CHAPTER 73 Elbow Disarticulation Amputation
INTRODUCTION
Over the years, advances in upper extremity prosthetics have included improved surgical techniques, preoperative management, postoperative management, and advances in prosthetic technology. In the past decade, the greatest advances have occurred in prosthetic technologies, fabrication techniques, and components to more effectively replace the lost function of the extremity.7
DEMOGRAPHICS
Trauma is the leading cause of upper extremity limb loss, accounting for 80% of upper extremity amputations. Tumor is the most common cause of upper extremity amputation in children. From 1988 to 1996, the rate of trauma and cancer-related amputations declined. This decline was likely due to improved surgical reconstruction, advances in limb-sparing techniques, and prevention through improved occupational safety awareness.6
Following trauma, the decision to attempt limb salvage or proceed with amputation is complex. There is a bias toward limb salvage in upper extremity trauma surgery. The functional demands of the upper extremity are different from the lower extremity. Lack of weight bearing forces, the ability to function with partial sensation, and limited function of upper extremity prostheses are reasons sited for limb salvage and reimplantation.8
ELBOW DISARTICULATION AMPUTATION
In children with upper limb deficiency or amputation, growth and development, bony overgrowth and more rigorous use of a prosthetic device need to be considered. An elbow disarticulation amputation level for this population optimizes residual limb length and avoids bony overgrowth. The slowed humeral growth after elbow disarticulation results in a humeral length at maturity that allows the use of a prosthetic elbow while retaining the suspension and rotational control of an elbow disarticulation.1 In children, transhumeral amputation results in a high incidence of bony overgrowth. An elbow disarticulation preserves the epiphysis, prevents bony overgrowth, and maintains growth potential; therefore, elbow disarticulation is the level of choice.2
AMPUTATION SURGERY
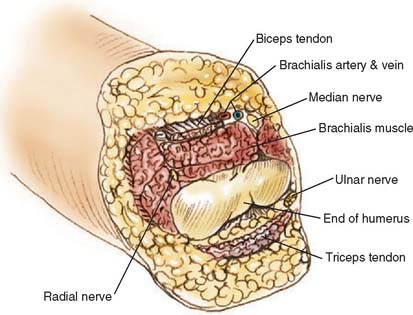
NERVES AND BLOOD VESSELS
Meticulous hemostasis is mandatory to avoid postoperative hematoma formation. All wounds are drained for 48 hours postoperatively.
BONE
Through-elbow amputation is carried out as a true disarticulation (Fig. 73-1). Minor contouring of the margins of the distal humerus is usually required to eliminate sharp condylar prominences. For above-elbow amputations, the bone edges should be slightly beveled so that there are no sharp prominences or rough bone edges.
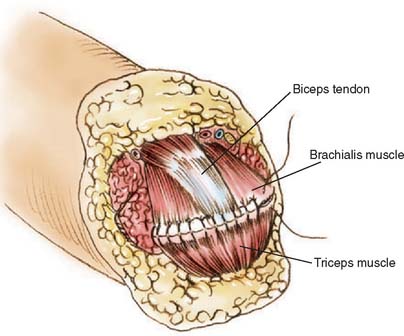
MUSCLE STABILIZATION
Whenever possible, the sectioned muscles and tendons are sewn to each other over the end of the humerus at the amputation site (Fig. 73-2). If possible, the triceps tendon and aponeurosis is retained and brought forward through and over the trochlea to be sewn under minimal tension to the brachialis muscles. The biceps tendon also can be interwoven into the brachialis muscle near the amputation site, giving excellent residual limb muscle control.
NERVE TRANSFERS
In an attempt to improve functional control of myoelectric prostheses, the possibility of transferring residual nerves to spare muscles in or near the residual limb has been studied. Using nerves to reinnervate targeted muscle, the surface myoelectric signals from these muscles have been used to simultaneously control multiple degrees of freedom in a prosthesis.13
Research into this concept has been promising. Studies have shown that when large nerves (such as the brachial plexus nerves) are transferred onto relatively small muscle areas, the recovery of the muscle is very good.12 With targeted reinnervation, control of a prosthesis will be easier and more natural because the myoelectric signals are physiologically correlated to the movements of the lost arm. Although targeted reinnervation shows exciting potential, ongoing research is needed.13
ACUTE POST-AMPUTATION MANAGEMENT
Following surgery, the goals of the preprosthetic period are to
Immediate and early postsurgical prosthetic fitting provides edema control, pain reduction, and protects the surgical incision.14 Successful prosthetic use is higher when fitting is completed within a “golden period” of 30 days after surgery.14 If prosthetic fitting and training are delayed, the patient can become adept at one-handed techniques, making it difficult to incorporate a prosthesis in their daily living activities. A second study has shown that even delayed fitting can be successful.22 Common reasons for rejecting a prosthetic limb include the perception of limited usefulness, excessive weight, and residual limb pain.