurface of the superior articular facet and lamina without further destabilizing the spinal segment (Fig. 133.7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree