Distal Radio-Ulnar Joint Capsulectomy for Post-Traumatic Limitation of Forearm Rotation
William B. Kleinman
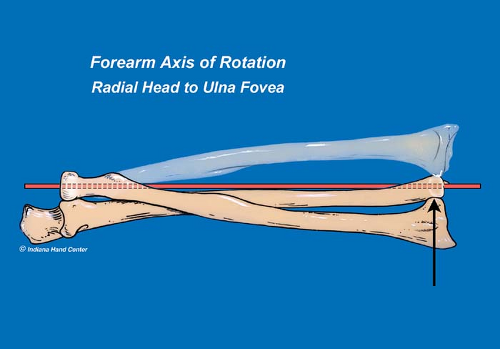
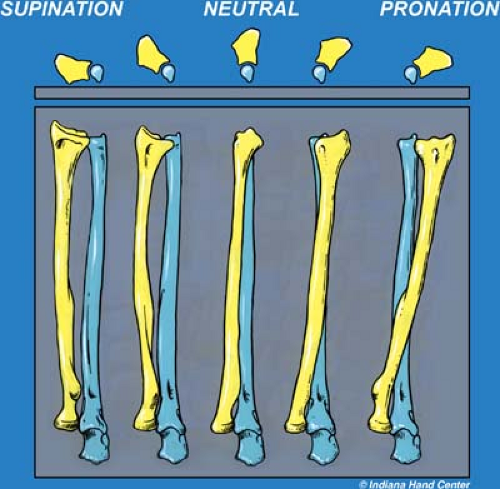
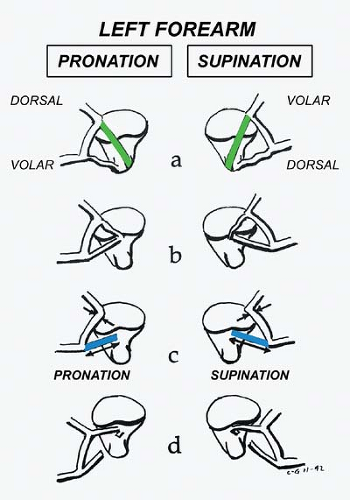
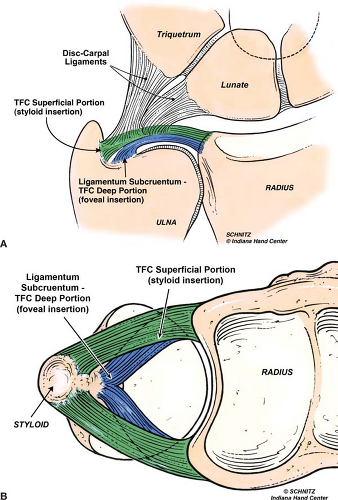
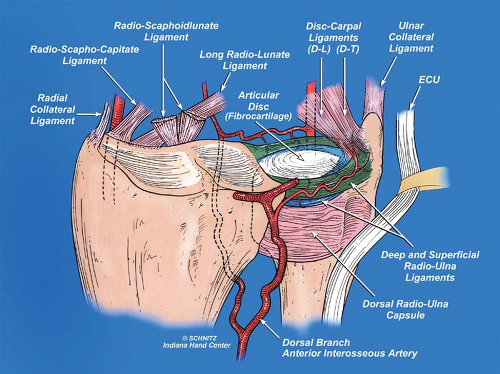
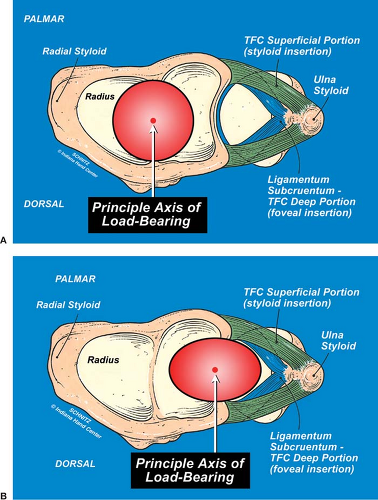
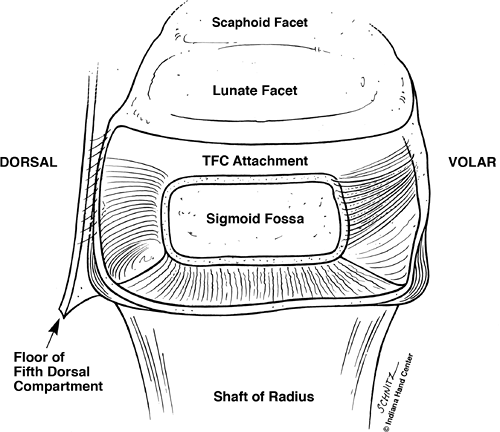
Reduced forearm pronosupination following trauma can have a profound, often devastating effect on upper extremity function. Of the four major joints of the upper extremity, the rotating forearm contributes most significantly to our ability to put or place our hand in space in order to maximize hand function (Fig. 36-1A, B). Forearm rotation is a complex activity that relies on integrated motion at the radiocapitellar and proximal radio-ulnar joints of the elbow, the mid-forearm interosseous ligament (IOL), and the distal radio-ulnar joint (DRUJ) at the wrist (Fig. 36-2). The longitudinal forearm axis-of-rotation passes through the center of the proximal radial head, along the forearm, exiting at the fovea of the distal ulna, at the base of the ulna styloid (Fig. 36-3). The ulnotrochlear joint of the elbow is a pure ginglymus (hinged) joint; it does not contribute at all to forearm rotation. Radius, carpus, and hand rotate as a unit around the longitudinal forearm axis-of-rotation from full supination, where the radius and the ulna are essentially parallel, to full pronation, where the radius–carpus–hand unit crosses the fixed ulna (Fig. 36-4). Normal biomechanics of full forearm pronosupination require not only rotation of the radius–carpus–hand unit around this longitudinal forearm axis-of-rotation, but translation of the sigmoid notch of the radius across the articular seat of the distal ulna. Figure 36-5 demonstrates the tracking line of the principal axis of load-bearing* through the full arc of pronosupination at the sigmoid notch (the distal cadaver ulna has been rotated out of the field for visibility of the notch). The obliquity of this load-bearing tracking line represents the relative shortening the radius undergoes as the radius–carpus–hand unit crosses the ulna from supination to pronation. Stability of the DRUJ through its normal 180-degree arc of forearm pronosupination is provided primarily by the complex check-rein components of the triangular fibrocartilage (TFC). The deep volar and dorsal components of the TFC (ligamentum subcruentum) (1) are principally responsible for stabilizing the radius–carpus–hand unit as it rotates and translates around the seat of the distal ulna (Fig. 36-6). The origin of the ligamentum subcruentum is at the fovea of the ulna; its two insertions are at the volar and dorsal aspect of the medial distal radius, distal to the sigmoid notch
(Fig. 36-7A, B). The well-vascularized superficial radio-ulnar ligaments of the TFC form a basket around the hypovascular central articular disc (Fig. 36-8).
(Fig. 36-7A, B). The well-vascularized superficial radio-ulnar ligaments of the TFC form a basket around the hypovascular central articular disc (Fig. 36-8).
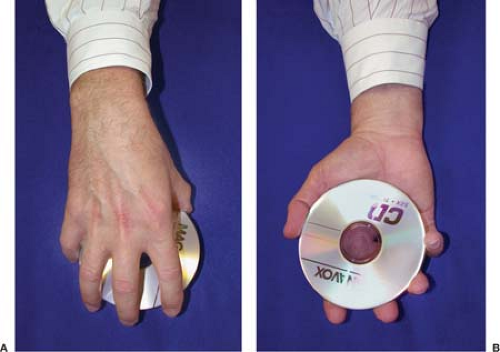 Figure 36-1 Rotation of the forearm is critical for putting or placing the hand in space for maximal function. |
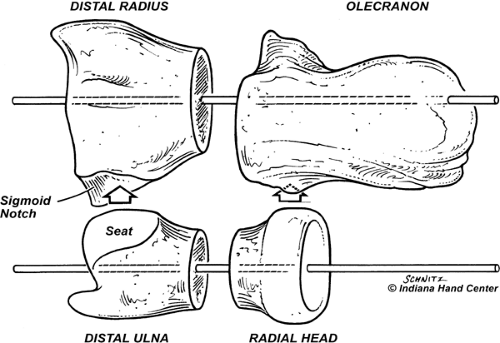 Figure 36-2 Forearm rotation takes place at two joints: (1) the distal radio-ulnar joint (DRUJ); and (2) the proximal radio-ulnar joint (PRUJ). Pronosupination can be conceptualized at both joints by thinking of the forearm as a bicondylar diarthrodial joint. Removing the long diaphyses of radius and ulna from the image places the DRUJ and PRUJ together as a flexing and extending glinglymuslike joint. |
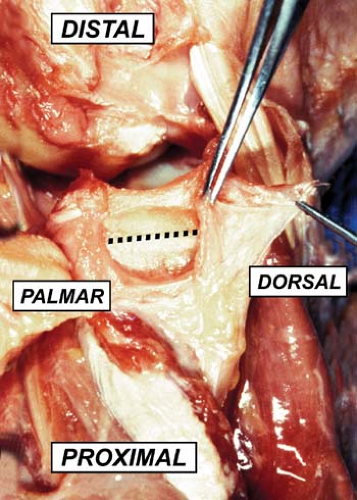 Figure 36-5 The principal axis of load-bearing tracks across the sigmoid notch from proximal/palmar in supination to distal/dorsal in pronation. |
The superficial radio-ulnar ligaments are relatively minor stabilizers of the DRUJ, because full pronation places the radius too volar relative to the entire ulna seat for the dorsal superficial radio-ulnar ligament to be mechanically effective as a DRUJ stabilizer. Conversely, full supination places the radius too far dorsal relative to the entire ulna seat for the volar superficial radio-ulnar ligaments to be effective (1,2) (Fig. 36-6). The articular disc (white; Fig. 36-8) is principally responsible for load transfer from the hand to the forearm through the ulnar side of the wrist, when the hand–forearm unit is ulnar deviated (Fig. 36-9A, B).
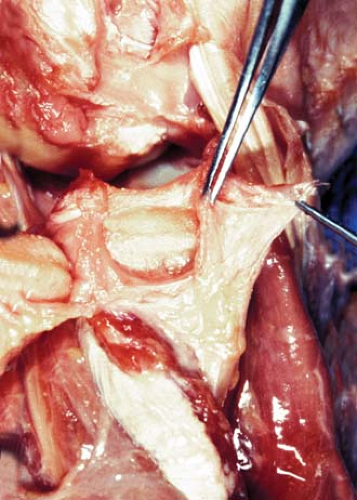
It is important to recognize that, although four extrinsic factors have been described as contributing to the stability of the DRUJ (extensor carpi ulnaris [ECU] tendon; ECU retinacular subsheath [VIth dorsal compartment], pronator quadratus [PQ] muscle, and interosseous ligament), the intrinsic components of the TFC bear the major responsibility for physiologic DRUJ stability (Figs. 36-6, 36-7 and 36-8). The entire DRUJ complex is biomechanically similar to any other diarthrodial joint in the human body. Two articular surfaces are joined for movement under load. Each opposing surface is covered by hyaline cartilage. The joint is surrounded 360 degrees by a capsule, the thickened parts of which form ligaments that guide motion between the two articular surfaces. The cartilage is nourished by synovial fluid. At the DRUJ, the TFC is the critical ligament complex guiding the radio-ulnar relationship through a physiologic arc of pronosupination. Vesely in 1967 gave the portion of the capsule other than the TFC the confusing name “volar and dorsal radio-ulnar ligaments,” implying that this remainder tissue represented some stabilizing component of the DRUJ capsule (3,4). More recently, details of the anatomy of the DRUJ capsule were investigated in our cadaver laboratory by my former hand surgery fellow, Dr. Thomas Graham, and me. Our findings were published in 1998, in the American Journal of Hand Surgery (3,5) (Figs. 36-10 and 36-11). Through our work in the lab, it became clear that, although the dorsal and volar DRUJ capsular components are anatomically distinct, neither of them plays a supportive role in DRUJ mechanics. Only the TFC and its various components are responsible for normal DRUJ stability.
Through a prospective clinical trial based on our newly acquired knowledge of the DRUJ capsule, we hypothesized that—as in all diarthrodial joints—normal elasticity of the DRUJ diarthrodial capsule could be clinically compromised by hemorrhage, exudate, and scarring associated with trauma to the wrist, especially with the magnitude of injury associated with fracture of the distal radius. It also became clear to us that chronic, post-traumatic stiffness of the forearm, following either closed manipulation or surgical intervention for displaced distal radius fractures, might be
directly attributable to trauma-induced contracture of the dorsal or volar capsules of the distal radio-ulnar joint. Forearm stiffness could be a consequence of prolonged immobilization or limited range-of-motion following injury.
directly attributable to trauma-induced contracture of the dorsal or volar capsules of the distal radio-ulnar joint. Forearm stiffness could be a consequence of prolonged immobilization or limited range-of-motion following injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree