Distal Femur Osteoarticular Allograft
Luis A. Aponte-Tinao
German L. Farfalli
Miguel A. Ayerza
D. Luis Muscolo
Distal femur osteoarticular allografts are utilized for reconstruction of the proximal side of the knee after tumor resection. Osteoarticular allografts do not sacrifice the side of the joint that is not compromise by the tumor and have the possibility of attaching soft-tissues. Reconstruction of the ligaments, tendons, and joint capsule must be meticulous and precise, since the longevity of these grafts is related in part to the stability of the joint. Care must be taken to avoid malalignment that will put greater stress on the allograft cartilage.
INDICATIONS
The procedure is appropriate for the treatment of a massive osteoarticular defect after tumor resection or massive traumatic bone losses.
The major neurovascular bundle must be free of tumor.
CONTRAINDICATIONS
Patients in whom preoperative imaging studies demonstrate evidence of intra-articular compromise of the tumor.
Inadequate host soft tissue to reconstruct the joint.
Patients with cartilage degenerative disease of the proximal tibia.
PREOPERATIVE PREPARATION: ALLOGRAFT SELECTION
Fresh frozen allografts are obtained and stored according to a technique that has been previously described (1). Poor anatomical matching of both size and shape between the host defect and the graft can significantly alter joint kinematics and load distribution, leading to bone resorption or joint degeneration. To improve accuracy in size matching between the donor and the host, we developed measurable parameters based on CT scans of the distal femur. In the axial view of the distal femur, we measure the maximum total width and anteroposterior width of the medial and lateral condyles (Fig. 17.1), and the width of the intercondylar notch. The allograft is selected on the basis of a comparison of these measures with those of the donor.
TECHNIQUE
All operations are performed in a clean air enclosure with vertical airflow and usually with spinal anesthesia. The patient is placed on the operating table in the supine position. A sandbag is placed under the ipsilateral buttock. A long midline incision is made (Fig. 17.2), beginning in the middle part of the thigh, and a medial
parapatellar arthrotomy is performed with the eversion of the patella in a similar way as in a total knee replacement to enable a wide exposure of the distal part of the femur and the knee joint (Fig. 17.3). The biopsy track is left in continuity with the specimen. The cruciate and collateral ligaments are identified and sectioned near the femur insertion to ensure that there is enough host tissue to reconstruct these ligaments with the donor. The distal part of the femur is approached through the interval between the rectus femoris and the vastus medialis. If there is an extraosseous tumor component, a cuff of normal muscle must be excised. Femoral osteotomy is performed at the appropriate location as determined on the basis of the preoperative imaging studies. All remaining soft tissues at the level of the transection are cleared. After the posterior and medial structures have been protected and retracted, the osteotomy is performed perpendicular to the long axis of the femur. Following the osteotomy, the distal part of the femur is pulled forward in order to expose the soft-tissue attachments of the popliteal space. The popliteal artery is mobilized, and the geniculate vessels are ligated and transected. Both heads of the gastrocnemius are released, and the posterior capsule is sectioned near the femoral insertion. The distal femur is then passed off the operative field (Fig. 17.4).
parapatellar arthrotomy is performed with the eversion of the patella in a similar way as in a total knee replacement to enable a wide exposure of the distal part of the femur and the knee joint (Fig. 17.3). The biopsy track is left in continuity with the specimen. The cruciate and collateral ligaments are identified and sectioned near the femur insertion to ensure that there is enough host tissue to reconstruct these ligaments with the donor. The distal part of the femur is approached through the interval between the rectus femoris and the vastus medialis. If there is an extraosseous tumor component, a cuff of normal muscle must be excised. Femoral osteotomy is performed at the appropriate location as determined on the basis of the preoperative imaging studies. All remaining soft tissues at the level of the transection are cleared. After the posterior and medial structures have been protected and retracted, the osteotomy is performed perpendicular to the long axis of the femur. Following the osteotomy, the distal part of the femur is pulled forward in order to expose the soft-tissue attachments of the popliteal space. The popliteal artery is mobilized, and the geniculate vessels are ligated and transected. Both heads of the gastrocnemius are released, and the posterior capsule is sectioned near the femoral insertion. The distal femur is then passed off the operative field (Fig. 17.4).
 FIGURE 17.1 Axial view of a distal femur allograft CT scan prior to implantation that shows the measure of the maximum total width and the anteroposterior width of the medial and lateral condyles. |
 FIGURE 17.2 Intraoperative photograph that shows the long midline incision that is made beginning in the middle part of the thigh. |
 FIGURE 17.3 Intraoperative photograph showing wide exposure of the distal femur after medial parapatellar arthrotomy is performed. |
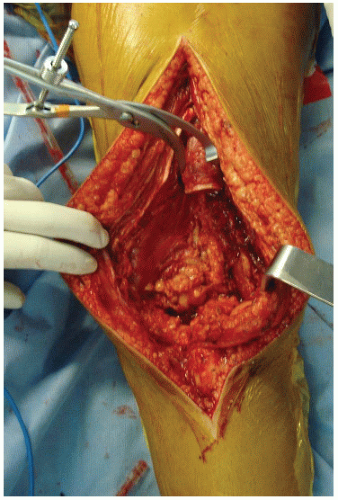 FIGURE 17.4 ntraoperative radiograph made after the distal femur is passed off the operative field, showing the osteoarticular defect. |
Simultaneous with the tumor resection, the allograft specimen is prepared in the back table. The graft is taken out of the plastic packaging and placed directly in a warm normal saline solution. After being thawed, the donor bone is cut to the proper length and soft-tissue structures such as the cruciate ligaments, collateral ligaments, and posterior capsule are prepared for implantation. It is crucial for joint reconstruction to have adequate soft-tissue structures in order to repair them to correspondent host tissues.
After resection of the tumor, the distal femoral transplant is inspected to confirm that the size is appropriate and no degenerative changes are present (Fig. 17.5). In order to avoid varus-valgus malalignment between the graft and the recipient we placed both on the back table surface to compare angular valgus and osteotomy parallelism between the host and donor (Fig. 17.6). Then the insertion of an allograft segment tailored to fit the bone defect is performed. Fitting the osteotomy between the host and donor in close apposition is a crucial step. When cortical bone is avascular, as in the allograft side, long-lasting stability is required and under this situation absolute stability offers the best conditions and chances for healing. The diaphyseal osteotomy is stabilized by internal fixation with an anterior short plate (Fig. 17.7), and in order to minimize the risk of fracture an additional lateral condylar buttress plate is placed in order to covers the entire length of the allograft (Fig. 17.8). Once we have secured the allograft bone with the host the knee is flexed to allow joint reconstruction (Fig. 17.9




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








