Revision Point
Three pairs of salivary glands, which produce saliva, open into the mouth. Name these glands, state their position and where they open into the mouth.
Saliva is largely made up from water (99%) which helps to moisten food. This process helps with taste; the taste buds can only be stimulated by chemical substances that are in solution and have therefore been dissolved in the saliva (Waugh and Grant, 2006). Mucus within saliva aids lubrication of food which enhances swallowing. Swallowing in the absence of adequate volumes of saliva becomes very difficult. The enzyme lysozyme contained within saliva helps to kill bacteria within the mouth. The other enzyme, salivary amylase, begins the chemical breakdown of complex sugars and starch to the disaccharide maltose (Seeley et al., 2003). Saliva has a typical pH of 6.7 which makes it slightly acidic. Sympathetic stimulation of the salivary glands inhibits saliva secretion during stressful moments, resulting in a dry mouth. When stimulated by the parasympathetic division of the ANS, more saliva is secreted to aid with digestion of foodstuffs. Saliva is secreted in anticipation of eating where the mere thought or sight of food will stimulate its release. This release is continued when food enters the mouth and the process of digestion begins.
Once swallowed, food passes through the pharynx and is propelled down the oesophagus by peristaltic action. Peristalsis is the rhythmic contraction of smooth muscles which propels foodstuffs through the digestive tract. The oesophagus passes through the diaphragm and opens into the stomach at the cardiac sphincter.
 Revision Point
Revision Point
Identify the different structures and organs that make up the digestive system.
Table 6.2 Functions of the mouth.
| Mechanical digestion of food |
| Chemical digestion of food |
| Taste |
| Swallowing |
| Speech |
The stomach
The stomach is a ‘J’ shaped organ situated just below the diaphragm. It is divided into four main regions – cardiac region, fundus, body and pylorus. The stomach has a lesser curvature and a greater curvature which provide attachments for folds of the peritoneum.
The gastric wall has three layers of muscle – an outer longitudinal layer, a middle circular layer and an inner oblique layer. These allow for the churning action of the stomach moving food forwards and backwards, a process which aids in the breakdown of food.
The sub-mucosa and mucosa are thrown into folds known as rugae, which greatly increase the surface area for secretion of digestive juices and allow for considerable distension following ingestion of a meal. The gastric mucosa contains deep gastric pits which are the openings for the gastric glands. Cells found within the gastric pits include surface mucous cells which secrete mucus, mucous neck cells which also secrete mucus, parietal cells which secrete hydrochloric acid (HCl) and intrinsic factor (necessary for the absorption of vitamin B12), endocrine cells which secrete the hormone gastrin and finally chief cells which secrete the enzyme pepsinogen.
Mucus protects the lining of the stomach from the actions of gastric juice. HCl acidifies food, stops the chemical breakdown of starch to maltose and converts inactive pepsinogen to the active form pepsin, which breaks down proteins to smaller units called polypeptides (hence beginning the chemical digestion of proteins). Pepsins work best at a pH of 1.5 3.5. Intrinsic factor combines with vitamin B12 to allow for its absorption. The hormone gastrin stimulates gastric glands to release gastric juice.
The contents of gastric juice can be found in Table 6.3.
The functions of the stomach can be found in Table 6.4.
Table 6.3 Constituents of gastric juice.
| Water |
| Mucus |
| Mineral salts |
| Hydrochloric acid (HCl) – pH 1–3 |
| Intrinsic factor |
| Pepsinogen |
Table 6.4 Functions of the stomach.
| Reservoir for food |
| Protection through action of HCl |
| Mechanical digestion (churning of muscles) |
| Chemical digestion through action of enzymes |
| Limited absorption of water, alcohol, glucose and some drugs |
The mechanical and chemical digestion which occurs in the stomach results in a semifluid liquid called chyme. This liquid can remain in the stomach for many hours before eventually being transported into the duodenum.
The small intestine
Chyme passes through the pyloric sphincter into the small intestine, a long tube 7 m in length which lies coiled up in the abdominal cavity. The small intestine is divided into three parts – duodenum, jejunum and ileum.
The duodenum, which is the first part of the small intestine, receives secretions from the pancreas (pancreatic juice) and the gall bladder (bile), both of which release these secretions into the duodenum via the hepatopancreatic ampulla (also known as the ampulla of Vater). The ileum of the small intestine terminates at the ileo-caecal valve leading to the large intestine or colon.
The mucous membrane lining of the small intestine is designed to greatly increase its surface area. It achieves this by the presence of circular folds, villi and microvilli (Figure 6.1). The circular folds around the intestine enhance absorption by causing the chyme to spiral through the intestine rather than moving through in a straight line. This slows the whole process thereby enhancing digestion and absorption. Villi are finger-like projections of the mucosa, richly supplied with blood capillaries, into which the products of digestion
Figure 6.1 Diagram of a villus. (Reproduced from Nair and Peate (2009). With permission from John Wiley & Sons.)
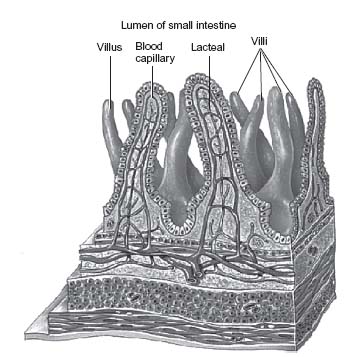
Table 6.5 Hormones necessary for chemical digestion of food.
| Hormone | Released from | Actions |
| Gastrin | Stomach | Stimulates gastric glands to produce gastric juice |
| Enteric gastrin | Small intestine | Continued stimulation of gastric glands |
| Gastric inhibiting peptide | Small intestine | Stops production of gastric juice |
| Secretin | Small intestine | Stimulates release of intestinal juice and pancreatic juice |
| Cholecystokinin | Small intestine | Stimulates release of pancreatic juice and bile |
are absorbed. They also contain a lymphatic vessel or central lacteal into which fatty acids, glycerol and fat-soluble vitamins are absorbed. The microvilli project from the apex of the villi and increase the overall surface area available for absorption. They form a fuzzy line at the apical surface of the villi known as the brush border.
The chyme within the small intestine undergoes chemical digestion from (i) intestinal juice from the intestinal glands, (ii) pancreatic juice secreted by acinar cells in the pancreas and (iii) bile produced by the liver and stored and concentrated in the gall bladder until required.
Tables 6.5 and 6.6 list the hormones and enzymes necessary for the chemical digestion of food.
In the process of chemical digestion, carbohydrates, fats and proteins are broken down to their smallest units of mainly glucose, fatty acids and glycerol and amino acids. This renders them small enough to be absorbed through the gut wall. Most of the absorption of nutrients from the digestive tract takes place through the wall of the small intestine into the blood and lymphatic system.
Absorption of nutrients in small intestine
Glucose absorption
- Monosaccharides enter the epithelial cells of a villus (through the microvilli)
- They leave the epithelial cells to enter a blood capillary within a villus
- They are then transported to the liver via the hepatic portal vein.
Protein absorption
- Amino acids enter the epithelial cells of a villus
- They leave the cells to enter a blood capillary within a villus
- They too are then transported to the liver via the hepatic portal vein.
Table 6.6 Enzymes necessary for chemical digestion of food.
| Enzyme | Released from | Action |
| Salivary amylase | Mouth | Breaks down starch to maltose |
| Pepsin | Stomach | Converts proteins to peptides |
| Rennin | Stomach in infants | Curdles (solidifies) milk |
| Enterokinase | Small intestine | Converts inactive trypsinogen to active trypsin |
| Peptidases | Small intestine | Convert peptides to amino acids |
| Lipase | Small intestine | Converts lipids to fatty acids and glycerol |
| Sucrase | Small intestine | Converts sucrose to glucose and fructose |
| Maltase | Small intestine | Converts maltose to glucose |
| Lactase | Small intestine | Converts lactose to glucose and galactose |
| Trypsinogen | Pancreas | Converted to trypsin by enterokinase. Trypsin converts polypeptides to peptides |
| Chymotrypsinogen | Pancreas | Converted to active chymotrypsin by trypsin. Chymotrypsin converts polypeptides to peptides |
| Carboxypeptidase | Pancreas | Converts polypeptides to peptides and amino acids |
| Pancreatic amylase | Pancreas | Converts polysaccharides to disaccharides |
| Pancreatic lipase | Pancreas | Converts lipids to fatty acids and glycerol |
| Ribonuclease | Pancreas | Converts RNA nucleotides to pentoses and nitrogenous bases |
| Deoxyribonuclease | Pancreas | Converts DNA nucleotides to pentoses and nitrogenous bases |
| Bile | Gall bladder | Emulsifies fat droplets into smaller particles |
Fat absorption
- Bile salts form aggregates called micelles in the small intestine
- Fatty acids and glycerol dissolve into these micelles in the small intestine
- Micelles now come into contact with the surface of the epithelial cells
- Fatty acids and glycerol diffuse into the cells
- Micelles stay behind in the chyme
- Once inside the epithelial cells, the fatty acids and glycerol recombine to form triglycerides (fats)
- Triglycerides unite with cholesterol and become coated with proteins and are now known as chylomicrons
- Chylomicrons leave the epithelial cells and enter the lacteal of a villus
- They are then transported in lymphatic vessels as chyle (this is lymph fluid which is high in lipids)
- The chyle is transported to the thoracic duct and enters the bloodstream at the left subclavian vein
- The fats eventually enter the liver via the hepatic artery.
Activity
Identify which nutrients are absorbed directly into the blood and which are initially absorbed into the lymphatic system. Describe how these nutrients reach the liver once they have been absorbed.
The large intestine
The large intestine extends from the ileo-caecal valve to the anus through which digestive residue is eliminated as faeces. It lies in an arch around the abdominal cavity, surrounding the small intestine. The functions of the large intestine can be seen in Table 6.7.
 Revision Point
Revision Point
Arrange the following parts of the large intestine in the correct order:
- Rectum
- Caecum
- Hepatic flexure
- Ascending colon
- Anal canal
- Sigmoid colon
- Transverse colon
- Descending colon
- Splenic flexure.
Table 6.7 Functions of the large intestine.
| Absorbs water (consolidation of faeces) |
| Absorbs some electrolytes |
| Absorbs vitamin K – synthesised from bacteria in the large bowel |
| Secretes mucus to lubricate faeces |
| Temporary storage of indigestible foodstuffs until they are eliminated from the body |
| Bacteria cause the fermentation of undigested food residues with the production of gases -hydrogen, carbon dioxide and methane |
| Bacteria in the large intestine also synthesise vitamin K and folic acid – a valuable source of these vitamins within the body |
As previously identified, the ileum of the small intestine terminates at the ileo-caecal valve leading to the large intestine. Longitudinal muscles of the large intestine are gathered into three bands known as taeniae coli. Contraction of these bands gathers the colon into a series of pouches known as haustra, which give the colon its puckered appearance.
Movement of the contents within the large intestine occurs via three mechanisms. Haustral churning occurs whilst they receive faecal contents as the haustra remain relaxed and distended. As the distension grows, a critical point is reached when the haustrum contracts and squeezes the contents into the next haustrum. Peristalsis also occurs in the ascending colon of the large intestine at the rate of 3–12 contractions every minute. Finally, mass movements (mass peristalsis) also occur from the middle of the transverse colon to the descending colon which quickly drives colonic contents into the rectum. Mass movements occur 3–4 times every day usually during or after eating (Seeley et al., 2003; Tortora, 2005). It should be noted that mass movements are said to be most common shortly after breakfast (Seeley et al., 2003).
 Point for Practice
Point for Practice
How would you incorporate the above knowledge into a plan of care for older adults in a residential, nursing home or hospital setting?
When the colon’s contents are moved into the descending colon and rectum, stretch receptors stimulate nerves initiating a reflex action of contraction of the rectum and relaxation of the internal sphincter. The external sphincter is voluntarily controlled until a suitable time and place is found in order for defaecation to occur.
Although chemical digestion does not take place in the large intestine, it has a very important function in relation to the absorption of water. Up to 7 l of digestive juices are secreted by the digestive system every day. Without re-absorption of the water and salts from these juices, dehydration would soon result.
 Revision Point
Revision Point
Compare the composition of the contents of the small bowel at the ileo-caecal junction with that in the rectum.
The liver
Although not specifically part of the digestive system, the liver has many functions associated with digestion and nutrients.
The liver is the largest gland in the body weighing about 1.4 kg in an average adult (Tortora, 2005). It lies in the right upper abdomen just under the diaphragm. Much of the liver is shielded by the ribs. It is roughly triangular shaped and is divided into two main lobes (Tortora, 2005). The lobes consist of smaller portions known as lobules in which cells are arranged in columns like spokes of a wheel. Between the columns of cells, the blood flows through incomplete capillaries called sinusoids which allow the blood to come in contact with liver cells. The lobules are made up from specialised epithelial cells called hepatocytes. Amongst other functions, hepatocytes are involved with the formation and secretion of bile. Hepatocytes are also associated with protein synthesis and can store glycogen, vitamins (A, B12, D, E and K), copper and iron (Seeley et al., 2003; Tortora, 2005). Blood vessels, ducts and nerves enter and leave the liver at the portal fissure on its inferior surface.
 Revision Point
Revision Point
1.The liver receives blood from two different vessels. Name these vessels and their origin. Differentiate between the contents of blood carried in the vessels.
2.Trace the passage of bile from its manufacture in the lobules to its entry into the duodenum.
3.Name the substances which the liver
- Stores
- Manufactures
- Detoxifies.
The gall bladder
The gall bladder is located on the inferior surface of the liver and is a pear-shaped sac. It stores, concentrates and excretes bile which is produced in the liver. Bile consists of water, mineral salts, bile salts, bile pigments and cholesterol. The pH of bile is between 7 and 9, making it slightly alkaline. Bile is involved in the chemical digestion of foodstuffs through the action of its bile salts where it emulsifies fat globules into smaller droplets. This action takes place within the small intestine. Bile salts also make cholesterol and fatty acids soluble, enabling these and the fat-soluble vitamins (A, D, E and K) to be easily absorbed.
The pancreas
The pancreas is situated behind the greater curvature of the stomach and consists of a head, body and tail. It secretes pancreatic juice (exocrine function) which leaves the pancreas in ducts that join to form the main pancreatic duct. This joins with the common bile duct and empties into the duodenum at the hepatopancreatic ampulla. Pancreatic juice consists of water, mineral salts, sodium bicarbonate and the enzymes trypsinogen, chy- motrypsinogen, pancreatic amylase and pancreatic lipase.
Sodium bicarbonate is alkaline and therefore neutralises acidic chyme in the small intestine and helps to create an environment conducive for digestive enzyme functioning. The pancreas is involved in the chemical digestion of foodstuffs through the action of its enzymes. Refer to Table 6.6 naming the enzymes necessary for chemical digestion of food.
The pancreas also has an endocrine function where it secretes and releases hormones including insulin, in relation to blood glucose homeostasis.
Ageing changes in the digestive system
There are few alterations in GI function associated with ageing, although cellular changes do occur involving secretory activity and motility of the major structures. These cellular changes are similar to that elsewhere in the body and despite these physiological alterations, GI function is usually maintained in line with body needs.
As already discussed, the major function of the GI system is to provide nutrition to the body. This is achieved by the mechanical and chemical processes of digestion, absorption, storage or movement of foods and excretion of unabsorbed elements.
The liver is the organ most severely affected by ageing. Bile formation stays quite stable in healthy individuals well into old age. The detoxification of both therapeutic and recreational drugs is progressively restricted with advancing age.
Many people lose their teeth by the age of 40 as a result of periodontal disease or infection (Christiansen and Grzybowski, 1999). However, today, older people are more likely to retain more of their natural dentition. This improvement is related to changing attitudes associated with loss of teeth in old age, improved health education and knowledge about dental care, increased use of fluoride (e.g. in water and in toothpaste) and increased availability of dental services (Matteson et al., 1997).
However, the teeth do undergo characteristic changes associated with ageing. They often acquire a yellowish-brown discolouration from staining caused by pigments found in beverages, tobacco and foodstuffs. The presence and action of oral bacteria also contribute to this discolouration (Timiras, 2003).
Tooth enamel becomes less permeable and more brittle, chipping and fracturing easily (Christiansen and Grzybowski, 1999). Within the pulp cavity, nerves degenerate and atherosclerosis affects the tiny blood vessels supplying the teeth, causing the teeth to become brittle (Roach, 2001).
Chewing surfaces on the teeth wear down so that they no longer match well when eating food. The grinding and chewing of food by the teeth results in beneficial chewing stress which helps to maintain bone health in the jaw. Loss or removal of teeth results in a reduction in this beneficial process. Bone loss in the jaw, associated with ageing (osteoporosis), contributes to the loosening of otherwise healthy teeth (Christiansen and Grzybowski, 1999; Timiras, 2003). Despite these changes, loss of teeth is not inevitable (Roach, 2001).
Recession of the gingivae occurs in all older people (Timiras, 2003) and results in an appearance of longer teeth than before, giving rise to the expression of being long in the tooth (Christiansen and Grzybowski, 1999). As gums recede, it becomes more difficult to maintain well-fitted dentures.
Older people are less likely to develop new dental caries. However, loss of interest in dental hygiene and loss of manual dexterity may lead to the build up of plaque and the subsequent formation of dental caries in the older adult (Timiras, 2003).
Structures on the tongue called papillae, many of which contain taste buds, atrophy with age. This atrophy is associated with the loss of taste. The ability to both detect and identify food flavours – salt, sweet, sour and bitter – decreases with age. There may be some increase in taste threshold for salt and sugars, causing bitter tastes to predominate (Deems et al., 1991). Brownie (2006) also states that sweet and salty taste decline first so that food begins to taste sour and bitter. However, Matteson et al. (1997) suggest that the sensation of taste only modestly decreases with age.
Secretions of the salivary glands reduce with age (Matteson et al., 1997), leading to a dry mouth which sometimes makes swallowing difficult (Roach, 2001). Heath and Schofield (1999) state that saliva production can be decreased as a consequence of a reduction in secretory cells by as much as 25% as they are replaced by fibrous or fatty tissue. They go on to claim that from the age of 50, salivary amylase is reduced and this impedes digestion of complex carbohydrates.
Thirst regulation is often affected making dehydration a prime risk among older adults (Lueckenotte, 2000). The sensation of thirst also changes with age (Mack et al., 1994). In older adults, a lack of sensation when the body is becoming fluid depleted may be due to a reduction in hypothalamic awareness of a change in body fluid status. As a result, an older adult can become dehydrated and not realise nor respond to this condition physiologically. Older adults can therefore lose fluids without stimulating the thirst response (Kenney and Chiu, 2001). As such, older adults may not request fluids to drink as they may not feel thirsty.
In the oesophagus, reflex actions triggered by the presence of food drive the contents downwards, through smooth muscle contractions known as peristalsis. These processes require a correctly timed contraction and relaxation order. However, this order can be affected with age, as it may become desynchronised resulting in swallowing difficulties (Timiras, 2003).
By the age of 64, the gastric mucosa has usually undergone some degree of atrophy (Christiansen and Grzybowski, 1999). In healthy older people, the mucosal cells in the stomach and small intestine atrophy and the production of hydrochloric acid is reduced (Roach, 2001; Timiras, 2003). This reduction in acid also decreases the rate of enzyme release such as pepsin which may result in difficulties digesting protein-rich foods (Timiras, 2003). The reduction of the mucous protective layer in the stomach increases the risk of attack from HCl and protein digesting enzymes which can then readily destroy the exposed mucosal cells (Timiras, 2003). A reduction in prostaglandin production associated with ageing contributes to the loss of the gastric mucosa. Prostaglandins enhance bicarbonate release which assists with protection of the mucosa from acid and digestive enzymes. This protective cover is reduced when less bicarbonate is produced associated with a reduction in prostaglandin levels. All of this increases the likelihood of gastritis and peptic ulceration (Timiras, 2003).
Associated with ageing is a decreased elasticity of the stomach, resulting in a reduction in accommodation of food. Gastric emptying is also slower with advancing age (Meiner and Lueckenotte, 2006). Production of intrinsic factor also decreases which is necessary for the absorption of vitamin B12. This can increase the incidence of pernicious anaemia in the older adult (Roach, 2001).
Many factors affect the absorption of digested foodstuffs, including the speed of passage of food through the digestive tract, any alterations to the absorptive surfaces of the digestive tract, the blood supply to the digestive system and the effectiveness of the transport mechanism involved. Dextrose and xylose are absorbed more slowly and fat absorption also tends to be slower in older people (Heath and Schofield, 1999). This can contribute to the feeling of fullness and a resulting reduction in appetite. Absorption of calcium, iron and vitamins B l and B2 decreases with age. The number of villi and microvilli in the small intestine reduce with age. They also decrease in height and increase in breadth, resulting in a significant reduction in mucosal surface area (Matteson et al., 1997). However, because there are more than 4 million villi/microvilli, this reduction in numbers and size does not significantly affect the absorption of most nutrients (Roach, 2001).
Changes in the large bowel include loss of mucosa, excess connective tissue and vascular changes which are largely due to atherosclerosis. The blood vessels supplying the colon may become tortuous which can impede the flow of blood to the colon (Matteson et al., 1997). There is a decrease in overall muscle strength and a reduction in peristaltic actions (Matteson et al., 1997; Roach, 2001). Decreased motility can contribute to the development of constipation which may also be linked to a diet lacking in fibre and fluids or to a lack of exercise (Roach, 2001; Timiras, 2003). There is an increase in the prevalence of diverticula in people over the age of 50, with increasing incidence thereafter. As stated, the presence of diverticulitis is common but it is not entirely clear whether this is related only to age or as a result of a lack of dietary fibre linked to constipation (Roach, 2001).
Frequency of defaecation remains the same after the age of 60 as compared to before 60. However, the volume of distension in the rectum necessary to stimulate the desire to defaecate is larger in older people.
With advancing age, the pancreas may become smaller and harder due to increasing fibrosis. Accumulation of lipofuscin (a pigment associated with ageing) can be noted which is also found on other organs such as the kidneys, heart and liver (Matteson et al., 1997; Timiras, 2003). Only one-tenth of the pancreas is required for normal digestion (Timiras, 2003), therefore the pancreas can be seen to have a large reserve capacity (Matteson et al., 1997). The total volume of secretions from the pancreas reduces after the fourth decade and enzyme release also reduces with age (Meiner and Lueckenotte, 2006). However, despite these changes, the production of bicarbonate, amylase and trypsin remains adequate to meet body demands (Matteson et al., 1997).
Ageing does not appear to affect the gall bladder or bile ducts. However, gallstones are more likely to occur with advancing age (Meiner and Lueckenotte, 2006).
After the age of 70, the liver decreases in size and secretes less enzymes than before. The reduction in size of the liver decreases the space available for storage of nutrients such as proteins, vitamins, minerals and glycogen. The reduction in hepatic enzymes interferes with metabolism and makes the detoxification of drugs more difficult (Roach, 2001).
According to Matteson et al. (1997), the metabolism of drugs may be reduced by as much as 30% from adulthood to old age. There is also a decrease in the production of bile and cholesterol associated with ageing.
The number of hepatocytes in the lobules decline with age. Protein synthesis within these hepatocytes is also reduced. This reduction in protein synthesis is associated with a decrease in enzymatic activity (Christiansen and Grzybowski, 1999). However, changes are usually quite minor and the liver has enough reserve capacity to accommodate these changes. Hepatic cells regenerate throughout life, but the regeneration slows as we age (Timiras, 2003).
Oral hygiene
The aim of oral hygiene is to keep the oral mucosa clean, moist and soft and to prevent the lips from cracking. Any food debris and dental plaque should be removed from the mouth and teeth. These actions should ensure a comfortable mouth and prevent halitosis. Good fluid intake will enhance these actions.
Older people require to have their mouths checked (assessed) and cleaned whether they have their natural teeth or otherwise. This assessment should form part of any admission procedure and should be repeated as often as is necessary. Many older adults living at home will follow a regular pattern of oral hygiene familiar to them. If removed from their home environment for whatever reasons, they should be enabled to follow their typical oral hygiene care patterns for as long as possible.
It should be recognised that many older care settings may not have adequate facilities for the maintenance of privacy and dignity when engaged in personal oral hygiene. Open style ward areas and shared bathroom facilities, inadequate lighting and fixtures which are not easy to reach and use do not enhance or encourage the maintenance of self-care. Furthermore, fixed routines within health-care settings may present as a barrier to independence and actually promote dependence in the care setting (British Society for Disability and Oral Health (BSDH), 2000).
Adams (1996) claimed that nurses in clinical practice lacked relevant knowledge in relation to oral health problems. White (2000) went on to claim that poor clinical knowledge of oral health problems was directly a consequence of poor education relating to oral hygiene and oral health care in nurses preregistration undergraduate programmes. They go on to state that this educational deficit can negatively impact on oral health care needs of older patients.
The ageing process has to be taken into account when considering the oral health needs of older adults. Teeth become loose and increasingly fragile relating to loss of gum tissue. There are changes in tooth structure related to simple wear and tear. As a result of these changes, the teeth are more easily damaged. The sockets in which the upper teeth are housed lose bone tissue, resulting in the teeth becoming slack and easily dislodged. The production of saliva is reduced. Muscles involved in the chewing of food are in some instances, used less, partly in relation to the use of softer food which requires less chewing action. Muscle tone is therefore reduced and over time muscle wasting can become apparent. When the muscles involved in chewing food become atrophied, food remains in the mouth for longer than before. Winkley et al. (1993) suggests that this allows sugars to remain in the oral cavity for longer periods of time which adds to the risk of dental caries.
The taste of food is affected by the presence of plaque and debris in the mouth, which in turn can reduce a person’s appetite and readiness to eat and drink. Without appropriate oral care, patients may develop dental and oral diseases, which can affect eating and drinking (Simons et al., 1999). Good oral health care therefore not only keeps the oral cavity clean and moist, it also helps to maintain appetite and enjoyment of food and drink, thus helping to encourage adequate nutritional and fluid intake.
Speech is affected by the condition of the oral cavity. Ill-fitting dentures and damaged teeth both influence the ability to speak clearly and pronounce words accurately. Infection and inflammation of the mouth also make it difficult for the individual to articulate their words and speak clearly. These conditions not only impact on the person’s ability to communicate with health-care professionals, but also impact on the ability to communicate with friends and family. In turn, this can lead to a withdrawal from family and wider social circles leading to social isolation.
Plaque and debris in the mouth can lead to bad breath or halitosis. Jones (1998) suggested that halitosis affects an individual psychologically and that this condition can negatively influence relationships within the family. Good oral health can help with self- image and self-esteem and enhance general well-being in older adults (Holmes, 1996).
Assessment of oral health
Roberts (2000a) claims that there is little evidence to indicate that oral assessment is taking place in clinical practice. During a global assessment, an assessment of your patient’s oral health status should also be included. An easy to use assessment tool is outlined below. This will allow for appropriate oral care interventions to be put into practice where necessary. During this assessment, advice in relation to improving oral health status can also be offered.
The following areas should be assessed:
- Teeth – identify for presence of plaque, debris and decay. If wearing dentures, are they well fitting?
- Mucous membranes and gums – identify any areas of redness, bleeding or evidence of ulceration
- Tongue – check for size, colour, dryness, cracks or blisters
- Saliva – quantity and quality
- Lips – evidence of cracking, blistering or peeling?
- Halitosis – presence or absence of?
(Adapted from Endacott et al., 2009, p. 82)
A simple, straightforward oral assessment should be completed on admission to a residential care setting (BSDH, 2000). Such an assessment will highlight any oral health problems and help in the planning of good oral care. The oral assessment should be included in the routine assessment by staff.
Nursing management of oral hygiene
There are a number of readily available products which can be used to help maintain good oral hygiene. The toothbrush is the most commonly used and should continue to be used unless the person has difficulties with manual dexterity. A toothbrush should be used to clean both gums and tongue of all patients, even if the person wears dentures. However, toothpaste should not be used to clean dentures as it may damage the denture surface (Clarke, 1993). If your patient is unable to clean their own teeth, the toothbrush remains the most effective means by which good oral hygiene is achieved. Health carers should therefore carry out this skill for them, using an appropriate toothbrush and toothpaste.
As a toothbrush, toothpaste and water are most widely used to maintain good oral hygiene at home, it seems appropriate that this practice should continue if admitted to a care setting (Roberts, 2000b).
The use of lemon and glycerine swabs is no longer recommended as a means to obtain good oral hygiene (Bowsher et al., 1999). The presence of lemon can lower the pH within the oral cavity, leading to a more acidic environment which can be harmful to an older person’s teeth. They also dry out the oral mucosa.
Foam sticks can be used to help cleanse and moisten the oral mucosa (Thurgood, 1994). However, they are not effective if used to remove plaque from the teeth (Bowsher et al., 1999).
The older method of using a gloved finger and a gauze swab cannot be recommended as a means to achieve good oral hygiene. The dangers of being bitten far outweigh the effectiveness of this method. This method can also push debris into gaps between the person’s teeth which if not removed can add to the risk of oral infection.
A variety of mouthwashes are available including chlorhexidine mouthwash which has been shown to be useful in the control of plaque and for its antibacterial and fungicidal properties (Curzio and MacCowan, 2000). Such a mouthwash may be of benefit if your patient finds it difficult in cleaning their own teeth due to manual dexterity problems. Xavier (2000) advises that chlorhexidine is a useful addition to other oral health-care measures.
Although thymol or glycothymol mouthwashes have an initial refreshing action when used, they do not have any lasting beneficial effects (Nicol et al., 2000) or any cleansing actions within the oral cavity (Rattenbury et al., 1999).
The use of a lip lubricant can help to prevent drying and cracking of an older person’s lips.
The eating of fresh fruit and drinking of fruit juices is something to be encouraged whether the older adult is at home or within a care setting. These not only provide essential vitamins but they are also refreshing and help to relieve a dry mouth.
If a person has dentures, they should be encouraged to remove them after each meal and rinse them under running cold water in order to remove any loose debris. If they cannot do this for themselves, a member of staff should perform these actions. It is also advisable to remove dentures overnight as this allows saliva to act upon acids which may have built up on the oral mucosa which would not be exposed if the dentures remain in place. Once removed, they should be cleaned and stored in cold water. They should neither be left to dry out, nor should be cleaned and stored in hot water as the dentures may warp and therefore become ill fitting. If dentures do not fit properly, this affects speech, mastication and can lead to discomfort and pain.
Nutritional assessment
Health-care professionals with appropriate skills and training should be involved in screening for malnutrition and risk of malnutrition. Holmes (2008, p. 48) states that ‘malnutrition means bad nutrition and can include deficiency, excess or imbalance of energy (calories), protein or other nutrients (vitamins and minerals) that adversely affects body function and outcome’. Malnutrition can therefore include both under-nutrition and over-nutrition. The major concern for older people is under-nutrition, which has been described as that which falls below what is necessary to sustain life and well-being.
All hospital inpatients and outpatients at their first clinic appointment should be screened for nutritional status. Screening should be incorporated into all nursing records for older people. This procedure should be repeated weekly for inpatients and where deemed necessary for outpatients. People in care homes should be screened on admission and again when there is clinical concern. Clinical concern is described as unintentional weight loss, fragile skin, poor wound healing, apathy, wasted muscles, poor appetite, altered taste sensation, impaired swallowing, altered bowel habit, loose fitting clothes or prolonged illness (NICE, 2006).
The following guidelines are recommended by NICE (2006) in relation to nutritional support. Interventions should be considered in people who are malnourished as defined by the following:
- A body mass index (BMI) of less than 18.5 kg/m2
- Recent unintentional weight loss greater than 10%
- BMI of less than 20 kg/m2 and recent unintentional weight loss greater than 5%.
They also state that nutritional support should be considered in people at risk of malnutrition including those who have eaten little or nothing for more than 5 days and/or people who have been identified as likely to eat little or nothing for 5 days or more. People with known poor absorptive capacity and/or high nutrient losses or those with increased nutritional needs from causes such as catabolism also require nutritional support.
Nutritional screening has been defined as a simple and rapid procedure that facilitates identification of nutritional risk (Green and Watson, 2005), whereas nutritional assessment is the determination of nutritional status using appropriate objective markers such as dietary intake, biochemical data, anthropometry and clinical condition (National Nursing Midwifery and Health Visiting Advisory Committee, 2002). Screening is the first step in nutritional assessment and should be incorporated into all nursing records for older people.
National Health Service Quality Improvement Scotland (NHSQIS, 2003) states that an assessment should include screening for malnutrition using a validated tool; however, they also state that clinical judgement may allow for the exclusion of some patients from the fuller screening.
Green and Watson (2005) carried out a detailed review of nutritional assessment and screening tools used by nurses. They found a wide range of tools available and in use and concluded that there needs to be greater emphasis upon the reliability and validity of these tools. They also state that adopting the use of screening tools such as the one produced by the British Association of Parenteral and Enteral Nutrition (BAPEN) may help standardise the approach to nutritional screening – Malnutrition Universal Screening Tool (MUST).
Bowling (2004, p. 13) defines nutritional screening as a means of ‘identifying patients who are malnourished or at risk of becoming undernourished’. The MUST was produced by BAPEN as means of identifying patients who are at risk of becoming malnourished whether they are underweight or obese. It is acknowledged that the tool is not designed to identify specific vitamin or mineral deviancies (BAPEN, 2003).
The tool consists of a five-step approach which culminates in a score that estimates the patient’s risk and can be viewed at the following web address: http://www.bapen.org.uk/musttoolkit.xhtml.
The score is related to recommended actions although Bowling (2004) adds that this will need to be supported by a care plan. Brown et al. (2006) state that MUST has a fair/ good to excellent inter rater reliability and is quick to complete. Steps in calculating MUST score:
- Measure height and weight to get a BMI score
- Note the percentage of unplanned weight loss and score
- Establish acute disease effect and score
- Add scores from steps 1, 2 and 3 together to obtain overall risk of malnutrition
- Use management guidelines and/or local policy to develop care plan
Score of 0 = low risk
- Screening repeated weekly in hospital, monthly in care homes, annually in community
Score of 1 = medium risk
- Document dietary intake for 3 days
- If no improvement, follow local policy for clinical concern
- Repeat screening as before
Score of 2 or above = high risk
- Referral to dietician, nutritional support team or implementation of other local policy
- Patient’s nutritional intake should be increased
- Care plan should be monitored and reviewed weekly in hospital, monthly in care homes and community.
Although the BMI is widely accepted as the Gold Standard indicator of malnutrition, its use may mask important weight changes in all patients which can result in a nutritional problem being overlooked. BMI may also be unreliable in the presence of conditions including oedema and ascites. If used as a single screening tool in such patients, unintentional weight loss may be missed. Furthermore, in older adults, reliable measurement of height can be difficult due to vertebral decompression, loss of muscle tone and postural changes (Harris and Haboubi, 2005).
However, the BMI omits to acknowledge the significance of age and metabolism which decreases with age. This is associated with a decrease in lean body mass which results in a reduction in calories required to maintain this mass. The outcome is a decrease in nutritional requirements for energy (Blechman and Gelb, 1999). Lean body mass declines by about 1% each year starting at the age of 55. This decline is a direct result of a reduction in overall activity. However, total body weight does not change as rapidly due to the increase in the proportion of body fat associated with ageing. However, if physical activity remains high, this reduction in lean body mass can be delayed.
As identified earlier, screening for malnutrition should be carried out on initial contact with health-care professionals and those identified at risk should be further assessed and evaluated using an appropriate and validated assessment tool. NHSQIS (2003) suggests that the following procedures should be followed in relation to Standard 2 (Assessment,
Screening and Care Planning) of their document Clinical Standards for Food, Fluid and Nutritional Care in Hospitals (2003).
When a person is admitted to hospital, an assessment is carried out. Screening for risk of under-nutrition is undertaken, both on admission and on an ongoing basis. A care plan is developed, implemented and evaluated.
(Standard 2 statement, p. 26)
Essential criteria associated with the Standard 2 statement (NHSQIS, 2003):
When a person is admitted to hospital as an inpatient, the following are identified and recorded within 1 day as part of the medical/nursing assessment:
- Height and weight
- Eating and drinking likes/dislikes
- Cultural/ethnic/religious requirements
- Social/environmental mealtime requirements
- Physical difficulties with eating and drinking
- The need for equipment to help with eating and drinking.
The initial assessment includes screening for risk of under-nutrition. This screening is carried out using a validated tool appropriate to the patient population and which includes criteria and scores that indicate action to be taken.
Repeat screenings are undertaken in accordance with clinical need and at a frequency determined by the outcome of the initial and subsequent screenings. The outcome of the screening is recorded in the medical notes.
The assessment process identifies the need for referral to specialist services, for example dietetic, dental.
Patients have access to specialist services within agreed timescale and access should be available 7 days a week for urgent cases.
When a person is admitted to hospital, an assessment is carried out. Screening for risk of under-nutrition is taken, both on admission and on an ongoing basis. A care plan is developed, implemented and evaluated.
The multidisciplinary care plan is followed, reviewed and refined, and includes:
- Outcomes of the initial assessment
- Outcomes of the screening for risk of under-nutrition
- Frequency/dates for repeat screening
- Actions taken as a consequence of repeat screening.
The discharge plan is developed with the patient and, where appropriate, carers, and includes information about:
- The patient’s nutritional status
- Special dietary requirements
- The arrangements made for any follow-up required on nutritional issues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




