Distal Biceps Tendon Tears: Surgical Indications and Techniques
Cory Edgar
Augustus D. Mazzocca
The surgical treatment of distal biceps ruptures is becoming a more commonly performed procedure. It is unclear if the incidence, reported in 2002 to be approximately 1.2 patients per 100,000 in the general population (1), has changed much in the last 10 years. However, the increasing demands of a middle-aged population, along with multiple advances in the fixation technology and a renewed focus on the local anatomy, have allowed for less invasive exposures and decreased complications and permit a more aggressive postoperative rehabilitation.
The injury is most commonly observed in males, within the dominant extremity, and in a middle-aged population 40 to 50 years old (1, 2, 3 and 4). Reported risk factors include smoking or nicotine exposure (1, 5) and anabolic steroid use (5, 6). The mechanism is most commonly attributed to eccentrically loaded arm under tension while the elbow is flexed at about 90° and pulled into extension.
The etiology of the distal biceps ruptures is still unclear as many patients report no pain prior to the moment of rupture, whereas others report an insidious deep elbow pain for weeks to months leading up to the rupture. Utilizing a cadaver injection study in 27 elbows, a consistent vascular pattern was identified and supported the theory of a hypovascular zone within the tendon approximately 2.14 cm in length within the central zone 2 of the tendon (7). This may lead to degenerative tendon associated with repeated microtrauma to the tendon (7). Morrey and others (8, 9 and 10) have suggested that an abnormal boney prominence or irregularities at the radial tuberosity are associated with tendon degeneration and lead to ruptures; however, boney abnormalities at this location may simply be normal anatomic variant (11). Some combination of anatomic factors and local tendon degeneration probably contribute to failure of the distal biceps tendon, but the precise mechanism has yet to be demonstrated.
ANATOMY/OSTEOLOGY
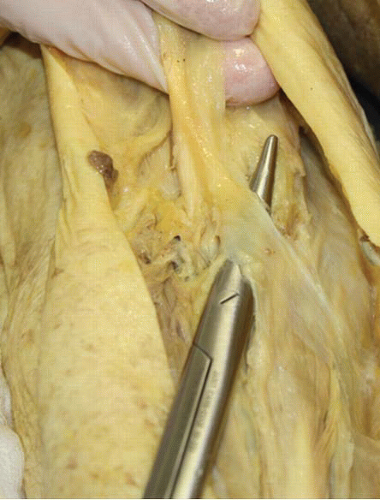
An understanding of the anatomy of the biceps origin and the osteology of the bicipital tuberosity is an essential aspect to getting an anatomic repair and better postoperative function. The biceps tendon inserts like a ribbon at the ulnar side of the lesser tuberosity, rather than as a cylinder on the center of the tuberosity (Fig. 38.1). The distal insertion of the short head positions it to be a more powerful flexor of the elbow, and the insertion of the long head on the tuberosity farther from the axis of rotation of the forearm increases leverage for supination. The average length of the biceps tendon insertion on the tuberosity is 21 mm, with an average width of 7 mm, indicating that the tendon insertion does not occupy the entire bicipital tuberosity (11, 12). The tuberosity does demonstrate some anatomic variability but has a mean length of 22 to 24 mm, a mean width of 15 to 19 mm, and it is located on the ulnar, posterior aspect of the proximal radius on average 25 mm from the radial head (11). The tendon insertion footprint is a ribbon-shaped configuration on the most ulnar aspect of the tuberosity, and it occupies 63% of the length and 13% of the width of the entire boney tuberosity (11).
The lacertus fibrosus (bicipital aponeurosis) typically originates from the distal short head of the biceps tendon, passes anterior to the elbow joint, and expands ulnarly blending with the fascia of the forearm (Fig. 38.2). It is composed of three layers that originate from the short head of the tendon and assists in stabilizing the tendon distally. As the forearm flexors contract, they tense the lacertus, subsequently causing a medial pull on the biceps tendon and perhaps contributing to its rupture, and can commonly mask a complete rupture during clinical examination.
CLINICAL EVALUATION AND WORKUP
Patients with complete distal biceps tendon ruptures usually report feeling a sudden, sharp, painful tearing sensation in the antecubital region of the elbow when an unexpected extension force was applied to the flexed/supinated arm. Occasionally, pain is also present in the posterolateral aspect of the elbow. The acute pain subsides
in a few hours and is replaced by a dull ache. Elbow range of motion is typically not affected, but symptoms of weakness and fatigue can occur with repetitive flexion and supination activities. Examination reveals tenderness in the antecubital fossa in the acute setting, and a defect can usually be palpated there. The “hook test,” as described by O’Driscoll et al. (13), is a means of palpating the tendon under resisted elbow flexion at about 70°; the biceps tendon can be “hooked” with a deep probing digit working lateral to medial just proximal to the crease.
in a few hours and is replaced by a dull ache. Elbow range of motion is typically not affected, but symptoms of weakness and fatigue can occur with repetitive flexion and supination activities. Examination reveals tenderness in the antecubital fossa in the acute setting, and a defect can usually be palpated there. The “hook test,” as described by O’Driscoll et al. (13), is a means of palpating the tendon under resisted elbow flexion at about 70°; the biceps tendon can be “hooked” with a deep probing digit working lateral to medial just proximal to the crease.
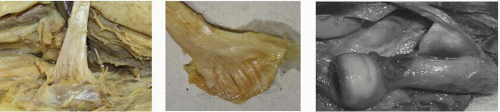 FIGURE 38.1. Cadaver dissections of distal biceps origin demonstrating the ulnar and posterior attachment and the ribbon footprint at the tendon entheses. |
The biceps is the main supinator of the arm and secondary flexor. Active flexion and supination of the elbow causes the biceps muscle belly to retract proximally, accentuating the defect in the antecubital fossa. If the biceps tendon can be palpated in the antecubital fossa, a partial rupture of the distal biceps tendon should be considered. Ecchymosis and swelling are usually evident in the antecubital fossa and along the medial aspect of the arm and proximal forearm. Plain radiographs generally do not show any bony changes, although irregularity and enlargement of the radial tuberosity and avulsion of a portion of the radial tuberosity have been reported with complete ruptures of the distal biceps tendon. We feel this is important to obtain for complete evaluation of the patient. MRI can be helpful to distinguish complete from partial ruptures and to differentiate partial rupture from tendinosis, tenosynovitis hematoma, and brachialis contusion. More importantly, in the rare but potentially difficult situation of a more proximal rupture of the distal biceps approaching the myotendinous junction, an MRI may aid in diagnosis (Fig. 38.3). In this setting, an allograft Achilles tendon should be made available to augment the length of the shortened tendon.
TREATMENT
Nonoperative Versus Operative Repair
There is a small role for nonsurgical management of distal biceps ruptures in the patient with low demand work and recreational activity function, older age or within a medically high-risk patient. There have been a few studies demonstrating some success with nonoperative treatment of distal biceps ruptures, stating patients had minimal functional loss and could lead to a full return to work as early as 4 weeks after injury (14, 15). However, more recent studies clearly show that unrepaired avulsion of the distal biceps tendon frequently leaves the patient with substantial weakness of supination and elbow flexion (16, 17, 18 and 19). Excellent subjective and objective results of surgical repair have been reported (4, 10, 19, 20, 21 and 22). Results with surgical repair have been superior to nonsurgical treatment in terms of restoring elbow flexion strength (30% improved), supination strength (40% improved), and upper extremity endurance (14). This statement is supported by the study by Baker and Bierwagen (16) in which cybex strength testing was performed on 13 patients treated with and without distal biceps reattachment. They reported 40% loss of supination strength, 79% loss of supination endurance,
30% loss of flexion strength, and 30% loss of flexion endurance in those patients treated nonoperatively (16). In a similar study, Morrey and coworkers (19) also showed a 40% loss of supination and 30% loss of flexion strength following nonoperative treatment for distal biceps ruptures.
30% loss of flexion strength, and 30% loss of flexion endurance in those patients treated nonoperatively (16). In a similar study, Morrey and coworkers (19) also showed a 40% loss of supination and 30% loss of flexion strength following nonoperative treatment for distal biceps ruptures.
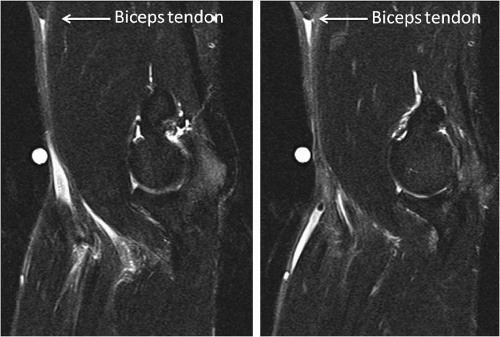 FIGURE 38.3. MRI right elbow, two cuts 9 mm apart moving medial to lateral. Note the ulnar-humeral joint and the very proximal, barely in the scanned field proximal biceps tendon tear and edema within the antecubital fossa.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|