CHAPTER 22 Double-Bundle Anterior Cruciate Ligament Reconstruction
Successful clinical results following single-bundle anterior cruciate ligament (ACL) reconstruction have been reported in 70% to 90% of cases.1,2 Historically, single-bundle ACL reconstruction techniques have been the standard treatment of choice for the ACL-deficient knee. As more and more patients have been helped through advanced surgical techniques and rehabilitation protocols, the expectations of future patients have risen. Today, almost all patients who suffer an acute ACL injury expect to return to full, unlimited sports activity in a rapid fashion. However, residual rotational instability has been reported in approximately 20% of cases after conventional single-bundle reconstruction.3 A recent biomechanical study has shown that single-bundle ACL reconstruction can successfully control anterior tibial translation but could not control a combined rotatory load of internal rotation and valgus torque.4 Similarly, in vivo kinematic studies have shown that ACL reconstruction can restore anteroposterior stability. However, the tibia remains externally rotated relative to the femur during normal kinematics of running.5 The concept of anatomic ACL reconstruction is predicated on a desire to restore native anatomy more closely and in turn, normal kinematics of the knee.
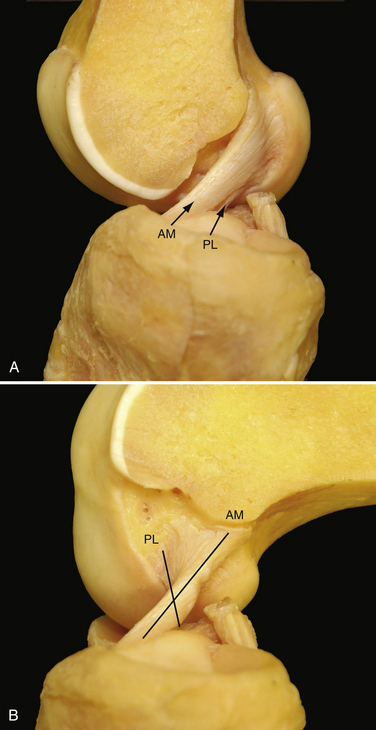
Multiple anatomic studies have used various methods to demonstrate that the ACL is composed of two distinct functional bundles; the anteromedial (AM) and posterolateral (PL) bundles (Fig. 22-1).6–8 Biomechanical studies have demonstrated that in situ forces, in response to an anterior tibial and combined rotatory load, are greatest in the PL bundle near full extension and at 60 degrees flexion in the AM bundle, respectively. Studies have also shown that reconstruction of either of the individual bundles alone cannot reproduce the mechanical properties of the native intact ACL.9,10 Yagi and colleagues11 have measured the in situ forces in response to an anterior tibial load and a combined rotatory load of internal rotation and valgus torque using a robotic universal force moment sensor testing system. When compared with single-bundle ACL reconstruction, the in situ forces in double-bundle reconstructed knees more closely approximated those of the native ACL.
ANATOMY
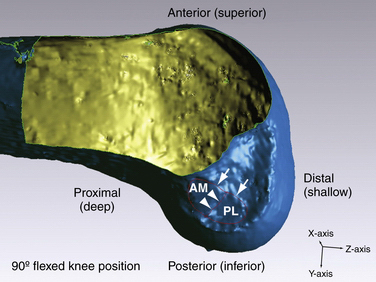
The ACL courses from the medial aspect of the lateral femoral condyle (femoral insertion site) to a position on the tibia between the medial and lateral tibial spines (tibial insertion site). For the sake of consistency, this chapter refers to positional relationships with the knee located in the anatomic position or full knee extension. It is important to realize that arthroscopic evaluation of the ACL typically occurs with the knee flexed to 90 degrees. For this reason, the anatomically anterior border of the ACL will appear arthroscopically as the superior border. Similarly, the anatomically posterior extent of the ACL will appear as the arthroscopic inferior border when the knee is flexed to 90 degrees (Fig. 22-2). The femoral insertion site or ACL origin is located at the anatomically posterior aspect of the lateral surface of the femoral intercondylar notch. The length of the femoral footprint of the ACL is 17.7 ± 1.2 mm and the width is 9.9 ± 0.8 mm. The femoral attachment of the AM bundle forms an angle with the PL bundle of 27.6 ± 8.8 degrees.12 The average length of the femoral AM bundle is 9.8 ± 0.8 mm, and the average length of the femoral PL bundle is 7.3 ± 0.5 mm. The anatomically anterior (arthroscopically superior) border of the femoral insertion of the ACL is defined by an important bony landmark13 referred to as the lateral intercondylar ridge (see Fig. 22-2). In a surgical observational study, no ACL fibers could be seen attaching anterior to the ridge. The lateral bifurcate ridge, another important osseous landmark, delineates the AM and PL insertion areas. Ferretti and associates12 arthroscopically visualized the lateral bifurcate ridge in 49 of 60 patients undergoing ACL reconstruction. Of the 49 patients with a discernible lateral bifurcate ridge, 25 had a prominent ridge with a significant change of slope, whereas the other 24 had a relatively smaller but evident ridge.
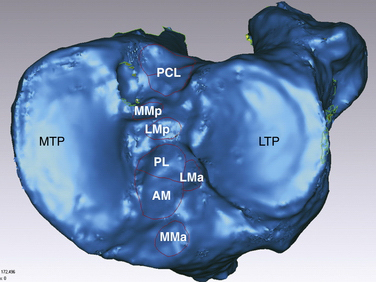
Anatomic ACL reconstruction is based on a comprehensive understanding of normal anatomy. It is important to realize that the course of the AM and PL bundles is distinct, with the bundles lining up in parallel near full extension and then crossing as the knee approaches 90 degrees of flexion (see Fig. 22-1).6,12,14–16 Specifically, the AM bundle originates at the anatomically posterior and proximal (arthroscopically inferior and deep) aspect of the lateral wall of the intercondylar notch. The PL bundle originates at the anatomically posterior and distal (arthroscopically inferior and shallow) aspect of the lateral wall of the notch (see Fig. 22-2). From the femoral origin, the fibers of the ACL course down to the tibial insertion site. In its midportion, the ACL tapers to a thinner diameter, similar to an hourglass shape. The cross-sectional area of the insertion sites are 3 to 3.5 times larger than the cross-sectional area of the ligament’s midsubstance.8,17 The ACL fibers fan out and insert on the center of the tibial plateau, between the two spines. It is for their relative insertion sites on the tibia that the two bundles of the ACL are named, with the AM tibial insertion site slightly anterior and medial to the PL bundle insertion site (Fig. 22-3.) The mean length of the tibial insertion has been reported in multiple studies7,18,19 to range from 14 mm (range, 9 to 18 mm) to 29.3 mm (range, 23 to 38 mm). The total area of the tibial insertion has also been reported with great variability, from 114 to 229 mm2. The area of the AM bundle insertion alone has been reported from 56 to 136 mm2 and the PL bundle from 52 to 93 mm2. The tremendous variability in reported size and area of the tibial insertion sites likely stems from the various methods used for taking measurements and the variable size of the cadaveric specimens used.20
Biomechanics
Recent biomechanical studies have more clearly defined the specific function of the two individual bundles of the ACL. Selective sectioning studies have shown that transection of the AM bundle increases anterior translation of tibia at 60 and 90 degrees of knee flexion. Conversely, transection of the PL bundle increases anterior translation of the tibia at 30 degrees of flexion. Following PL bundle transection, there was also increased rotation at 0 and 30 degrees in response to a combined rotatory load.21
In general, the concept of isometry in ACL reconstruction should be dismissed. The AM and PL bundles do not remain isometric throughout a full functional range of motion. Each bundle of native ACL is exposed to varying degrees of tension at various flexion angles.22 The AM bundle is slightly more isometric than the PL bundle, remaining taut throughout a greater arc of motion. In contrast, the PL bundle is taut with the knee in extension and is lax when the knee is flexed. Logically, the contribution of the PL bundle to knee stability becomes increasingly important under greater degrees of tension, or near full extension.9,10,23
Injury Mechanism and Rupture Pattern
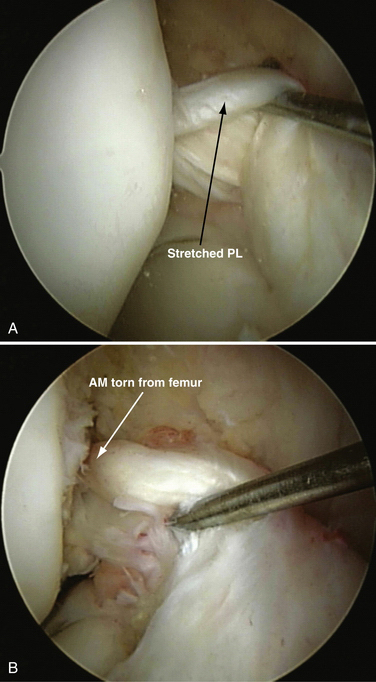
Understanding the mechanism of injury is an important first step in formulating an appropriate treatment strategy. Various injury mechanisms will place differential strains on the AM and PL bundles, thus producing various rupture patterns. Two distinct injury mechanisms of ACL have been classically described by Muller24: (1) hyperextension trauma, with resultant stretch of the ACL over the anterior intercondylar notch roof; and (2) moderate extension trauma, during which the AM bundle is taut and a valgus and/or external rotation force is applied. Based on the variable tension patterns exhibited different positions of knee flexion, we have seen a variety of two bundle injury patterns and isolated AM or isolated PL bundle injuries (Fig. 22-4). Isolated PL bundle injury occurs when stress is applied at or near full extension. In greater degrees of flexion (30 to 60 degrees), isolated AM bundle injury can occur.
In a prospective study, 121 consecutive patients were evaluated arthroscopically. with attention directed to determining the pattern of rupture.25 All patients were evaluated within 120 days of acute injury. There was complete rupture of the AM and PL bundles in 75% of patients. In the remaining 25% of patients, partial tear of the ACL could be seen. In 12% of total patients, no evidence of PL bundle injury could be seen. Therefore, we think that meticulous dissection of the remnant ACL is an important first step prior to proceeding with the reconstructive aspect of ACL surgery. Single-bundle augmentation is performed when appropriate, according to the specific injury pattern.26 Preservation of intact native tissue has distinct advantages, including preservation of the microvasculature and proprioceptive fibers. Isolated reconstruction of the AM or PL bundle alone requires an awareness of such injury patterns and more precise preoperative and intraoperative diagnostic assessment of the injury pattern.
PATIENT EVALUATION
History and Physical Examination
In cases of acute ACL injury, patients typically present with painful swelling, limp, and an obvious history of trauma. Common mechanisms include landing after jumping, a deceleration change in direction seen in pivoting sports (e.g., soccer, basketball, tennis), and direct blow forces on the lateral side of the knee producing valgus and external rotational force on the tibia. Some patients will report an audible pop or the sensation of tearing at the time of injury. A significant effusion typically occurs within a few hours of injury. A flexed posture of the knee joint can be seen caused by the large hemarthrosis, but should also raise concern for the possibility of mechanical obstruction from the remnant ACL or a bucket handle tear of the meniscus. In patients with a history of trauma followed by hemarthrosis, the most common arthroscopic finding is ACL injury (45% in a study of 320 patients).27
A manual assessment of knee laxity includes several tests—the Lachman, anterior drawer, and pivot shift tests. The Lachman test is considered to be the most reliable test for assessment of ACL injury.28 However, false-negative findings can be seen in acute cases when significant hamstring spasm and guarding are present. To avoid a high false-negative rate, effort should be made to have the patient as relaxed as possible. The Lachman test is performed at 20 to 30 degrees of knee flexion. One hand of the examiner stabilizes the femur and the other hand applies an anteriorly directed force to the proximal tibia. The degree of translation and the quality or firmness of the end point should be noted. Classification of anteroposterior translation is categorized as grade I (3 to 5 mm), grade II (6 to 10 mm), or grade III (more than 10 mm).
The pivot shift test is highly specific for the diagnosis of ACL injury, but the sensitivity is low, particularly in the awake patient. Most patients may allow for a single shift to be performed, but will typically guard against allowing the knee to shift thereafter.28,29 The pivot shift maneuver mimics the giving way or buckling phenomenon that patients experience. A pivot shift test is performed with the patient supine and the hip in slight abduction as a valgus force is applied to the extended knee. In the ACL-deficient knee, the tibia rests in an internally rotated and anteriorly subluxated position. As the knee is flexed to 20 degrees, the tibia reduces, suddenly resulting in the pivot shift. The degree of shift is graded as grade I or pivot glide, grade II or distinct shift, and grade III or transiently locked out. This test can be difficult to perform in the awake patient but is highly sensitive and specific during the examination under anesthesia.30
Diagnostic Imaging
In most cases of acute ACL injury, plain radiographs will be negative. Still, radiographs are necessary to rule out combined ligamentous injury, secondary arthritic changes, or physeal injury in the skeletally immature patient. The Segond fracture, or lateral tibial rim avulsion of the meniscotibial ligament, is considered pathognomonic for ACL injury. This lateral capsular avulsion is produced by the stress of knee flexion and internal tibial rotation commonly seen as a mechanism of ACL injury.31
Magnetic resonance imaging (MRI) is highly sensitive and specific for the diagnosis of acute ACL tear.32 However, it is often far more difficult to differentiate partial tears from complete tears or to detect isolated single-bundle tear patterns. There is great variability in clinically available MRI magnets. High-resolution MRI with dedicated ACL sequences greatly increases the sensitivity of MRI. Standard MRI protocols consist of sagittal, coronal, and axial T1- and T2-weighted images (Fig. 22-5). The issue with such sequences is that the ACL does not course through the knee in a perfectly coronal or sagittal plane. Therefore, to improve sensitivity, we use modified oblique coronal and oblique sagittal imaging sequences. When the beam is oriented parallel to the fibers of the ACL, greater detail is appreciated and the AM and PL bundles can be evaluated independently. (Figs. 22-6 and 22-7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree