Distal Humerus Fractures: Open Reduction Internal Fixation
Daphne M. Beingessner
David P. Barei
INTRODUCTION
Intra-articular fractures of the distal humerus in adults are uncommon but complex and challenging injuries. They typically occur in young people as the result of high energy trauma and occur more commonly in males. As life expectancy grows, the incidence of distal humerus fractures in the elderly has increased, particularly in women. In this group of patients, fractures often occur as the result of a ground-level fall. Fixation in these patients with osteopenic bone may be difficult, and surgical tactics and newer implants continue to evolve to accommodate this challenge.
Historically patients did poorly with surgical management of this injury, but in the past 25 years, modern fixation techniques have dramatically improved outcomes. Today, the majority of patients experience only mild to moderate residual impairment and regain approximately 75% of their elbow motion and strength. Union rates between 90% and 100% have been reported. However, stable internal fixation that allows early range of elbow motion is mandatory to achieve such outcomes.
The elbow joint functions to position the hand in space. Restoration of elbow motion is essential to perform most activities of daily living. A range of motion between 30 and 130 degrees of flexion (100-degree arc) is necessary to perform most activities of daily living. Recent series of distal humerus fractures have demonstrated restoration of motion arcs of up to 112 degrees when repaired with contemporary fixation techniques.
The surgeon must have a thorough knowledge of the complex anatomy around the elbow prior to embarking on surgery of the distal humerus. The osseous anatomy can make plate contouring difficult, and precontoured periarticular plates have been developed to facilitate fixation. The flat posterolateral surface of the humerus is an ideal place for plate placement while the distal medial humerus invariably requires plate contouring for placement around the medial epicondyle. Virtually all surgical approaches involve identification and protection of the ulnar and radial nerves during exposure and hardware placement.
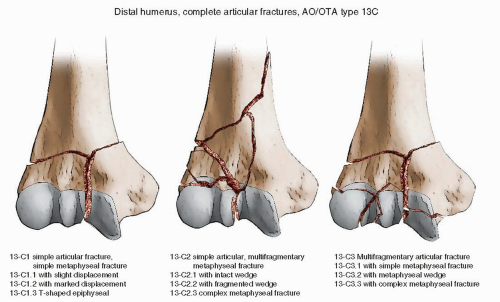
The most common classification used for distal humerus fractures is the OTA/AO classification system. Type A fractures are extra-articular, type B fractures are partial articular (such as isolated condyle fractures, coronal shear fractures, or epicondyle fractures), and type C fractures are complete articular injuries. Thirty-nine percent of fractures are type A, twenty-four percent type B, and thirty-seven percent type C. (Fig. 8.1)
INDICATIONS AND CONTRAINDICATIONS
Nonoperative treatment of displaced distal humerus fractures in adults leads to a high rate of nonunion, malunion, and elbow stiffness. It is typically reserved for low-demand elderly patients with significant medical comorbidities who cannot tolerate surgery. Such patients, particularly those with minimally displaced fractures or lowarticular injuries/shear injuries, can be treated with immobilization in a long arm cast for 3 weeks followed by
early range of elbow motion. For patients with significant displacement of the metaphysis, the soft tissues must be carefully monitored to be sure that there is no skin compromise secondary to displaced fragments.
early range of elbow motion. For patients with significant displacement of the metaphysis, the soft tissues must be carefully monitored to be sure that there is no skin compromise secondary to displaced fragments.
Comminuted intra-articular fractures in geriatric patients with significant osteopenia may be better treated with total elbow arthroplasty. In particular, fractures with significant shear components, articular comminution, and fractures that are below the olecranon fossa may be difficult to repair in osteopenic bone. However, arthroplasty should be reserved for low-demand patients as the long-term outcomes have shown a high incidence of implant loosening.
The vast majority of open and closed displaced intra-articular fractures in adults are best treated with open reduction and stable internal fixation that allows early range of motion to optimize elbow function. Distal humerus fractures continue to be challenging injuries to manage but with improved fixation techniques and implants, good outcomes are possible.
PREOPERATIVE PLANNING
History and Physical Examination
A complete history including mechanism of injury, preinjury condition, medical issues, and handedness should be obtained. Physical examination should identify open wounds, skin tenting, significant abrasions or contusions, nerve function (particularly ulnar and radial nerve), and associated injuries. A thorough vascular examination including peripheral pulses should be performed. If the peripheral pulse on the affected extremity is decreased, then noninvasive vascular studies should be performed, and any significant abnormalities should prompt a vascular surgery consultation. Although vascular injuries are uncommon, they can be missed due to the excellent collateral blood flow in the upper extremity. The patient should be medically optimized prior to surgical intervention, which is often lengthy.
Imaging Studies
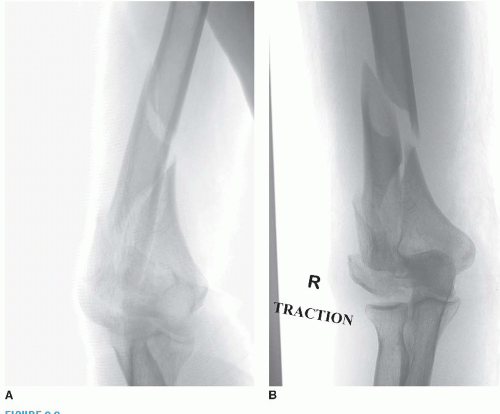
Typically, plain radiographs are sufficient to diagnose and develop a treatment plan. Radiographs should include the entire length of the humerus and the forearm. Traction radiographs are helpful to further delineate the fracture geometry (Fig. 8.2). With adequate analgesia, gentle traction is applied to the arm in the radiology suite, and an anteroposterior and lateral radiograph of the elbow is obtained. These radiographs should be studied to identify all components of the fracture. It is important to determine if there is continuity of the trochlear fragment to the medial epicondylar fragment as this can influence hardware choice. Unlike plateau or pilon fractures, computed tomography scanning is not usually needed but can be helpful when coronal plane injuries such as shear fractures of the capitellum and trochlea are suspected.
Timing of Surgery
Fractures should be immobilized in a long arm splint in a position that takes pressure off the skin. This position may vary according to fracture configuration but is often with the elbow semiextended. A hyperflexed position should be avoided to prevent development of a compartmental syndrome. In the absence of soft-tissue compromise or open injuries, the fracture should be treated on an urgent, but not emergent, basis. It is essential to have a complete and detailed preoperative plan to be sure that all required implants are available. The patient should be medically optimized since the surgery can be lengthy. Open fractures or those with significant soft-tissue compromise should be treated on an emergent basis. If the patient is not well enough for a prolonged procedure, an irrigation and débridement of the open wound may be performed followed by replacement of a well-padded splint and fixation when the patient’s condition permits. A spanning external fixator and staged fixation protocol is rarely necessary but may be useful for grossly contaminated open injuries or those with a vascular injury and repair.
The goal of treatment is anatomic and rigid fixation of the articular component of the injury and either absolute or relative stability of the metaphyseal component depending on the degree of comminution. A variety of implants may be required for provisional and definitive fixation of these fractures, and their availability should be confirmed preoperatively. These implants include 3.5-mm LCDC plates, 2.7- and 3.5-mm reconstruction plates, precontoured periarticular distal humerus nonlocking and locking plates, minifragment plates and screws (2.0, 2.4, and 2.7 mm), and Kirschner wires in various sizes (1.25, 1.6, and 2.0 mm). A variety of clamps including small and large Weber clamps, a small saw and osteotomes for an osteotomy, and bipolar cautery should also be available.
SURGERY
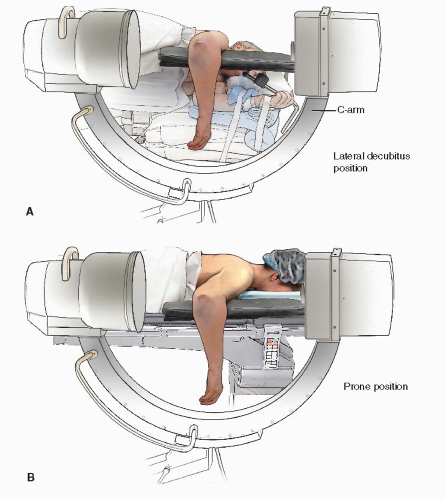
After appropriate medical evaluation, the patient is brought to the operating room, general anesthesia is induced, and preoperative antibiotics are administered. Because these fractures often require prolonged operating time, regional techniques of anesthesia are used less frequently. Advanced monitoring (i.e., arterial or central lines) is performed at the discretion of the anesthesiologist based on the patient’s physiologic status as well as comorbidities. A Foley catheter is routinely placed. The lateral decubitus or prone position allows for good visualization of the fracture as well as proper positioning of the C-arm. We prefer a lateral
position on a foam mattress with a radiolucent armboard since it decreases the potential risks of prolonged prone positioning such as eye injuries (Fig. 8.3). All pressure points must be carefully padded with particular care taken to avoid compression of the peroneal nerve at the knee or the lateral femoral cutaneous nerve at the hip. The prone position is useful for selected patients with spine injuries or fractures in their contralateral extremities. The lower arm is supported on a well-padded plexiglass armboard. Sequential compression devices are placed on the legs and used for the duration of the case. The C-arm is brought in from the head of the table. Prior to prepping and draping test, images should be obtained to ensure high-quality images during the procedure (Fig. 8.4A,B). The entire arm from shoulder to hand is prepped and draped (Fig. 8.5). A sterile tourniquet may be used but is not often necessary and may be in the way of a more extended incision. Injecting the proposed incision with Marcaine with Epinephrine helps with hemostasis during the exposure (Fig. 8.6).
position on a foam mattress with a radiolucent armboard since it decreases the potential risks of prolonged prone positioning such as eye injuries (Fig. 8.3). All pressure points must be carefully padded with particular care taken to avoid compression of the peroneal nerve at the knee or the lateral femoral cutaneous nerve at the hip. The prone position is useful for selected patients with spine injuries or fractures in their contralateral extremities. The lower arm is supported on a well-padded plexiglass armboard. Sequential compression devices are placed on the legs and used for the duration of the case. The C-arm is brought in from the head of the table. Prior to prepping and draping test, images should be obtained to ensure high-quality images during the procedure (Fig. 8.4A,B). The entire arm from shoulder to hand is prepped and draped (Fig. 8.5). A sterile tourniquet may be used but is not often necessary and may be in the way of a more extended incision. Injecting the proposed incision with Marcaine with Epinephrine helps with hemostasis during the exposure (Fig. 8.6).
A posterior midline incision is made, and full-thickness medial and lateral fasciocutaneous flaps are raised. It is important to elevate the deep fascia in order to more easily identify the ulnar and radial nerves (Fig. 8.7). The fracture is then exposed using a triceps-sparing approach (Fig. 8.8) or an olecranon osteotomy. We prefer these approaches since they are extensile and allow for excellent visualization of the joint. The preoperative plan should indicate which approach will be required. The triceps-sparing approach is the first step of the olcranon osteotomy approach and can easily be converted to an osteotomy should increased visualization be required. On the medial side, the ulnar nerve is identified proximal to the elbow joint under the medial triceps (Fig. 8.9). It is dissected approximately 15 cm proximal to the joint and distally to the level of its first motor branch into the flexor carpi ulnaris (Fig. 8.10). It can be fully elevated for transposition or left in situ and protected throughout the procedure depending on the fracture and fixation requirements. The triceps is then elevated from the posterior aspect of the humerus on the medial side by lifting it directly from the humerus and medial intermuscular septum (Fig. 8.11). Distally, the posterior band of the medial collateral ligament is elevated, and the posterior joint capsule is entered to visualize the trochlea. On the lateral side, the sensory branch of the radial nerve is identified in the fascia and followed proximally to the radial nerve proper, which typically lies just anterior to it (Fig. 8.12). The radial nerve
is identified as it crosses the posterior humerus proximally and distally as it travels anterior the intermuscular septum. If the fracture is distal and will not require long plates, the radial nerve does not need to be exposed, and dissection should remain posterior to the septum. The triceps is then elevated from the posterior humeral shaft. Distally, the anconeus may be divided or dissected on its lateral side to be elevated with the triceps (Fig. 8.13). The joint capsule is opened laterally and the fracture exposed. The visualization afforded by this approach is typically adequate for fractures with a simple articular split, particularly if it is lateral to the midpoint of the trochlea (Fig. 8.14). Fractures with three articular fragments may be converted to two fragments by reducing the middle segment to the medial or lateral joint fragment first and then reducing the remaining fracture.
is identified as it crosses the posterior humerus proximally and distally as it travels anterior the intermuscular septum. If the fracture is distal and will not require long plates, the radial nerve does not need to be exposed, and dissection should remain posterior to the septum. The triceps is then elevated from the posterior humeral shaft. Distally, the anconeus may be divided or dissected on its lateral side to be elevated with the triceps (Fig. 8.13). The joint capsule is opened laterally and the fracture exposed. The visualization afforded by this approach is typically adequate for fractures with a simple articular split, particularly if it is lateral to the midpoint of the trochlea (Fig. 8.14). Fractures with three articular fragments may be converted to two fragments by reducing the middle segment to the medial or lateral joint fragment first and then reducing the remaining fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree