Distal Humerus Fractures
CASE PRESENTATION
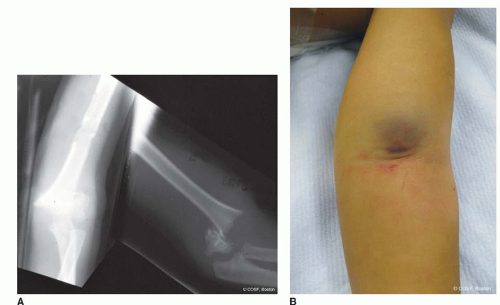
A 5-year-old male falls from the monkey bars at the playground and suffers a supracondylar humerus fracture of his nondominant elbow. No other injuries occurred with the fall. In the emergency room, he is noted to have a pale hand with no radial or ulnar pulse. Testing of his median nerve reveals absent light touch sensibility and no thenar intrinsic opposition or flexor pollicis longus (FPL) motor function. His radiographs reveal a completely displaced fracture (Figure 27-1).
CLINICAL QUESTIONS
What is the incidence of supracondylar humerus fractures?
How are these fractures classified?
What is the incidence of associated neurovascular injuries?
When is closed reduction or cast immobilization alone indicated?
What are the indications for closed reduction percutaneous pinning (CRPP)?
How frequently is open reduction internal fixation (ORIF) performed?
Are there indications for traction treatment?
Is an overnight delay for surgery safe?
Is it best to use lateral entry or crossed medial and lateral pins?
What is the significance of a pink pulseless hand?
When is exploration of the brachial artery indicated?
What is the risk of permanent neurologic injury?
When is surgical treatment of an injured nerve indicated?
What are the risk factors for a Volkmann ischemic contracture?
When is an osteotomy of a malunion indicated?
What is the best treatment for a T-condylar humerus fracture?
What are the diagnostic signs of a nonaccidental physeal fracture?
THE FUNDAMENTALS
Etiology and Epidemiology
Supracondylar humerus fractures are most often due to a fall from a height. It is usually the nondominant, outstretched arm (and therefore, typically the left arm since only 8% to 15% of the world’s population is lefthand dominant) that hits the ground first and hardest.1,2 Fortunately, most supracondylar fractures are isolated injuries. Children with ligamentous laxity and hyperextension at the elbow have a higher predilection for a supracondylar rather than a forearm fracture with a fall.3 The peak age is 5 to 6 years, which is also a time when children have more ligamentous laxity and resultant elbow hyperextension.4,5 The anatomic mechanism of injury is that the olecranon abuts the olecranon fossa, and the anterior capsule simultaneously provides anterior tension. This combination of traumatic forces propagates an extension fracture through the thin supracondylar bone of the distal humerus. Only about 1% of these injuries are open fractures, but near open fractures with entrapment of the brachialis muscle, periosteum, neurovascular structures, and skin and subcutaneous tissue in the fracture site are more common. On average, there is about an 8% risk of nerve injury. However, the more severely displaced the fracture, the higher the risk of neurovascular compromise. Displaced fractures have, on average, a 20% to 40% risk of neurovascular injury. Supracondylar fractures are the most common and riskiest fractures about the elbow in a child.
Floating elbow injuries with simultaneous supracondylar humerus and forearm fractures are an even higher energy trauma and, therefore, are at more risk for compartment syndrome. Metaphyseal-diaphyseal fractures are more often due to a direct blow and are harder to align by percutaneous pinning techniques. Nonaccidental trauma, including a difficult delivery at birth, can result in a distal humeral physeal separation. A high index of suspicion is necessary for acute diagnosis and treatment of transphyseal injuries, especially when the secondary centers of ossification have yet to appear. T-condylar humerus fractures are usually due to high-velocity sports injuries in the adolescent and require adult-type treatment for best results.
Clinical Evaluation
Physical Exam
A careful exam in the acute care setting is mandatory with supracondylar fractures. The presentation can range from minimal swelling and tenderness to marked deformity (Figure 27-2). With the nondisplaced, stable injuries, the child will not move or use the limb. The differential diagnosis includes, among others, infection (septic arthritis, osteomyelitis), inflammatory arthritis (Lyme, juvenile rheumatoid arthritis), nursemaid’s or pulled elbow, and an occult fracture elsewhere in the upper limb. Palpation of the entire limb from clavicle to fingers is required. Monitoring of body temperature, generalized physical exam for skin rashes or joint effusions, and appropriate laboratory testing for infection or inflammatory arthritis may be indicated. A posterior fat pad sign on the lateral radiograph is suggestive of a nondisplaced elbow fracture.6 These stable fractures are in a sense not a problem, as they will heal well without complications. You just do not want to miss a minimally displaced fracture with medial comminution that could drift into varus; an acute infection that needs surgical and antibiotic treatment; an inflammatory or systemic condition that you are treating instead as a localized trauma; or a nonaccidental trauma that puts a child at greater risk without social and medical intervention.
 FIGURE 27-2 Intraoperative photograph in splint of a displaced type III supracondylar humerus fracture with marked deformity and anterior ecchymosis. The distal capillary refill is intact. |
The displaced fractures are obvious by the deformity at presentation but need a very careful and critical exam for neurovascular compromise and associated injuries. Inspect the anterior cubital fossa for an open fracture, especially when the skin is tented and ecchymotic. Look for skin puckering that indicates the metaphyseal spike of the proximal fragment has entrapped the subcutaneous tissues. A pucker sign means more disruption of the brachialis muscle, soft tissues, and risk of neurovascular entrapment. A precise, step-by-step exam of the three
major nerves (median, radial, and ulnar) in the upper limb and vascularity of the hand (palpable pulses, capillary refill, and color of the hand) is imperative in all displaced fractures. The median nerve motor function is tested by isolating extrinsic (FPL and index finger flexor digitorum profundus [FDP II]) and intrinsic (thenar opposition) muscles; the ulnar nerve extrinsics by flexor digitorum profundus small finger (FDP V) and intrinsics by first dorsal interosseous (index finger abduction with metacarpophalangeal [MCP] joint flexion) muscle testing; and the radial nerve extrinsics by extensor pollicis longus (EPL) (thumb retropulsion and interphalangeal [IP] joint extension), extensor digitorum communis (EDC) (finger MCP joint extension), and/or wrist extension assessment. Of note, isolated nerve injuries to the anterior interosseous branch of the median nerve (FPL, FDP II) are the most common motor impairment with pediatric supracondylar humerus fractures due to this nerve’s location right next to the displaced fracture.7 The direction of fracture displacement usually coincides with the nerve injury and matches the local anatomy: median nerve injury from posterolateral fractures; radial nerve injury from posteromedial fractures; and ulnar nerve injury from flexion displacement.8 Multiple nerve injuries are common. Sensibility is tested by light touch in all children and two-point discrimination in children >5 years of age. Do not test sensibility by painful pin prick. The median nerve distribution for sensibility is thumb and index finger pulp; ulnar nerve is small finger pulp; radial nerve is dorsal first web space. Accurate preoperative documentation is critical to postoperative decision making. If you cannot tell the status of a nerve by motor and sensibility testing, be truthful in the chart and note that. Later, if the nerve is not functioning, an inaccurate exam or record can impair you or your consultants in making the best decisions about observation versus intervention.
major nerves (median, radial, and ulnar) in the upper limb and vascularity of the hand (palpable pulses, capillary refill, and color of the hand) is imperative in all displaced fractures. The median nerve motor function is tested by isolating extrinsic (FPL and index finger flexor digitorum profundus [FDP II]) and intrinsic (thenar opposition) muscles; the ulnar nerve extrinsics by flexor digitorum profundus small finger (FDP V) and intrinsics by first dorsal interosseous (index finger abduction with metacarpophalangeal [MCP] joint flexion) muscle testing; and the radial nerve extrinsics by extensor pollicis longus (EPL) (thumb retropulsion and interphalangeal [IP] joint extension), extensor digitorum communis (EDC) (finger MCP joint extension), and/or wrist extension assessment. Of note, isolated nerve injuries to the anterior interosseous branch of the median nerve (FPL, FDP II) are the most common motor impairment with pediatric supracondylar humerus fractures due to this nerve’s location right next to the displaced fracture.7 The direction of fracture displacement usually coincides with the nerve injury and matches the local anatomy: median nerve injury from posterolateral fractures; radial nerve injury from posteromedial fractures; and ulnar nerve injury from flexion displacement.8 Multiple nerve injuries are common. Sensibility is tested by light touch in all children and two-point discrimination in children >5 years of age. Do not test sensibility by painful pin prick. The median nerve distribution for sensibility is thumb and index finger pulp; ulnar nerve is small finger pulp; radial nerve is dorsal first web space. Accurate preoperative documentation is critical to postoperative decision making. If you cannot tell the status of a nerve by motor and sensibility testing, be truthful in the chart and note that. Later, if the nerve is not functioning, an inaccurate exam or record can impair you or your consultants in making the best decisions about observation versus intervention.
Assessing the vascularity to the hand is critical in defining the extent of soft tissue injury, risk of compartment syndrome, and operative urgency. Start with the color of the hand. Pale is a major problem; pink is obviously good. Up to 20% of supracondylar fractures will have vascular impairment upon presentation. Feel for a pulse and be certain it is not your own. Check the capillary refill, which is normally <3 seconds, and feel the fullness of the pulp. The patient can have a pink hand with normal capillary refill, full pulp, and still have no pulse, thus, the pink pulseless hand (see Sidebar 1). If the median nerve is out in a pink pulseless hand, this is still a surgical emergency. No one will disagree that a pale pulseless hand is a surgical emergency. Also, always look for at risk signs and symptoms for a developing compartment syndrome that will lead you to the operating room more emergently. They include marked swelling, skin puckering, absent pulse and nerve impairment, no bony contact of fracture fragments, and an increasing analgesia requirement that does not relieve the pain, among others.
Radiographic Classification
For evaluation of an acute elbow injury, anteroposterior (AP) and lateral radiographs are standard. Unfortunately, you usually get at least one if not two oblique views instead. Requesting views of the elbow rather than of the distal humerus compounds the problem since all elbow injuries present with an elbow flexion posture. This leads to overlap of the proximal forearm and distal humerus on the AP x-ray view of the elbow, but AP and lateral views of the distal humerus will reveal clear images of the fracture.
Distal humeral varus-valgus alignment is assessed by Baumann angle of the humeral-capitellar line on the AP view (Figure 27-3).9, 10, 11 and 12 On the lateral view, the anterior humeral line through the anterior half of the capitellum and the lateral humeral-capitellar angle (usually 40 degrees) defines flexion-extension deformity (Figure 27-4).13 Since the capitellar secondary center of ossification is the first to appear at 1 to 2 years, the alignment of the distal humerus in most pediatric traumatic injuries can be evaluated by humeral capitellar measurements. The medial epicondylar epiphyseal angle is used by some to assess fracture malalignment and adequacy of reduction in the child old enough to have the medial epicondylar secondary center of ossification.14 An anterior fat pad sign is often normal, but a posterior fat pad sign is frequently
indicative of an occult elbow fracture (Figure 27-5). The use of CT scans is generally reserved for T-condylar humerus fractures, while MRI scans are employed when there is a diagnostic dilemma or complex fracture dislocation to reveal injuries to the physeal and/or articular cartilage. Ultrasounds are helpful in nonaccidental trauma before the secondary centers of ossification appear.15, 16 and 17
indicative of an occult elbow fracture (Figure 27-5). The use of CT scans is generally reserved for T-condylar humerus fractures, while MRI scans are employed when there is a diagnostic dilemma or complex fracture dislocation to reveal injuries to the physeal and/or articular cartilage. Ultrasounds are helpful in nonaccidental trauma before the secondary centers of ossification appear.15, 16 and 17
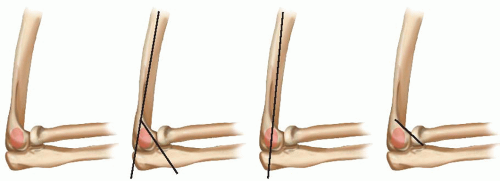
Supracondylar and transphyseal fractures are classified by direction and degree of displacement. Up to 98% of fractures are displaced in extension. The extension fractures are further defined as posteromedial (varus) or posterolateral (valgus). Flexion deformity occurs rarely. Both extension and flexion fractures have three-dimensional deformity and thus also malrotation.18 The Gartland classification and its modifications define the degree of displacement: type I nondisplaced, type II displaced but hinged with cortical contact, and type III displaced with no cortical contact.19, 20 and 21 The modified Gartland classification really helps determine the type of treatment (immobilization alone, closed reduction and immobilization, and reduction and pinning), timing of surgical intervention (emergent, urgent in the morning, or in the next few days), and risk of neurovascular impairment (the higher the class type, the greater the risk). Beware of the “tweeners”: Type “1.5” may collapse and be a risk for deformity in a cast (Figure 27-6), type “2.5” is more at risk for instability and neurovascular compromise, and type “3.5” may be unstable in all directions (Skaggs type IV).
 FIGURE 27-5 Lateral radiograph revealing both an anterior and posterior fat pad sign. This patient had a mild supracondylar humerus fracture treated closed. |
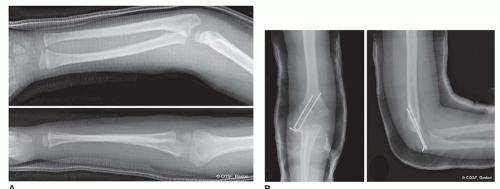
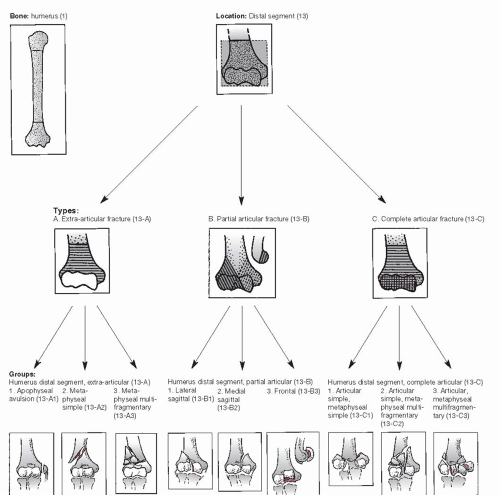
Intra-articular humerus fractures are defined by column (medial, lateral, or both) and degree of comminution. The AO classification is used most often (Figure 27-7). T-condylar fractures in the adolescent are usually AO C1 and C2 injuries. Metaphyseal-diaphyseal fractures are separate entities and need to be recognized as such for proper treatment and fixation decisions (Figure 27-8).22 Floating elbow injuries include simultaneous fractures above and below the elbow joint. More proximal open fractures may require external fixation.
Surgical Indications
The strong take from the weak, but the smart take from the strong.
—Pete Carril
All displaced supracondylar, transphyseal, metaphysealdiaphyseal, and T-condylar fractures require reduction and stabilization (Figure 27-9). Almost all, if not all, of these injuries are treated with operative fixation, either percutaneous or open. The major differences in treatment have to do not with whether to perform surgery but rather when and how. Open fractures, pending compartment syndromes, and avascular limbs are emergencies. There is now sufficient evidence to know that overnight delay in surgery is acceptable as long as there is not vascular compromise, worsening peripheral neurologic status, and the wait is not too long (see Coach’s Corner).23, 24, 25, 26, 27, 28, 29 and 30
SURGICAL PROCEDURES
You can discover more about a person in an hour of play than in a year of conversation.
—Plato
It is important to understand that: (1) there are many different ways to successfully treat supracondylar humerus fractures, and (2) supracondylar humerus fractures have the highest rate of complications of any pediatric fracture. The standard of treatment now is CRPP for displaced supracondylar and transphyseal fractures. The surgical variance is on how many pins (two, three, or rarely more); entry site (lateral only or medial and lateral); and angle of pin placement (parallel or divergent [preferred], distal to proximal [by far the most common], or proximal to distal). Closed reduction and immobilization (cast, collar, and cuff) and traction treatment can be successful, but both have higher rates of malunion and are used rarely now. The ORIF approach is reserved for an avascular limb and irreducible and open supracondylar fractures but could be performed successfully for many displaced fractures. An ORIF with bicolumn plates and screws is the standard treatment for T-condylar humerus fractures in children and adolescents,31 but some simpler fractures in younger children can be treated with multiple percutaneous pins and/or screws. Both the choosing and the execution of the treatment really make a difference in the outcome of these injuries.
• Immobilization
The nondisplaced, stable fracture will heal regardless of what immobilization is chosen. Sling, collar and cuff, posterior splints, and casts have all been used successfully. There is some limited evidence that the children are more comfortable in a posterior above-elbow splint or bivalved cast. Immobilization also protects against repeat injury that could lead to fracture displacement.32 It is important not to mistake the fracture with minimal medial comminution for a nondisplaced, stable fracture, as this “tweener type 1.5” fracture is the one that will drift and heal in varus and extension with limited immobilization.33
▪ Closed Reduction
Type II and even some type III fractures have been treated successfully with closed reduction and cast, sling, splint, or collar and cuff immobilization.34, 35, 36, 37, 38, 39, 40, 41 and 42 If closed reduction and immobilization are chosen, careful follow-up clinically and radiographically is necessary to prevent complications. Supracondylar, and especially transphyseal, fractures heal quickly, and there is limited time for repeat reduction. Successful second reduction or conversion to a CRPP or ORIF technique for an impending malunion has been reported on average at 6 days with a range from 2 to 19 days.43 For us, all displaced (type II and III) fractures are treated with operative reduction and pin stabilization.44,45 The CRPP approach lessens the risk of malunion in an extended (<90 degrees) cast and neurovascular compromise in a flexed (>120 degrees) cast.46
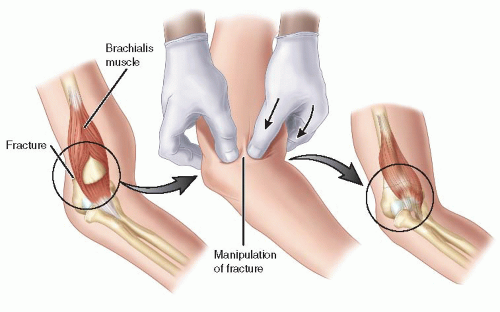
The reduction technique is the same for closed reduction and immobilization or CRPP. With the patient under anesthesia, gentle longitudinal traction is applied with the arm in approximately 30 degrees of flexion until the soft tissues and bony fragments disengage. The closed reduction can be performed with one of the surgeon’s hands controlling the distal fragment and the other hand stabilizing the upper arm and proximal fragment or by the surgeon distracting with both hands on the forearm or distal fragment and the assistant holding the upper arm. If there is brachialis muscle entrapment by the metaphyseal
proximal fragment, the milking maneuver is performed from proximal to distal (Figure 27-10).47,48 Once the fracture fragments are mobile, valgus-varus malalignment is corrected in 30 to 40 degrees of elbow flexion to prevent neurovascular entrapment. The surgeon’s thumb controls one side of the humerus, and the other digits control the other side of the humerus during correction of malalignment (Figure 27-11). Finally, the surgeon’s hands are rotated with the thumb over the olecranon apophysis and displaced distal fragment, and the rest of the hand is anterior on the humeral diaphysis to stabilize the proximal fragment (Figure 27-12). An alternative method is to have both of the surgeon’s thumbs on the olecranon and the fingers of both hands on the proximal humerus. The extended fragment is then flexed >120 degrees by holding the proximal fragment stable and bringing the olecranon
and distal fragment into anatomic position. To correct malrotation and provide periosteal tension band stability, forearm rotation is performed during flexion reduction. For most fractures, this is in pronation. For some posterolateral fractures, this is in supination. (In the more common posteromedially displaced fractures, the lateral periosteum is torn; therefore, additional stability is conferred by pronating the forearm, as this tensions the lateral muscles and soft tissues. Conversely, in posterolateral injuries, the medial periosteum is disrupted, and forearm supination will add stability by tightening the flexor-pronator mass and medial soft tissues.) Proper rotational positioning can be assessed under fluoroscopy. To maintain a stable closed reduction, >120 degrees of flexion is required, which is risky for neurovascular compromise. This is why now all these fractures are pinned.49, 50 and 51 If there is a persistent bony block to flexion during reduction, then the fragments have not been disengaged. If there is a “mushy” or “rubbery” feeling, then there is soft tissue interposed, the most worrisome of which could involve the NVB. Confirmation of anatomic reduction is obtained with AP, lateral, and oblique radiographs of the distal humerus. Irreducible fractures, especially those with neurovascular entrapment, require open reduction. The vascularity to the hand is always assessed after closed reduction by feeling for a pulse and checking the color, capillary refill, and fullness of the digital pulps (Figure 27-13).
proximal fragment, the milking maneuver is performed from proximal to distal (Figure 27-10).47,48 Once the fracture fragments are mobile, valgus-varus malalignment is corrected in 30 to 40 degrees of elbow flexion to prevent neurovascular entrapment. The surgeon’s thumb controls one side of the humerus, and the other digits control the other side of the humerus during correction of malalignment (Figure 27-11). Finally, the surgeon’s hands are rotated with the thumb over the olecranon apophysis and displaced distal fragment, and the rest of the hand is anterior on the humeral diaphysis to stabilize the proximal fragment (Figure 27-12). An alternative method is to have both of the surgeon’s thumbs on the olecranon and the fingers of both hands on the proximal humerus. The extended fragment is then flexed >120 degrees by holding the proximal fragment stable and bringing the olecranon
and distal fragment into anatomic position. To correct malrotation and provide periosteal tension band stability, forearm rotation is performed during flexion reduction. For most fractures, this is in pronation. For some posterolateral fractures, this is in supination. (In the more common posteromedially displaced fractures, the lateral periosteum is torn; therefore, additional stability is conferred by pronating the forearm, as this tensions the lateral muscles and soft tissues. Conversely, in posterolateral injuries, the medial periosteum is disrupted, and forearm supination will add stability by tightening the flexor-pronator mass and medial soft tissues.) Proper rotational positioning can be assessed under fluoroscopy. To maintain a stable closed reduction, >120 degrees of flexion is required, which is risky for neurovascular compromise. This is why now all these fractures are pinned.49, 50 and 51 If there is a persistent bony block to flexion during reduction, then the fragments have not been disengaged. If there is a “mushy” or “rubbery” feeling, then there is soft tissue interposed, the most worrisome of which could involve the NVB. Confirmation of anatomic reduction is obtained with AP, lateral, and oblique radiographs of the distal humerus. Irreducible fractures, especially those with neurovascular entrapment, require open reduction. The vascularity to the hand is always assessed after closed reduction by feeling for a pulse and checking the color, capillary refill, and fullness of the digital pulps (Figure 27-13).
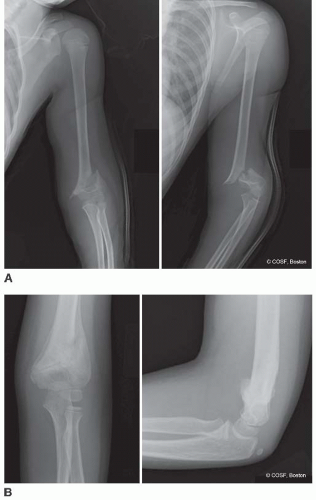 FIGURE 27-8 A: Metaphyseal-diaphyseal fracture with displacement. B: Healed fracture after pin removal. |
▪ Closed Reduction Percutaneous Pinning Supracondylar and Transphyseal Fractures
The techniques of CRPP vary in terms of body position (supine [preferred at most centers including ours] or
prone)52, 53 and 54; divergent lateral entry or medial and lateral entry crossed pins; number of pins placed (two or three); use of arm support (fluoroscopy image intensifier or fluoroscopic arm board); and whether you move the arm through the shoulder (not the fracture site) or rotate the fluoroscopy to obtain a lateral image of the reduction and pinning.
prone)52, 53 and 54; divergent lateral entry or medial and lateral entry crossed pins; number of pins placed (two or three); use of arm support (fluoroscopy image intensifier or fluoroscopic arm board); and whether you move the arm through the shoulder (not the fracture site) or rotate the fluoroscopy to obtain a lateral image of the reduction and pinning.
Our method is to perform closed reduction under general anesthesia in the operating room in the supine position after sterile prepping and draping. The fluoroscopy image intensifier is used as the arm support. The forearm, elbow joint in full flexion, and humerus are rotated as a single, stable unit through the shoulder to obtain AP, oblique (optimal views of medial and lateral columns), and lateral fluoroscopic images. Young children have sufficient tension-free shoulder external rotation to 90 degrees or greater to do this safely without loss of fracture reduction. The lateral entry pins are placed obliquely from distal to proximal with one up the lateral column and one across the olecranon fossa (Figure 27-14). The proximal medial humeral cortex needs to be penetrated with each pin for sufficient stability. The medial cortical penetration can be felt by the operating surgeon, heard by the change in pitch of the drill by others in the room, and confirmed by fluoroscopy. The preferred pin size is 5/64″ for children >20 kg and 0.0625″ for children <20 kg. The fracture stability is tested manually with flexion-extension and rotation movements; brief continuous fluoroscopy can be used for confirmation.55, 56 and 57 If the fracture is at all unstable or acceptable but not perfect, a third lateral pin or a medial pin is placed (Figure 27-15).58, 59, 60 and 61 Biomechanical analysis indicates crossed pins are more stable; clinical evidence
confirms this trend, but three divergent lateral pins suffice in most cases.62, 63 and 64 Divergent lateral pins are more stable than parallel lateral pins.65
confirms this trend, but three divergent lateral pins suffice in most cases.62, 63 and 64 Divergent lateral pins are more stable than parallel lateral pins.65
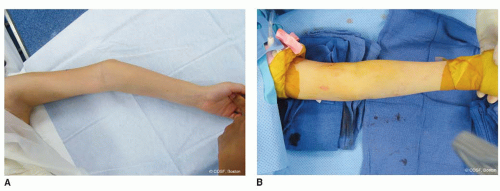 FIGURE 27-11 A: Varus deformity noted on intraoperative clinical image before closed reduction. B: Anatomic carrying angle restored with closed reduction on fluoroscopic image intensifier. |
Although medial pins raise the concern of iatrogenic ulnar nerve injury,66, 67 and 68 they can be placed safely through a small incision.69 Since ulnar nerve instability is common in this age group,70 the medial pin is placed with <90 degrees of elbow flexion to avoid impingement or injury. The ulnar nerve is identified and protected with a retractor. The pin entry site is more anterior on the medial epicondyle to avoid the posterior position of the ulnar nerve. The pin trajectory is more horizontal to prevent nerve compression.71 Oscillating technique with the drill is used to prevent soft tissue engagement by the wire that could compress or kink the nerve. Again, confirmation of desired pin placement, fracture alignment, and stability are obtained on the intraoperative fluoroscopic images. The final act when using a medial pin is to check the ulnar nerve, being certain there is no compression, impingement, or kinking of the nerve at rest and with full elbow movement. The wire is bent anterior to lessen the risk of problems.
Of note, flexion type and multiple-plane, unstable extension fractures can be much harder. To achieve anatomic alignment with CRPP, the fracture fragments often need to be held reduced in space by the surgeon or assistant while the other one gets the first stabilizing lateral entry pin in place. The position is usually with maximum distraction and flexion of 60 to 80 degrees while correcting the varus-valgus malalignment. In flexion-type injuries, axial loading of the forearm may assist in reduction, as the proximal radius and ulna push against the flexed distal humerus. The reduction and pinning are based on the AP plain images only. Be careful not to overirradiate your hands. Once the first pin is across, then the other pin(s) can be placed in the typical fashion noted above. On occasion, two pins are placed appropriately in the distal fragment and used to joystick the fracture reduction before being passed into the proximal fragment.72 There is a higher incidence of open reduction with flexion injuries. If the ulnar nerve is out preoperatively, decompression is appropriate at the time of open reduction.73
Transphyseal fractures are often markedly unstable. The children are often very young, and the diagnosis can be delayed due to the nonaccidental trauma etiology. If you are fortunate enough to make the diagnosis early, CRPP is indicated. In the very young, an intraoperative elbow arthrogram is often necessary to confirm the diagnosis, location of the epiphysis, and articular surface and to guide anatomic reduction (Figure 27-16). Since the periosteum can be disrupted all the way to the shoulder by the force of injury, pin stabilization with two to three lateral pins or crossed pins is mandatory. Placement of these pins is not easy in the small child with a maximally swollen elbow and limited views of the osseous and cartilaginous fracture fragments arthrofluoroscopically.
The metaphyseal-diaphyseal fractures have more obliquity to them and a tendency toward malangulation even after pinning.22 Some of these fractures need an intramedullary pin or more proximal pin placement to maintain varus-valgus alignment. The radial nerve becomes more at risk the more proximal you place your lateral pins.
If there is a floating elbow injury, pin both the supracondylar and forearm fractures to avoid the risk of a
compartment syndrome in a cast. The most common floating elbow combination in a child is distal radius and supracondylar fractures. The distal radius is pinned first (see Chapter 34



compartment syndrome in a cast. The most common floating elbow combination in a child is distal radius and supracondylar fractures. The distal radius is pinned first (see Chapter 34
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree