Endoscopic and Anterior Approaches for Spinal Deformity Surgery in the Adolescent and Young Adult
Mark B. Dekutoski
Mark Pichlemann
Jeremy L. Fogelson
INDICATIONS
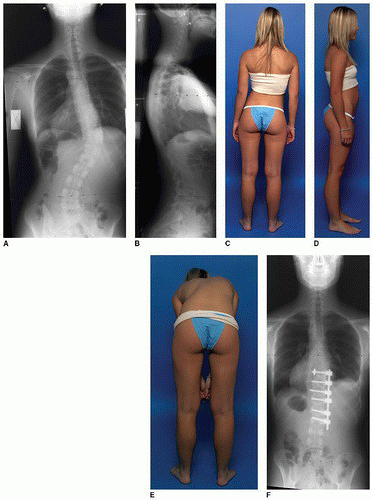
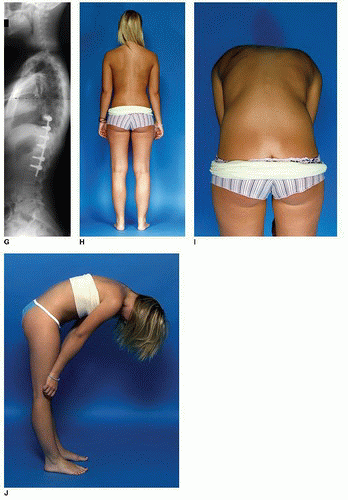
Contemporary open thoracolumbar approaches for anterior scoliosis correction and fusion have been modeled after the early technique popularized by John Hall from Boston Children’s Hospital in the late 1980s. The typical curve patterns for which this technique is most appropriate are thoracolumbar curves, which we now classify as Lenke V or VI curves. Patient selection and informed patient choice in choosing anterior versus posterior approaches need to be thoughtfully and thoroughly reviewed with the family. The patient depicted in Figure set 14-1 has a Lenke Vb thoracolumbar curve as depicted in Figure 14-1A and B radiographically and clinically in Figure 14-1C and D. Confirming that the patient’s proximal and distal curves are nonstructural is critical for restoration of the trunk shift demonstrated in Figure 14-1C. Her significant rib hump demonstrated in Figure 14-1E also responds favorably to the derotation effected by 270-degree annulotomy and discectomy and deliberate orthogonal placement of the screws relative to the native rotational axis of the vertebrae. Figure 14-1F and G demonstrate the contralateral locking nut that enhances proximal screw fixation. This concept and implant design was popularized by Dr. Izzy Liebermann while at the Cleveland Clinic in the late 1990s to address the troublesome rate of proximal screw pullout, loss of correction, and potential nonunion noted with the widespread adoption. Figure 14-1G demonstrates osseous union and the patient’s 1-year sagittal profile. Figure 14-1H and I demonstrate the 1-year clinical correction of coronal balance, level shoulders, waist symmetry, and reduction of rib hump on posteroanterior (PA) and forward bend photos. For this patient, a T9 to L2 anterior approach was utilized, whereas with a typical posterior approach, an additional distal segment may have been necessary.
CONTRAINDICATIONS
Delivery of the appropriate surgical intervention with expected outcome and limited complications requires surgeon training and experience coupled with development of clinical and hospital-based teams. Surgical intervention for spinal deformity surgery is one of the most demanding technical and resource-driven procedures in tertiary medical centers. While outstanding results are published from mature centers, these results and outcomes are not generalizable to all orthopedic surgeons or neurosurgeons in spine practice. Specific patient selection, indications, informed patient consent, and technical execution of the breadth of deformity procedures require specialized training. Individual patient counseling needs to be based upon the experience and outcomes of the surgical team.
Use of endoscopic techniques in North America for anterior scoliosis is challenged by the limited number of surgeons and centers that have developed this expertise and the resource consumption associated with the increased surgical times and potential complications. That said, outstanding clinical outcomes have been published by several mature scoliosis centers for endoscopic anterior fusion.
PREOPERATIVE PREPARATION
Patient education and informed patient choice require careful discussion of the known outcomes, and breadth of treatment choices is an obligation of the surgeon team. Discussion of the specific limitations and outcome expectations for the breadth of procedures and evolution of techniques and outcomes should be presented to the patient by the patient care team.
Through the 1980s and 1990s, correction of scoliotic and kyphotic deformity evolved from in situ fusion to use of distraction and nonsegmental fixation. Anterior fusion and early anterior fixation were commonly used in deformity centers to enhance fusion rates, treat pseudoarthrosis, and limit potential for occurrence of crankshaft phenomenon. North American deformity practices represented by the founders of the Scoliosis Research Society and their fellows became adept at open techniques for thoracic and lumbar fusion (3). The commonplace thoracolumbar “sharkbite” with reflection and reconstruction of the diaphragm became a routine approach to adult and neuromuscular deformity. When compared to the high rates of pseudoarthrosis in that era, the morbidity of the anterior approach was quite favorable in the balance of risks and benefits.
In the late 1990s and early 2000s, several international and North American centers became interested in the immediate and long-term pulmonary effects of scoliotic deformity (1,2,4,13




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree