Endoscopic Carpal Tunnel Release: Chow Technique
James C. Y. Chow
James Campbell Chow
Athanasios A. Papachristos
INTRODUCTION
Historical Note
Sir James Paget first described a median nerve compression following a distal radius fracture in 1854 (1). Subsequently in 1880, James Putman, a neurologist from Boston, reported similar symptoms in a group of his patients. The first formal description of a surgical decompression for the treatment of this condition was reported in 1933 followed by Phalen’s classic article in 1950. Since then, open carpal tunnel release has been established as the gold standard for the surgical treatment of carpal tunnel syndrome.
Dr. James C.Y. Chow began working on an endoscopic release of the transverse carpal ligament in 1985, unaware that Dr. Ichiro Okutsu in Japan as well as Dr. John Agee in California were concurrently and separately working toward similar goals. The primary motivation of Dr. Chow’s concept was to create a method for the surgical treatment of carpal tunnel syndrome that would be able to preserve the unaffected surrounding normal anatomic structures of the wrist and hand. Through these pursuits, Dr. Chow developed the slotted cannula late in 1986. After a thorough cadaveric trial period, the procedure was completed in May 1987, and it was performed in a patient for the first time in September of the same year.
The first two reports in the literature on endoscopic carpal tunnel release (ECTR) Chow et al. (2). In the next year, Chow presented a conference paper based on his clinical results after ECTR in 149 cases at the 1990 AANA Annual Meeting in Orlando, Florida. In the fall of the same year, another conference paper by Agee et al. (3) was presented at the 1990 American Society for Surgery of the Hand Annual Meeting in Toronto, Canada, regarding the clinical results of a multicenter study with the use of the Agee technique for the endoscopic release of the carpal ligament. Since the publishing of the three original endoscopic carpal ligament release techniques, there has been an increasingly continuous interest and much debate among surgeons regarding the safety and efficacy of the endoscopic procedure versus that of the open one. Several modifications and variations to the three original ideas have been made since their initial demonstration.
Anatomy/Pathoanatomy
The carpal tunnel is bounded deeply by the volar surface of the distal radius, ulnarly by the hook of hamate, radially by the scaphoid, and superficially by the confluence of the rather stout transverse carpal ligament, palmar aponeurosis, and antebrachial fascia. The carpal tunnel contains nine tendons (the flexor digitorum sublimus and profundus to all four fingers and the flexor pollicus longus) as well as the median nerve.
Carpal tunnel syndrome is a compressive neuropathy of the median nerve at the wrist. As such, it can result from any etiology that increases intracarpal tunnel pressure. This can include irritation and swelling of any of the nine flexor tendons and their tenosynovium, edema of the median nerve itself, anatomical abnormality or scarring of any of the bordering structures of the carpal tunnel, anomalous lumbrical anatomy, an intracarpal tunnel mass (such as a deep ganglion cyst), or stiffening and contracture of the transverse carpal ligament itself.
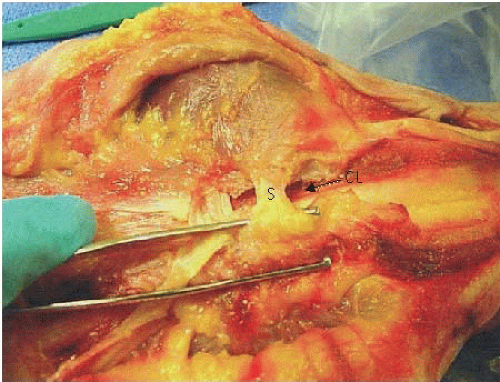
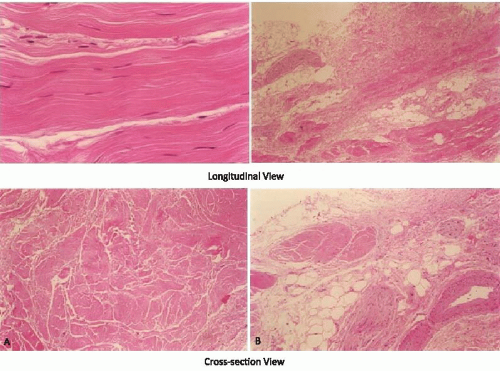
Over the past 25 years of endoscopic carpal ligament release surgery, an otherwise undescribed soft tissue structure has become evident. Further cadaver dissection has revealed an additional soft-tissue band, volar to the resected carpal ligament. This soft tissue band courses between the thenar and the hypothenar musculatures (Fig. 44.1). Microscopic examination shows this band to be a distinct structure when compared with the transverse carpal ligament. While the carpal ligament is formed solely by compact collagen fibers, this soft tissue band contains small nerves and vessels (Fig. 44.2). In reference to its location, the authorship has named this structure the “intramuscular soft-tissue band.” Because of its location and histology, the authorship believes that the preservation of this anatomy is paramount for the rapid recovery seen in ECTR compared with open carpal tunnel release. Theoretically, this can be attributed to (1) prevention of bowstringing of the flexor tendon, (2) decreased pain (possibly pillar pain),
(3) decreased bleeding, and (4) increased muscle strength of the thenar and hypothenar muscles.
(3) decreased bleeding, and (4) increased muscle strength of the thenar and hypothenar muscles.
CLINICAL EVALUATION
Carpal tunnel syndrome accounts for approximately 463,673 carpal tunnel releases performed annually in the United States (4). Patients who have developed this syndrome usually present with a history of characteristic symptoms such as nocturnal pain and paresthesias, numbness in the median nerve distribution distal to the wrist, and thenar muscular weakness. In addition, the physician should be aware of the patient’s general health condition and family history. Congenital diseases or anomalies, connective tissue diseases, systemic and metabolic disorders, and a previous sustained injury to the distal forearm and wrist should be taken into consideration.
Physical examination is critical for accurate diagnosis. In an acute case, there is tenderness along the carpal canal area. Light percussion over the median nerve at the wrist area produces an “electric current” sensation that radiates to the median nerve distribution known as Tinel sign. Phalen sign is evoked by holding the wrists at maximum flexion and the dorsal aspects of the hands in full contact such as a “reverse praying” position. This position narrows the carpal canal and if it reproduces the paresthesias in the fingers within 60 seconds, the sign is considered positive. As the pathologic condition advances, less time is necessary to evoke a response. Other examinations include the monofilament test, two-point discrimination, reverse Phalen’s test, and tourniquet test. In the late stages, with thenar muscle atrophy, one can observe the muscle waste in the thenar area. Muscle weakness is tested subjectively by resisted palmar abduction of the thumb against the examiner’s index finger and comparison of one hand with the other.
A carefully performed history and physical examination can help the physician distinguish between an isolated compression neuropathy at the wrist and a double crush syndrome (5). Clinical correlation of the double crush phenomenon has been demonstrated by the high incidence of concurrent carpal syndrome in patients with
cervical radiculopathy. An equally high incidence of associated carpal tunnel syndrome with a more proximal entrapment of the median nerve has also been reported (6). Therefore, the physician must concomitantly exclude thoracic outlet syndrome, pronator compression syndrome in the forearm, and CNS disease.
cervical radiculopathy. An equally high incidence of associated carpal tunnel syndrome with a more proximal entrapment of the median nerve has also been reported (6). Therefore, the physician must concomitantly exclude thoracic outlet syndrome, pronator compression syndrome in the forearm, and CNS disease.
Electromyography and nerve conduction velocity (NCV) tests aid in the detection of carpal tunnel syndrome. Indications for surgery should not be decided or altered according to the results of NCV tests, especially when the results are normal but the patient has the clinical signs and symptoms of the syndrome. A delay of the distal latency of the median nerve of 7.0 milliseconds or longer represents significant compression of the median nerve; if present, surgery should be considered without further delay. The most important aspects in diagnosing carpal tunnel syndrome are the history and physical examination. Electrodiagnostic studies of the median nerve are an adjunct used to confirm the diagnosis and perhaps suggest how the patient will respond to surgery.
Wrist radiography can rule out the possibility of congenital or acquired bone and joint deformity, abnormality, or pathology. Previously sustained fractures of the distal forearm and wrist should be taken into consideration. A malunited fracture of the distal radius, previously performed surgery in the wrist area, and a hypoplastic or aplastic hook of the hamate (7) can produce difficulties for the surgeon while placing and operating through the slotted cannula. Therefore, standard anteroposterior and lateral views of the distal forearm-wrist and a tunnel view of the wrist are required. If a more extensive study is indicated, MRI, CT scan, ultrasound, bone scan, or arthrogram of the wrist may be necessary.
TREATMENT
Conservative Management
Conservative management includes daily or nightly wrist splinting, alteration of daily activities, physical therapy, and nonsteroidal anti-inflammatory oral medication. Intracarpal tunnel steroid injections have been used with varying reported success.
Open versus Arthroscopic Management
The indications for the open surgical release of transverse carpal tunnel ligament have been well established and, in most cases, they apply to ECTR.
The advantages of endoscopic over open carpal tunnel release include the following: no hypertrophic scar or scar tenderness, no pillar pain, less compromise to pinch or grip strength, and an earlier return to work and daily activities. However, ECTR has the potential to become a dangerous procedure if performed by an inexperienced surgeon (8). Considerable intraoperative complications have been reported throughout the United States by surgeons using this technique (9, 10). This situation has raised a controversy among surgeons regarding the value of endoscopic carpal tunnel surgery. However, it has also been shown that ECTR can be performed safely by experienced surgeons. Despite its steep learning curve, ECTR can give both the patient and the surgeon a great deal of satisfaction (11). As the knowledge, technique, and instrumentation have evolved, the safety of ECTR has improved.
AUTHORS’ PREFERRED TREATMENT: TWO-PORTAL ENDOSCOPIC TECHNIQUE
The original technique was described by Chow as a transbursal approach to the carpal tunnel requiring penetration of the ulnar bursa. Based on the results of a multicenter study, the original technique has been modified in an attempt to decrease the complications and the learning curve. The conversion to an extrabursal technique has made the surgical procedure much easier and safer, thus offering a better visualization of the proximal transverse carpal ligament. The following is a description of the extrabursal, dual-portal technique.
Operating Room Setup
The patient is placed in a supine position and a hand table is used. Two video monitors are preferred, although some surgeons can manage the procedure with only one. One of the two monitors should face the surgeon and the other should face the assistant. The surgeon sits on the ulnar side of the patient and the assistant faces the surgeon (Fig. 44.3). The arthroscopic equipment consists of a short 4.0 mm × 30° video endoscope that prevents light guide from interfering with the patient’s forearm by having the light post on the same side as the direction of view, a camera apparatus, a light cord, a camera input device, and a light source device. Optional equipment includes a DVD video recorder and a video printer for the printing of any captured images. Water pump and shaver equipment are not used.
A standard handset should be available. Specific instrumentation for the procedure, designed by Dr. Chow,
comprises an ECTRA System Kit and an ECTRA Disposable Kit (Smith & Nephew Endoscopy, Andover, MA). The ECTRA System Kit includes the video endoscope, slotted cannula, dissecting obturator, curved blunt dissector, palmar arch suppressor, probe, retractors, and hand holder. The dissecting obturator is attached with a detachable handle that can also take some other types of obturators included in the kit (conical or boat-nose obturator), although the latter is not being used routinely. The ECTRA Disposable Kit includes a probe knife, a triangle knife, a retrograde knife, a hand pad, and swabs. These knives allow the surgeon to determine both the direction and the depth of cut. Standard preparations and draping are performed as usual without the application of a tourniquet. Before the introduction of local anesthesia, a skin marker is used to map landmarks for the entry and exit portals.
comprises an ECTRA System Kit and an ECTRA Disposable Kit (Smith & Nephew Endoscopy, Andover, MA). The ECTRA System Kit includes the video endoscope, slotted cannula, dissecting obturator, curved blunt dissector, palmar arch suppressor, probe, retractors, and hand holder. The dissecting obturator is attached with a detachable handle that can also take some other types of obturators included in the kit (conical or boat-nose obturator), although the latter is not being used routinely. The ECTRA Disposable Kit includes a probe knife, a triangle knife, a retrograde knife, a hand pad, and swabs. These knives allow the surgeon to determine both the direction and the depth of cut. Standard preparations and draping are performed as usual without the application of a tourniquet. Before the introduction of local anesthesia, a skin marker is used to map landmarks for the entry and exit portals.
Anesthesia
Local anesthesia combined with intravenous medication is recommended for the procedure because it allows the patient and the surgeon to communicate. An alert patient can inform the surgeon, during the procedure, about any abnormal sensation in the hand, indicating a potential problem from any variance of nerve structure in the wrist and palm region (12-14). Usually, when the patient first comes into the operating room, fentanyl citrate (Sublimaze) (Baxter Healthcare Corporation, Westlake Village, CA) 100 µg is given intravenously. This is a narcotic analgesic type of medication with an onset period of 7 to 8 minutes and a peak action of approximately 30 minutes. Normally, the surgical time does not exceed 10 minutes. Xylocaine 1% (Astra, Westboro, MA) without epinephrine is injected at the entry and exit portals, approximately 2 to 3 cc at the entry portal and 6 to 7 cc at the exit portal owing to the higher degree of sensitivity of the skin on the palmar region. Special care is taken to limit the injection to the skin and subcutaneous tissue and to avoid affecting the nerve by penetrating deeply.
Positioning the Entry Portal
The proximal end of the pisiform bone is palpated on the volar surface of the wrist within the flexor carpi ulnaris tendon at the distal wrist flexor crease and is marked with a small circle. A line from the proximal pole of the pisiform is drawn radially, approximately 1.0 to 1.5 cm in length. From this point, a second 0.5-cm line is drawn proximally. A third dotted line, approximately 1.0 cm in length, is drawn radially from the proximal end of the second line to create the entry portal (Fig. 44.4A). The average dimensions of these lines will vary slightly, depending on the overall size of the hand.
Positioning the Exit Portal
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree