Dorsal Plating
Charles Day
Orrin Franko
Indications/Contraindications
Past studies have demonstrated that dorsal plating of distal radius fractures can effectively stabilize dorsally angulated intra- or extraarticular fractures, dorsal shearing factures, die-punch lunate facet fractures, and dorsal radiocarpal fracture-dislocations (1,2,3,4). These fracture patterns can be effectively treated whether they are low- or high-energy injuries.
Relative contraindications include volarly displaced fractures, which may benefit from a volar plate, as well as comminuted articular distal radius fractures, which will not allow for screw fixation distally and may be better addressed using an external fixator. A volar comminuted fragment may be better addressed using a volar plate, as well (5).
Preoperative Preparation
Surgical preparation requires sterilization and draping in the usual fashion. Preoperative antibiotics are given to help prevent wound infection. An axial block with monitored anesthesia care (MAC) can be used for anesthesia.
Technique
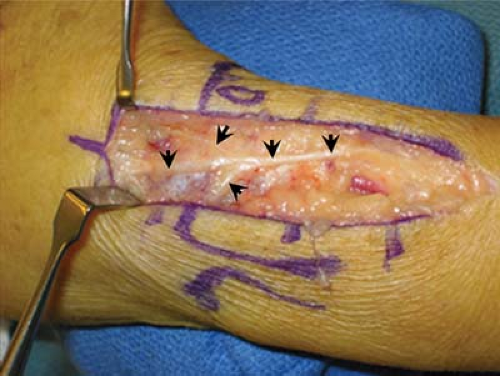
The surgical procedure begins with a 7- to 12-cm dorsal incision just ulnar to Lister’s tubercle (Fig. 6-1).
Take care to identify and avoid the superficial branch of the radial nerve (Fig. 6-2).
Expose the extensor retinaculum, incise it over the third dorsal extensor compartment, and retract the extensor pollicis longus (EPL) tendon radially (see arrow, Fig. 6-3).
Expose the distal radius and the proximal row of the carpus via sharp dissection of the periosteum and dorsal wrist capsule between the second and fourth dorsal extensor compartments (Fig. 6-3). Take care to avoid injury to the underlying scapholunate ligaments during the capsular dissection.
Once the articular surface and fracture are visualized, remove any hematoma or fibrous union at the metaphyseal fracture site.
Remove Lister’s tubercle, and then reduce the fracture. Reduction of the dorsal angulation is best achieved by stabilizing the hand while placing bone retractors (Hohmann retractors) underneath the proximal fragment and lifted to reduce the fracture angulation (Fig. 6-4).
A 0.045 K-wire can be used to hold the reduction while fluoroscopy is used to visualize its positioning and alignment (Fig. 6-5A, B).
Once satisfactory reduction is achieved, place the plate directly over the dorsum of the radius and then stabilize it with a single screw in the oval-shaped sliding hole of the plate stem (Fig. 6-6). Prior to stabilization, the plate can be appropriately bent to accommodate the curvature of the distal radius.

Figure 6-1 The initial incision can be 7 to 12 cm long along the dorsal aspect of the wrist, just ulnar to Lister’s tubercle (arrow). The radius (R) and ulna (U) have been outlined here.
Use fluoroscopy to confirm placement of the plate with respect to the bone (Fig. 6-7A, B).
Rotation of the plate around the single screw can still be achieved at this point. If needed, visualize and reduce the articular fracture site, using a bone hook and clamp (Fig. 6-8).
Once placement has been verified with fluoroscopy, place three to five 2.7-mm screws across the metaphyseal holes of the plate (Fig. 6-9).
Check fixation and alignment once again with fluoroscopy, and place two more cortical screws. At least six cortices (two for each screw) are required for adequate stability of the plate (Fig. 6-10A, B).
For further stability, pack allograft bone chips into any metaphyseal defects.
Close the wrist capsule with a 3-0 Vicryl interrupted stitch.
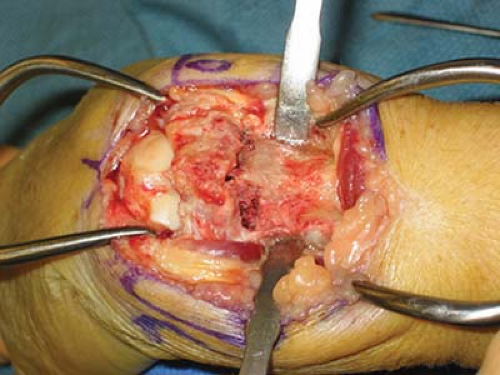
Figure 6-4 Reduction of the dorsal angulation is best achieved by stabilizing the hand while placing bone retractors underneath the proximal fragment and lifting to reduce the fracture angulation.

Figure 6-5 A 0.045 K wire can be used to hold the reduction while a fluoroscopy scan is used to visualize its positioning and alignment in both the anteroposterior (A) and lateral (B) views.
Repair the extensor retinaculum with nonabsorbable 3-0 polyester braided sutures, and leave the EPL dorsal to the extensor retinaculum to minimize tendon scarring. Despite the low-profile design of the plate, sometimes relaxing incisions are made on either side of the extensor retinacular flaps to ensure closure over the metaphyseal portion of the distal radius plate.
Close the subcutaneous layer, using 3-0 Monocryl, and close the skin, using a 4-0 Monocryl subcuticular stitch.
Pearls and Pitfalls
Care must be taken to ensure that no free-floating fragments exist along the volar cortex of dorsally angulated distal radius fractures (a volar plate may better address this fracture type).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree