Abstract
Introduction
In spatial neglect, the functional benefit of rehabilitation methods is subject to debate. A few studies have reported that galvanic vestibular stimulation (GVS) is efficacious in spatial neglect. The objective of the present study was to establish whether the effects of GVS persist after the end of stimulation.
Materials
Four patients with pathological rightward deviation in a bisection task at least three months after right hemisphere stroke. A single-blind, randomized crossover design was used to assess the effects of GVS on performance in line bisection and star cancellation tasks under three different conditions (cathode-right, cathode-left and sham stimulation).
Results
There were no significant differences in the performance of either task following GVS (relative to sham stimulation).
Conclusion
Galvanic vestibular stimulation did not reduce spatial neglect symptoms in any of the stimulation conditions. Further studies are necessary to understand the disparity between our results and those reported in the literature. Repeated sessions, a higher current intensity and/or alternating-current stimulation may improve this method before it can be used clinically.
Résumé
Introduction
L’intérêt fonctionnel des techniques de rééducation de la négligence spatiale unilatérale (NSU) est discuté. Quelques études rapportent un effet de la stimulation galvanique vestibulaire (SGV) pour traiter la NSU. Nous cherchons à déterminer si l’effet de la SGV persiste à l’arrêt des stimulations.
Patients et méthode
Cette étude inclus 4 patients à 3 mois minimum d’un AVC de l’hémisphère droit présentant une déviation pathologique sur l’épreuve de bissection de lignes de 20 cm. L’effet de la SGV et sa durée sont étudiés dans un schéma d’étude croisé dans différentes conditions (cathode à gauche, cathode à droite et simulée) et sur deux épreuves : bissection de lignes et barrage de cibles.
Résultats
Les résultats obtenus sous SGV, quel qu’en soit le sens (cathode à droite–anode à gauche ou inverse), ne sont pas différents de ceux obtenus sous condition simulée.
Conclusion
Nous ne retrouvons pas d’effet significatif de la SGV quel que soit le sens de stimulation. Des études supplémentaires sont nécessaires pour comprendre les divergences avec les résultats déjà décrits. Les effets de séances de répétées, d’une SGV de plus forte intensité ou d’un courant alternatif pourraient améliorer cette technique avant d’envisager son utilisation en rééducation.
1
English version
1.1
Introduction
Unilateral spatial neglect (USN) syndrome is conventionally defined as an inability to detect, move towards, or respond to significant stimuli delivered contralaterally to a brain lesion and that cannot be attributed to sensorimotor impairment . Unilateral spatial neglect occurs in 25 to 30% of stroke victims and is predictive of a poor functional outcome . Furthermore, USN appears to have a negative impact on post-stroke quality of life . Relief of the symptoms of USN is thus a major challenge on both individual and societal levels.
In 2006, Luaute et al.’s literature review identified 18 different rehabilitational approaches for left USN. The techniques’ respective degrees of efficacy are subject to debate . A temporary decrease in USN symptoms has been described following the application of different types of sensory stimulation . Caloric vestibular stimulation (CVS) consists in activation of the vestibular system via the instillation of warm or cold water into the external auditory meatus. This technique is associated with a reduction in neglect symptoms such as tactile neglect , representational disorders , somatoparaphrenia and related symptoms such as anosognosia and hemiplegia . Nevertheless, the use of CVS in rehabilitation is limited by practical aspects and its frequent side effects (nystagmus, nauseas and dizziness) .
Galvanic vestibular stimulation (GVS) consists in the activation of the vestibular system by application of direct current to the skin over the mastoids. In contrast to CVS, GVS is associated with very few adverse effects; several studies of small numbers of patients have suggested that GVS might be a valuable way of reducing the symptoms of USN . Moreover, the ability to perform sham stimulation (analogous to a placebo ) enables statistical analysis of the GVS’s effects. The fact that GVS is simpler and less costly to implement than transcranial magnetic stimulation and CVS means that its use in rehabilitation can be envisaged. A decrease in visuospatial neglect during GVS and a lasting reduction in tactile extinction after GVS (even some time after stroke) have already been demonstrated. Left-cathodal GVS led to a decrease in deviation of the subjective vertical in patients with right hemisphere damage . Left arm position sense (which can be altered by right-cathodal GVS in right-handed healthy subjects ) was improved by left-cathodal GVS in patients with left USN . Line bisection is deviated leftwards by right-cathodal GVS in right-handed healthy subjects . Case studies have described a reduction in prosopagnosia and improvements in figure-copying during GVS . Galvanic vestibular stimulation is cheap, easy to implement and can be applied to most patients (even soon after stroke). Improved left-side visual exploration during left-cathodal GVS has already been described in patients suffering from USN. The objective of the present study was to determine whether the improvement in the leftwards visual exploration persisted after the end of GVS. This duration will influence the value and efficacy of this type of treatment and the way the technique can be implemented as part of a rehabilitation programme.
1.2
Patients and methods
In the present interventional, prospective, single-blind, crossover feasibility study, each patient was treated with three different GVS modes. Patients were recruited from the neurological rehabilitation clinics at Raymond Poincaré University Hospital (Garches, France) and Aunay sur Odon General Hospital (Aunay sur Odon, France). The main inclusion criteria were the occurrence of a first right ischemic or hemorrhagic stroke more than 3 months previously (to diminish the effects of spontaneous recovery), and a 20 cm line bisection test result suggestive of left USN (i.e. a rightwards deviation of more than 6.5 mm). The exclusion criteria included the standard contra-indications to GVS (epilepsy, the presence of a pacemaker or intracranial ferromagnetic material, and skin damage over the mastoids), participation in another USN trial, corrected visual acuity that prevented close-up reading, vestibular damage and pre-existing neurological disease. Table 1 summarizes the characteristics of the study patients. The Catherine Bergego scale was used to assess USN behaviour in everyday life and it ranges from 0 (least severe) to 30 (most severe) . All patients displayed homonymous hemianopsia and left proportional hemiplegia. Only one patient (KJ) had resumed walking, with the aid of a crutch.
| Patient | Gender | Age (years) | Handedness | Educational level/profession | Lesion sites | Time since stroke (months) | CBS score | Stimulation order |
|---|---|---|---|---|---|---|---|---|
| BP | M | 61 | Right-handed | University degree/nurse | Temporo-insular, deep frontal | 3.5 | 22 | RC-sham-LC |
| KJ | M | 38 | Right-handed | Left school at 12/cook | Frontoparietal, thalamic, CGN | 12 | 20 | Sham-RC-LC |
| CB | M | 66 | Right-handed | Left school at 16/company director | Frontoparietal, CGN | 3 | 16.25 | RC-LC-sham |
| FG | M | 69 | Right-handed | University degree/decorator | Frontoparietal | 3 | 22 | LC-sham-RC |
For each GVS condition, tests were performed before, during, immediately after and ten minutes after stimulation. The primary efficacy criterion was the deviation in the line bisection task (length: 20 cm; width: 1 mm) taken from the batterie d’évaluation de la négligence (BEN) battery . Each line was presented on an A4 sheet placed horizontally in front of the patient. The patient had to mark the centre of the line with a pencil mark. The deviation (in mm) relative to the centre of the line was measured. By convention, rightward and leftward deviations were given positive and negative values, respectively. The baseline was measured for an average of 8 bisections (range: 5–9). On average, 4 bisections (range: 3–5) were performed at each measurement time point before, during and after GVS. The patients also performed the star cancellation test from the Behavioural Inattention Test (BIT) battery . The efficacy criterion was the total number of small stars cancelled. In the star cancellation test, three omissions suggest the presence of an attentional disorder. This test was performed once before, during and after GVS. The order in which the various stimulation conditions were administered is given in Table 1 .
Galvanic vestibular stimulation was applied with a regulated, direct-current device (Galvadyn, Electronic Conseil, Gallargues Le Montueux, France) with a maximum output current of 20 mA and a maximum output voltage of 30 V. The carbon electrodes (4 cm × 6 cm) were covered with a saline-soaked sponge held in place over the mastoids with a strap. Each patient was exposed to three different stimulation conditions: cathode-left anode-right, cathode-right anode-left, and sham stimulation. The time interval between the stimulations was always greater than 48 h, so that the results were not perturbed by a post-effect of previous stimulation. The patients were not informed about the type of stimulation delivered at each session. During stimulation, the current intensity was increased manually by 0.1 mA per second until a value of 1.5 mA was reached. During increases and decreases in current intensity, GVS can induce a slight itching sensation. Hence, during sham stimulation, the current was increased in the same way and then turned off after a few seconds. Sham stimulations were performed with the cathode on the left mastoid and the anode on the right mastoid, making it impossible for the patient to distinguish between real and sham stimulations . In each condition, the stimulation lasted for 20 min. This duration was chosen in compliance with the safety guidelines on direct-current transcranial stimulation . The tests were performed after 10 minutes of stimulation. A preset alarm signalled the end of the stimulation period and the stimulator switched itself off automatically.
Statistical analyses of the data were performed with R software (version 2.14.1) . The Friedman test was used to compare the mean deviations recorded with each type of stimulation. The Friedman test is a non-parametric test that can compare k-paired samples corresponding to k therapeutic conditions for the same blocks, in order to detect a difference between conditions. For the cancellation test, the Friedman test was also used to compare the total number of cancelled stars.
In line with the tenets of the Declaration of Helsinki, all the patients gave their consent to participation in the study after have been informed of its procedures, its objectives and the risks associated with GVS.
1.3
Results
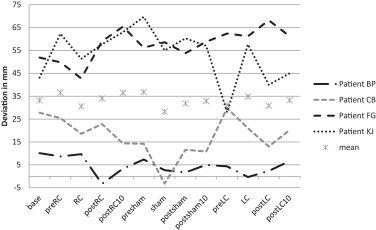
The scores in the 20 cm line bisection test are summarized in Fig. 1 for each patient and each condition. There were no significant differences between the three stimulation conditions ( P = 0.89 in the Friedman test).
The mean total number of cancelled stars is not shown for the tests performed 10 min after the right-cathodal GVS or 10 min after the sham condition because these measurements were not performed in all patients ( Fig. 2 ) and thus would not have been comparable with those recorded in the other conditions. None of the conditions was associated with a significant increase in the total number stars cancelled ( P = 0.58 in the Friedman test).
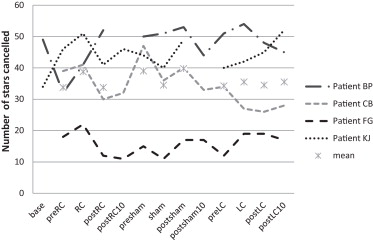
Patients FG and BP obtained better results in both tests during right-cathodal stimulation, as expected. At the end of each session, the patient was always asked to describe the sensations felt during the stimulation. Patient KJ reported a burning sensation under the right mastoid electrode in all stimulation modes, although it did not reach the pain threshold. Sham stimulation also produced this sensation, albeit less intensely. The patient had a scar from a decompressive craniectomy above the right mastoid and dysaesthesia in the retroauricular region. The other patients had not felt any pain but did sometimes report an itching sensation under the electrode. No skin lesions under the electrodes were observed.
1.4
Discussion
Galvanic vestibular stimulation did not significantly modify performance in the 20 cm line bisection test from the BEN and the star cancellation test from the BIT. These results do not confirm those of previous studies . Utz et al. used a variant of the Schenkenberg bisection test, featuring 17 lines for bisection on a sheet of paper. Only bisection of the lines situated furthest to the right on the sheet was significantly less deviated rightwards during GVS. The Schenkenberg test is perhaps more sensitive to variations in USN. Nevertheless, our results shown that GVS had no effect on the deviation in bisection of a single line placed in front of a patient suffering from left USN.
In the star cancellation test, GVS was associated with a significant difference in the total number of stars cancelled. In the study by Rorsman et al. , GVS increased the number of cancelled targets in the BIT’s line crossing and star cancellation tests. Nevertheless, this improvement was not constant and GVS did not have a positive effect on the two tests at the same time, despite the larger number of patients in the study. In the study by Rorsman et al., infraliminal stimulation was delivered at an intensity of 0.7 to 1.7 mA (median: 1.15) only during performance of the tests . In the present study, the stimulation method was exactly the same as that used by Utz et al. , and so does not explain the discordant results. In the absence of a significant effect, it is impossible to draw conclusions about the duration of this effect. In contrast, GVS is described in the literature as being simple to implement, cheap, and well tolerated. None of the patients complained about pain. The itching sensation felt under the electrode is a secondary effect that is frequently described in the literature.
Even though GVS is a relatively constraint-free technique, its efficacy is still subject to debate because our results contradict the literature data. Higher current intensities might have larger effects but might invalidate comparisons with sham stimulation. Increasing the number of stimulation sessions might conceivably constitute a way of increasing efficacy. However, a recent study showed that the improvement in performance in BIT tests was no greater after 10 sessions of GVS than after a single session . In the absence of a placebo condition, the latter study of a large number of patients does not enable one to draw conclusions as to the effect of GVS. If GVS does have an effect on the symptoms of USN, the mechanism of action is poorly understood. The right posterior parietal cortex is active during bisection tasks, and damage to this region often induces USN . During a bisection task in healthy subjects, functional MRI shows that GVS leads to greater activation of the ventral premotor cortex and posterior parietal cortex. Cortical activation in functional MRI experiments is greatest when direct-current GVS is turned on or turned off . It would be interesting to study the effect of alternating current GVS on USN. It appears that cathode-right stimulation is associated with greater effects in visual exploration tasks . The opposite configuration appears to have a greater effect on sensory extinction . The stimulation modes might have different effects, depending on the patient and the type of lesion.
The main limitation of the present study was the small number of patients. Moreover, only the patients were blinded to the type of stimulation applied. Use of the Schenkenberg Bisection Test would have enabled a more accurate comparison with the literature findings. To comply with safety rules, exposure to GVS did not exceed 20 minutes; this limited the number of tests that could be performed and the number of trials per test. Further research is required to better understand GVS’s mechanism of action and identify some effective stimulation modes.
1.5
Conclusion
Relative to a sham condition, GVS did not decrease the symptoms of USN in line bisection and star cancellation tasks. Additional studies are needed to understand the divergences with the literature results. The effects of repeated sessions, higher-intensity GVS and alternating-current GVS should be studied, with a view to improving this technique before its use in rehabilitation can be considered.
Disclosure of interest
The authors have not supplied their declaration of conflict of interest.
2
Version française
2.1
Introduction
Le syndrome de négligence spatiale unilatérale (NSU) est classiquement défini comme l’incapacité de détecter, s’orienter vers, ou répondre à des stimuli porteurs de signification situés du côté opposé à une lésion cérébrale et ne pouvant pas être attribuée à un déficit sensoriel ou moteur . La négligence spatiale unilatérale, qui survient dans dans 25 à 30 % des cas d’AVC , est un facteur de mauvais pronostic pour la récupération fonctionnelle . Elle semble avoir un impact négatif sur la qualité de vie ressentie après un AVC . La réduction des symptômes de NSU représente donc un enjeu majeur à l’échelle individuelle et collective.
Luauté et al. rapportent en 2006, dans une revue de la littérature , 18 différentes approches de rééducation de la NSU gauche. L’efficacité des techniques proposées est toujours discutée . Une diminution temporaire des symptômes de NSU a été décrite sous différents types de stimulations sensorielles . La stimulation calorique vestibulaire (SCV) consiste en l’activation du système vestibulaire par instillation d’eau chaude ou froide dans le conduit auditif externe. La SCV permet la réduction des symptômes de négligence tels que la négligence tactile , le trouble représentationnel , la somatoparaphrénie ou de symptômes associés comme l’anosognosie et l’hémiplégie . Néanmoins, l’utilisation de la SCV est limitée en rééducation par ses modalités de mise en œuvre et ses effets secondaires fréquents (nystagmus, nausées et vertiges) .
La stimulation galvanique vestibulaire (SGV) consiste en l’activation du système vestibulaire par application d’un courant continu sur la peau en regard des mastoïdes. Contrairement à la SCV, la SGV n’entraîne quasiment pas d’effet indésirable et pourrait être un moyen intéressant de réduire la NSU comme le suggèrent plusieurs études d’effectifs limités . De plus la possibilité d’effectuer une condition simulée, équivalent à un placebo , permet la mesure statistique des effets de cette stimulation. Elle est plus simple à mettre en œuvre et moins coûteuse que la stimulation magnétique transcrânienne et la SCV, ce qui permet d’envisager son utilisation en rééducation. Une diminution de la négligence visuo-spatiale a déjà été démontrée pendant les stimulations , ainsi qu’une amélioration de l’extinction tactile durable même à distance de l’AVC . La SGV cathodique gauche a permis une diminution de la déviation de la verticale subjective après lésion hémisphérique droite . Le sens de position du bras gauche qui peut être altéré par la SGV cathodique droite chez des droitiers sains est amélioré par la SGV cathodique gauche en cas de NSU gauche . La bissection de ligne est déviée vers la gauche sous SGV cathodique droite chez des droitiers sains . Une diminution de la prosopagnosie et des améliorations en copie de figures sous SGV ont été décrits dans des études de cas . Cette technique peu coûteuse, facile à mettre en œuvre, peut être proposée à la majorité des patients même rapidement après la survenue d’un AVC. Une amélioration de l’exploration visuelle à gauche a déjà été décrite pendant la SGV chez des patients souffrant de NSU. Cette étude cherche à déterminer si l’amélioration de l’exploration visuelle vers la gauche se maintient à l’arrêt de la SGV. Cette durée conditionne l’intérêt et l’efficacité d’une thérapie et permet d’adapter la façon dont cette technique peut être proposée dans un programme de rééducation.
2.2
Patients et méthode
Dans cette étude de faisabilité, interventionnelle, prospective, en simple insu et de type croisé, trois modes de SGV ont été réalisés pour chaque patient. Les patients ont été recrutés en rééducation neurologique à l’hôpital Raymond Poincaré de Garches et au centre hospitalier d’Aunay sur Odon. Les critères d’inclusion étaient la survenue d’un premier AVC droit ischémique ou hémorragique datant de 3 mois au minimum (pour diminuer les effets de la récupération spontanée), une bissection de ligne de 20 cm en faveur d’une NSU gauche (par exemple déviation de plus de 6,5 mm vers la droite). Les critères d’exclusion comprenaient les contre-indications à la SGV (épilepsie, matériel ferro-magnétique intracrânien, lésion cutanée en regard des mastoïdes, pacemaker ), la participation à un autre protocole sur la NSU, une acuité visuelle corrigée ne permettant pas la lecture de près, une lésion vestibulaire, une maladie neurologique préexistante. Le Tableau 1 résume les caractéristiques des patients inclus. La négligence spatiale en vie quotidienne a été évaluée par l’échelle de Catherine Bergego allant de 0 à 30 et sur laquelle le score augmente avec la sévérité de la négligence spatiale . Tous les patients présentaient une hémianopsie latérale homonyme et une hémiplégie gauche proportionnelle. Seul le patient KJ avait repris la marche, avec une canne anglaise.







