Double Bundle Posterior Cruciate Ligament Reconstruction
Christopher A. Kurtz MD
Jon K. Sekiya MD
Chad T. Zehms MD
Christopher D. Harner MD
History of the Technique
Reconstruction of the posterior cruciate ligament (PCL) has gained ever-increasing attention in the medical literature. This growing appreciation of the PCL, especially in conjuncture with a multiligamentous knee injury, has led to significant refinements in PCL reconstruction techniques. However, despite these important advancements, treatment of the PCL deficient knee remains a difficult challenge. Numerous controversies still exist regarding the optimal management of PCL injuries, including surgical versus conservative treatment, acute versus chronic reconstruction, transtibial tunnel versus tibial inlay fixation, allograft versus autograft tissue for reconstruction, and single versus double-bundle techniques. This chapter will discuss some of the more recent advances in double bundle techniques as well as the authors’ preferred methods.
Efforts to develop a double bundle PCL reconstruction evolved initially from basic science anatomical dissections. Traditionally, the PCL has been divided into two predominate bundles: anterolateral (AL) and posteromedial (PM). Anatomical dissections1,2 have shown that the larger and stronger anterolateral bundle is primarily taut in flexion and the smaller posteromedial bundle is primarily taut in extension. In actuality, the PCL is significantly more complicated with multiple bands all functioning to some extent throughout the range of knee motion3,4,5,6; however, the two-bundle concept is a useful distillation of complex anatomy into workable units and is the cornerstone of all double bundle techniques.
In addition to anatomic studies, biomechanical evaluations of the PCL further advanced the argument for a double bundle approach to reconstruction. Because of its larger size and strength, the anterolateral bundle is usually recreated in single bundle reconstruction techniques. Further investigation and biomechanical analysis revealed that the single bundle reconstructions did not fully restore native mechanics in all ranges of motion.6,7,8 These studies have shown that the anterolateral bundle reconstruction alone is unable to restore normal knee kinematics especially with higher degrees of flexion. This has also been observed clinically in the authors’ experience with single bundle PCL reconstructions for isolated grade-III injuries.9
Many believe that the addition of the posteromedial bundle to the reconstruction is the key to re-creating normal posterior restraint as the knee is flexed beyond 90 degrees.7,8 This phenomenon is likely due to the relatively vertical orientation of the anterolateral bundle at higher degrees of knee flexion, which decreases its ability to resist posterior translation while concomitantly the posteromedial bundle assumes a more mechanically advantageous horizontal alignment.6
The natural progression was to the double bundle technique, re-creating both the AL and PM bundles of the PCL. Today, much of the PCL literature focuses on double bundle reconstructions using various allografts and graft placement techniques. These include the tibial tunnel and tibial inlay techniques using Achilles, hamstring, quadriceps tendon, tibialis anterior, and bifid patellar tendon allografts.
Indications and Contraindications
Classification of PCL injuries can serve as a useful guide in their management. Partial or grades I and II tears have different outcomes and treatment algorithms than full thickness or grade-III injuries. PCL injuries may be further classified as isolated or as part of a multiligamentous knee injury. In addition, these injuries can be broken down by
time from injury into acute or chronic tears.10 The appropriate avenue of treatment will stem from classifying the injury along with a careful evaluation of patient-specific considerations.
time from injury into acute or chronic tears.10 The appropriate avenue of treatment will stem from classifying the injury along with a careful evaluation of patient-specific considerations.
Agreed upon indications for PCL reconstruction presently include isolated grade-III PCL injuries as well as a PCL tear as part of a multiligamentous knee injury. In the acute setting, grade-III injuries or multiligamentous injuries are best approached within the first few weeks from injury.10,11 Patients with symptomatic chronic grade-III PCL injuries are also candidates for surgical reconstruction. In the chronic setting it is critical to assess for associated limb malalignment as well as associated posterolateral corner insufficiency.12,13 If these additional deformities are present, they should then be addressed at the same setting or as a staged procedure as primary reconstruction of the chronic PCL tear without attention to an associated limb alignment or concomitant posterolateral corner insufficiency may lead to graft failure.
Contraindications to reconstruction are also important to consider. All grade-I and the majority of grade-II PCL injuries lend themselves to nonoperative treatment, particularly in the non–high-end athlete.14,15,16 The exception for grade-II injuries would be those mentioned previously in multiligamentously injured knees or in the symptomatic elite athletes. Abnormal limb alignment, mechanical axis abnormalities, and visual gait disturbances should be addressed in a staged fashion or concomitantly with the planned surgical procedure. Any and all abnormalities found on examination must be corrected prior to or in concert with reconstruction of the PCL. Meticulous attention to detail with regard to these associated injuries is critical to a successful outcome with the surgical management of this complex injury.
Surgical Techniques
Achilles-Hamstring Reconstruction
Prior to beginning the case and opening of any grafts, a full and complete examination under anesthesia is performed to confirm a grade-III PCL injury as well as to evaluate for any associated injuries. Some studies have demonstrated that a grade-III PCL injury is unlikely to be found in isolation.17,18 The operation is performed with the patient in a supine position and the use of a tourniquet is optional. A sandbag and lateral post aid in maintaining a flexed knee position when needed throughout the case. A standard diagnostic arthroscopy is performed and any chondral or meniscal injuries are addressed. The damaged PCL is debrided, leaving a footprint at its insertion sites on the femur and tibia. An accessory posteromedial portal and a 70-degree arthroscope aid in the visualization of the tibial insertion site. Care is taken to avoid damage to the meniscofemoral ligaments of Humphrey and Wrisberg when present.
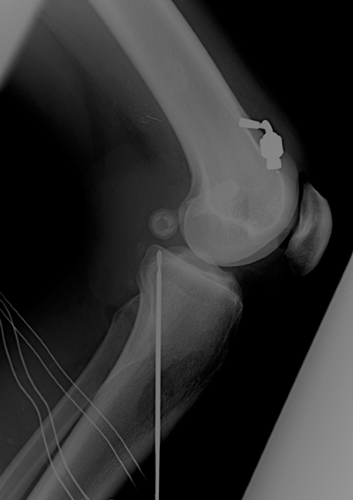
With the knee in 90 degrees of flexion, a PCL drill guide set at 60 degrees is placed at the junction of the middle and distal thirds of the tibial footprint, erring slightly lateral. The guide pin is then drilled from the anteromedial tibial through the prepositioned guide. An intraoperative lateral radiograph or C-arm is used to confirm acceptable guide-pin placement (Fig. 46-1). The tibial tunnel is then drilled to a diameter of 11 mm followed by an 11-mm tunnel dilator. The superior aspect of the intra-articular portion of the tibial tunnel is chamfered smooth with a rasp. Attention is then turned to the femoral tunnels. At a point approximately 6 mm from the articular surface, within the femoral footprint of the AL bundle, a Beath pin is placed through the anterolateral arthroscopic portal at the 1 o’clock position in a right knee (11 o’clock in a left knee) exiting out the anteromedial femur. The femoral tunnel is drilled to an 11-mm diameter and a depth of 30 mm. The PM femoral tunnel is prepared in a similar fashion. At a point approximately 5 to 6 mm from the articular surface within the footprint of the PM bundle, a second Beath pin is placed again through the anterolateral arthroscopic portal at the 2:30 position of a right knee (9:30 in a left knee) (Fig. 46-2). In order to avoid breakthrough between the two tunnels, the PM pin should diverge from the AL pin and be centered at least 4 to 5 mm from the AL tunnel edge. The PM tunnel is drilled to a depth of 30 mm with a diameter of 6 to 7 mm depending on
the doubled hamstring graft size. The Beath pins may be left in place for future graft passage or exchanged for a looped shuttle suture.
the doubled hamstring graft size. The Beath pins may be left in place for future graft passage or exchanged for a looped shuttle suture.
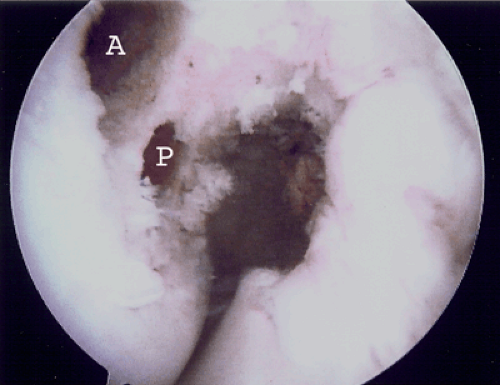 Fig. 46-2. Arthroscopic view of the two femoral tunnels in a left knee. A, anterolateral; P, posteromedial. |
Graft preparation occurs at the back table while the tunnels are created. An Achilles allograft is used for the AL bundle and a doubled autologous hamstring (either semitendinosus or gracilis) is used for the PM bundle. The Achilles is prepared with an 11 mm by 25 to 30 mm bone block. The tendinous end is whipstitched with nonabsorbable braided no. 5 Ethibond (Ethicon, Summerville, N.J.) or no. 2 Fiberwire (Arthrex, Naples, Fla.). The hamstring is harvested in the standard fashion through the anteromedial incision. The harvested hamstring is then doubled over a closed-looped EndoButton (Smith & Nephew, Andover, Mass.) and whipstitched on each end with no. 2 Fiberwire (Arthrex, Naples, Fla.).
Each graft is then sequentially passed in the same fashion. An 18-gauge wire loop is placed up the tibial tunnel, through the knee, and out the anterolateral portal. The sutured ends of the grafts are passed back through the knee and seated into the tibial tunnel via the looped 18-gauge wire. Femoral tunnel passage is accomplished with either the prepositioned Beath pins or by the shuttle sutures. The Achilles bone plug is then delivered into the knee via the anterolateral portal and seated into the AL femoral tunnel with the cancellous side facing posterior. The looped end of the hamstring graft is likewise passed and seated into the AM femoral tunnel (Fig. 46-3). The Achilles bone block is secured with a 7 by 20 mm metal interference placed over a guidewire through the anterolateral portal. Care is taken to fix the bone plug of the AL graft on the posterior surface, which fixes the graft to the perimeter of the femoral cortex. This allows for maximal length and mimics normal anatomy more precisely. The hamstring is fixed on the femur by flipping the EndoButton on the anteromedial outer femoral cortex or alternatively, the hamstring may be secured with an absorbable biointerference screw. The grafts are tensioned and the knee is brought through several cycles of flexion and extension. With the knee held at 90 degrees of flexion, tension applied to the graft, and application of an anterior drawer, the Achilles (AL bundle) allograft is fixed to the tibia with a soft-tissue screw and washer. The hamstring (PM bundle) autograft is fixed with a separate soft-tissue screw and washer with the knee held at 15 degrees of flexion, tension on the graft, and application of an anterior drawer (Fig. 46-4A,B). The knee is then examined for stability and full range of motion and any required retensioning is performed by adjusting the tibial fixation. Once stability is restored, then the tibial fixation is augmented with a biointerference screw placed up the tibial tunnel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree