CHAPTER 13 Disorders of the Sternoclavicular Joint
The first detailed case report of a sternoclavicular joint injury appeared as early as 1843,1 and numerous related articles appeared in the late 19th century. However, it was not until the 1920s and 1930s that such articles appeared in the American literature.2–4
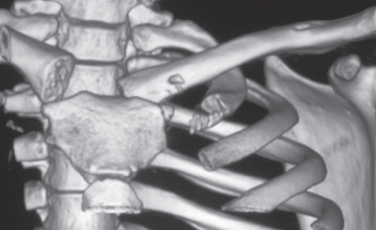
Injuries to the sternoclavicular joint are an uncommon problem and many authors apologize for reporting only three or four cases. The rarity of these injuries and the lack of standardized methods for treatment, measuring outcomes, and reporting complications increases methodologic flaws in structured literature reviews and often precludes a meaningful meta-analysis. From a review of the literature and in our combined 50 years of clinical experience, anterior dislocations are best treated nonoperatively, and posterior dislocations, which have accounted for deaths, need to be promptly diagnosed and reduced. Anterior and posterior injuries in adults up to age 23 years are usually physeal injuries and heal without specific treatment. Special radiographs are usually required to make the diagnosis. In our experience, high definition three-dimensional computed tomography (CT) images are the gold standard for evaluating these injuries (Fig. 13-1).
SURGICAL ANATOMY
The sternoclavicular joint is a diarthrodial joint and is the only true articulation between the upper extremity and the axial skeleton. The articular surface of the clavicle is much larger than that of the sternum, and both are covered with fibrocartilage. The enlarged bulbous medial end of the clavicle is concave front to back and convex vertically and therefore creates a saddle-type joint with the clavicular notch of the sternum. The clavicular notch of the sternum is curved, and the joint surfaces are not congruent. In 2.5% of patients there is a small facet on the inferior aspect of the medial clavicle, which articulates with the superior aspect of the first rib at its synchondral junction with the sternum.5
Ligaments of the Sternoclavicular Joint
Intra-articular Disk Ligament
The intra-articular disk ligament is a very dense, fibrous structure that arises from the synchondral junction of the first rib with the sternum and passes through the sternoclavicular joint. This ligament divides the joint into two separate joint spaces. The upper attachment is on the superior and posterior aspects of the medial clavicle. DePalma6 has shown that the disk is perforated only rarely; the perforation allows a free communication between the two joint compartments (Fig. 13-2). Anteriorly and posteriorly, the disk blends into the fibers of the capsular ligament. The disk acts as a checkrein against medial displacement of the medial clavicle.
Costoclavicular Ligament
The costoclavicular ligament, also called therhomboid ligament, consists of an anterior and a posterior fasciculus. The costoclavicular ligament attaches inferiorly to the upper surface of the first rib and to the synchondral junction of the first rib and sternum; it attaches superiorly to the margins of the impression on the inferior surface of the medial end of the clavicle, sometimes known as the rhomboid fossa.7,8
The fibers of the anterior fasciculus arise from the anteromedial surface of the first rib and are directed upward and laterally. The fibers of the posterior fasciculus are shorter and arise lateral to the anterior fibers on the rib and are directed upward and medially. The fibers of the anterior and posterior components cross and allow stability of the joint during rotation and elevation of the clavicle. The anatomy of the costoclavicular ligament is in many ways similar to the structural configuration of the coracoclavicular ligament on the outer end of the clavicle (Fig. 13-3).
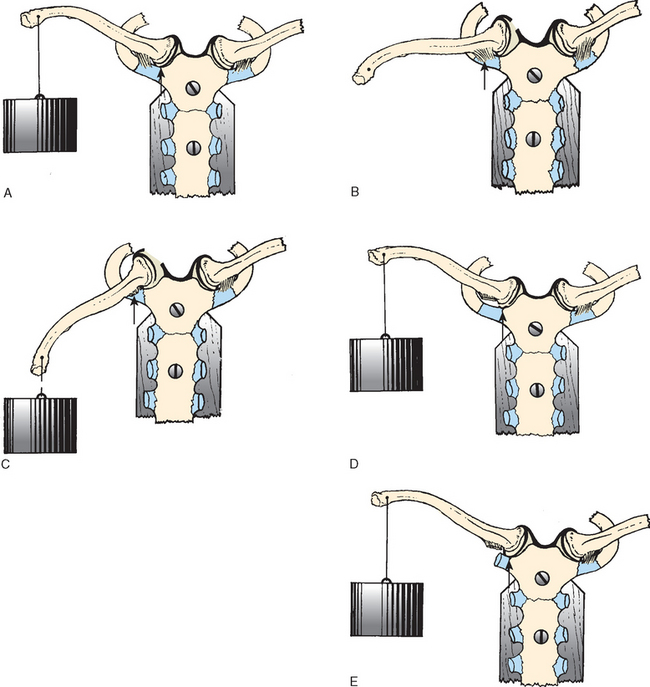
Bearn9 has shown experimentally that the anterior fibers resist excessive upward rotation of the clavicle and that the posterior fibers resist excessive downward rotation. Specifically, the anterior fibers also resist lateral displacement and the posterior fibers resist medial displacement (Fig. 13-4).
Capsular Ligament
The capsular ligament covers the anterosuperior and posterior aspects of the joint and represents thickenings of the joint capsule (Fig. 13-5). This structure is the strongest of all the sternoclavicular ligaments and is the first line of defense against the upward displacement of the medial clavicle caused by a downward force on the distal end of the shoulder. We have observed that the clavicular attachment of the ligament is primarily onto the epiphysis of the medial clavicle, with some secondary blending of the fibers into the metaphysis. Although some authors report that the intra-articular disk ligament greatly assists the costoclavicular ligament in preventing upward displacement of the medial clavicle, Bearn9 has shown that the capsular ligament is the most important structure in preventing upward displacement of the medial clavicle (see Fig. 13-4). In experimental postmortem studies, he determined, after cutting the costoclavicular, intra-articular disk, and interclavicular ligaments, that they had no effect on clavicle poise. However, the division of the capsular ligament alone resulted in a downward depression of the distal end of the clavicle. Bearn’s findings have many clinical implications for the mechanisms of injury of the sternoclavicular joint.
Through a cadaveric study Spencer and coworkers10 measured anterior and posterior translation of the sternoclavicular joint. Anterior and posterior translation was measured in intact specimens and following transection of randomly chosen ligaments about the sternoclavicular joint. Cutting the posterior capsule resulted in a significant increase in both anterior and posterior translation. Cutting the anterior capsule produced a significant increase in anterior translation. This study demonstrated that the posterior sternoclavicular joint capsule is the most important structure for preventing both anterior and posterior translation of the sternoclavicular joint, with the anterior capsule acting as an important secondary stabilizer.
Range of Motion of the Sternoclavicular Joint
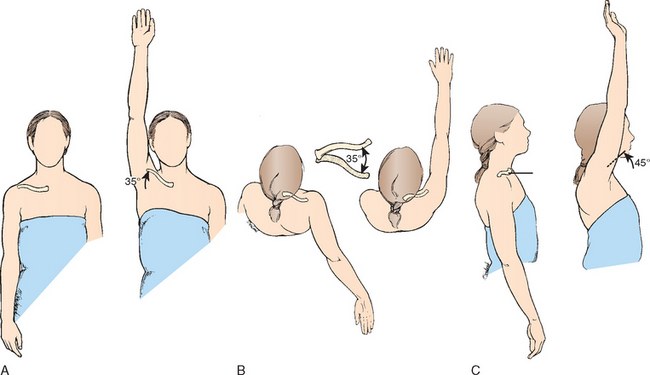
The sternoclavicular joint is freely movable and functions almost like a ball-and-socket joint in that the joint has motion in all planes, including rotation. The clavicle and therefore the sternoclavicular joint in normal shoulder motion is capable of 30 to 35 degreess of upward elevation, 35 degreess of combined forward and backward movement, and 45 to 50 degreess of rotation around its long axis (Fig. 13-6). It is most likely to be the most frequently moved joint of the long bones in the body because almost any motion of the upper extremity is transferred proximally to the sternoclavicular joint.
Epiphysis of the Medial Clavicle
Although the clavicle is the first long bone of the body to ossify (intrauterine week 5), the epiphysis at the medial end of the clavicle is the last of the long bones in the body to appear and the last epiphysis to close (Fig. 13-7). The medial clavicular epiphysis does not ossify until the 18th to 20th year, and it fuses with the shaft of the clavicle around the 23rd to 25th year. Webb and Suchey,11 in an extensive study of the medial clavicular physis in 605 male and 254 female cadavers at autopsy, reported that complete union might not be present until 31 years of age. This knowledge of the epiphysis is important because we believe that many of the so-called sternoclavicular dislocations are fractures through the physeal plate.
Applied Surgical Anatomy
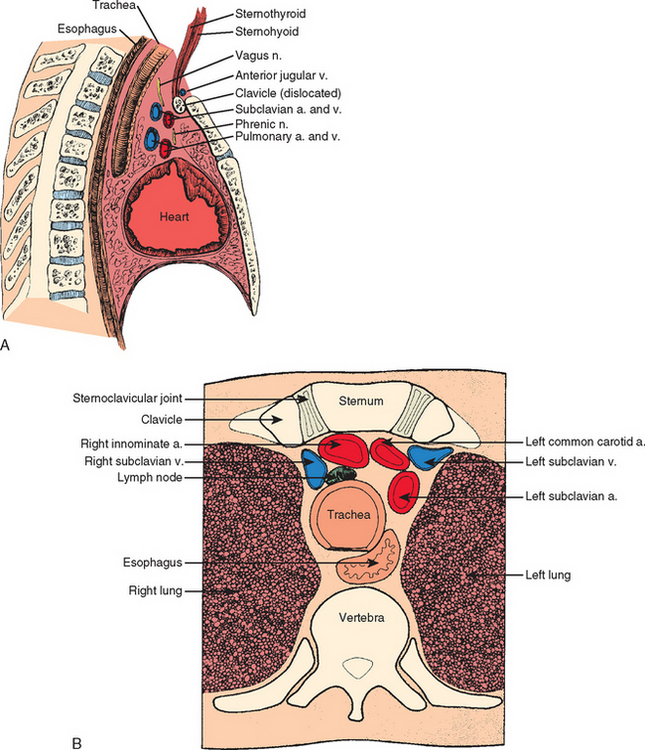
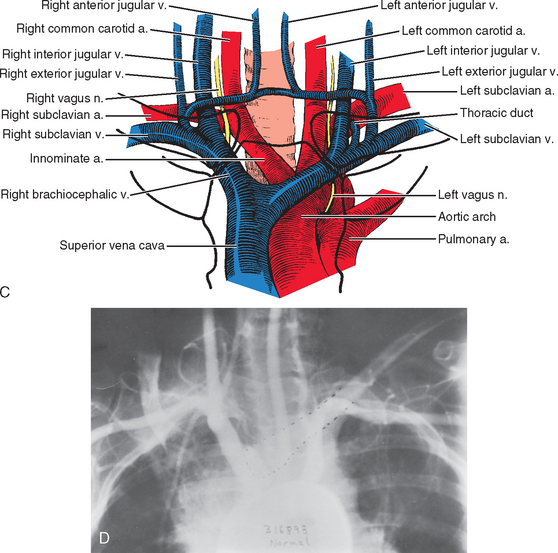
Surgeons planning an operative procedure on or near the sternoclavicular joint should be completely knowledgeable about the vast array of anatomic structures immediately posterior to the sternoclavicular joint. A curtain of muscles—the sternohyoid, sternothyroid, and scaleni— are located posterior to the sternoclavicular joint and the inner third of the clavicle and block the view of vital structures. Some of these vital structures include the innominate artery, innominate vein, vagus nerve, phrenic nerve, internal jugular vein, trachea, and esophagus. If one is considering the possibility of stabilizing the sternoclavicular joint by running a pin down from the clavicle into the sternum, it is important to remember that the arch of the aorta, the superior vena cava, and the right pulmonary artery are also very close at hand (Fig. 13-8).
Another structure to be aware of is the anterior jugular vein, which is between the clavicle and the curtain ofmuscles. Anatomy books state that this vein can be quite variable in size. We have seen it as large as 1.5 cm in diameter. This vein has no valves, and when it is nicked, it looks like someone has opened up the floodgates.
MECHANISM OF INJURY
Direct Force
Indirect Force
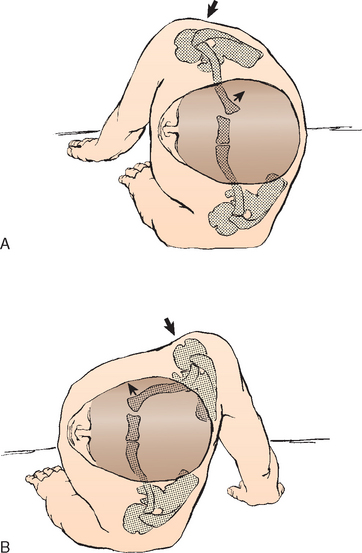
A force can be applied indirectly to the sternoclavicular joint from the anterolateral or posterolateral aspects of the shoulder (Fig. 13-9). This is the most common mechanism of injury to the sternoclavicular joint. Mehta and colleagues12 reported that three of four posterior sternoclavicular dislocations were produced by indirect force, and Heinig13 reported that indirect force was responsible for eight of nine cases of posterior sternoclavicular dislocations. Indirect force was the most common mechanism of injury in our 185 patients as well. If the shoulder is compressed and rolled forward, an ipsilateral posterior dislocation results; if the shoulder is compressed and rolled backward, an ipsilateral anterior dislocation results.
Most Common Cause of Injury to the Sternoclavicular Joint
The most common cause of dislocation of the sternoclavicular joint is vehicular accidents; the second is an injury sustained during participation in sports.14–16 Omer,16 in his review of patients from 14 military hospitals, found 82 cases of sternoclavicular joint dislocations. He reported that almost 80% of these occurred as the result of vehicular accidents (47%) and athletics (31%).
CLASSIFICATION OF PROBLEMS OF THE STERNOCLAVICULAR JOINT
Classification Based on Anatomy
Anterior Dislocation
An anterior dislocation is the most common type of sternoclavicular dislocation. The medial end of the clavicle is displaced anteriorly or anterosuperiorly to the anterior margin of the sternum (Fig. 13-10).
Classification Based on Etiology
Atraumatic Problems
For a variety of nontraumatic reasons, the sternoclavicular joint can sublux or enlarge.
Spontaneous Subluxation or Dislocation
Although both sternoclavicular joints can be affected, usually one joint is more symptomatic. It usually occurs in patients who have generalized ligament laxity of other joints (Fig. 13-11). In some patients, the anterior dislocation of the sternoclavicular joint is painful and is associated with a snap or pop as the arm is elevated overhead, and another snap occurs when the arm is returned to the patient’s side. The condition usually occurs in the late teens and young adulthood.
Arthritis
Arthritis involving the sternoclavicular joint can come in many forms:
Osteoarthritis.
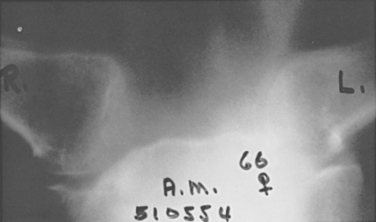
Osteoarthritis is characterized by narrowing of the joint space, osteophytes, subchondral sclerosis, and cysts on both sides of the joint (Fig. 13-12). Because most of the wear occurs in the inferior part of the head of themedial clavicle, most of the degenerative changes occur in that region. The sometimes discrete degenerative changes are best seen on tomograms and CT scans. Sternoclavicular joint arthritis and hypertrophy can develop after radical neck surgery, particularly when the spinal accessory nerve is sacrificed.17,18 The incidence is reported to be as high as 54%.17
Arthropathies.
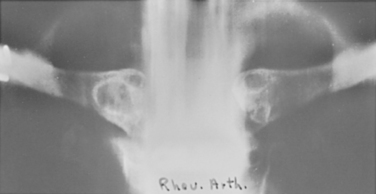
Some of the disease processes that produce degenerative changes in the sternoclavicular joint are rheumatoid arthritis, rheumatoid spondylitis, scleroderma, Reiter’s syndrome, psoriasis, polymyalgia rheumatica, secondary hyperparathyroidism, gout, pseudogout, leprosy, syringomyelia, metastatic carcinoma, condensing osteitis, Friedreich’s disease (aseptic necrosis of the medial end of the clavicle), and sternoclavicular hyperostosis (Fig. 13-13).
Condensing Osteitis of the Medial Clavicle.
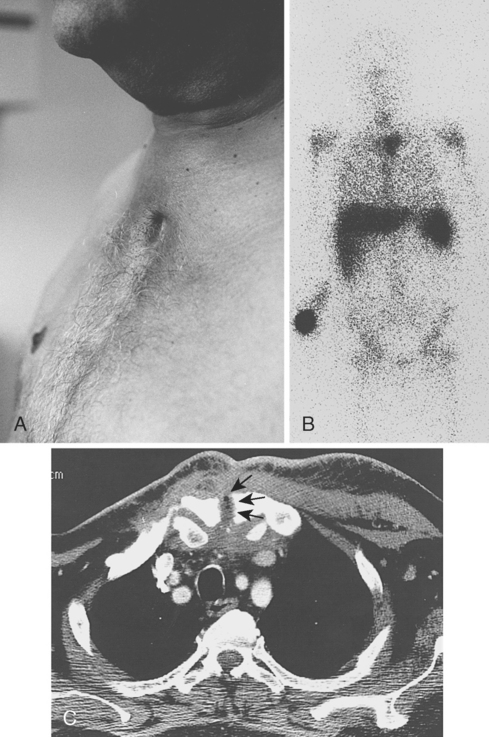
Condensing osteitis of the medial clavicle is an uncommon condition that usually develops in women older than 40 years and can occur secondary to chronic stress on the joint.59,60 The joint is swollen and tender, and radionuclide studies reveal increased uptake of the isotope.
Radiographs show sclerosis and slight expansion of the medial third of the clavicle. The inferior portion of the sternal end of the clavicle shows sclerotic changes. Some osteophytes may be present, but the joint space is preserved. The changes in the medial clavicle are best detected by CT. The differential diagnosis includes Paget’s disease, sternoclavicular hyperostosis, Friedreich’s avascular necrosis of the medial clavicular epiphysis, infection, Tietze’s syndrome, and osteoarthritis. More recently, Vierboom and coworkers19 described the use of magnetic resonance imaging (MRI) as an adjunctive method for diagnosing this entity. Most patients do well with conservative treatment, that is, with antiinflammatory medications. However, Kruger and associates20 recommend incisional or excisional biopsy in refractory cases.
Sternocostoclavicular Hyperostosis.
First described by Sonozaki,21,22 sternocostoclavicular hyperostosis involves adults of both genders between 30 and 50 years of age and is usually bilateral. The process begins at the junction of the medial clavicle, the first rib, and the sternum as an ossification in the ligaments and later involves the bones. In some cases, the hyperostosis is extensive and forms a solid block of bone consisting of the sternum, ribs, and clavicle. Patients may have peripheral arthritis. Subperiosteal bone changes have been noted on the radiographs of other bones of the skeleton, specifically, the humerus, pelvis, tibia, ribs, and vertebral bodies.
The condition has been graded into stages I, II, and III by Sonozaki and colleagues.21,22 Stage I consists of mild ossification in the costoclavicular ligaments. Stage II is characterized by an ossific mass between the clavicle and the first rib. In stage III, a bone mass exists between the clavicle, sternum, and first rib.
As might be expected with fusion of the sternoclavicular joint, shoulder motion is severely restricted. Sternoclavicular hyperostosis is a seronegative and HLA-B27–negative rheumatic disease. In this condition, hypostosis can appear in the spine, long bones, sacroiliac joints, and the sternoclavicular region. This entity is also associated with palmoplantar pustulosis. Tamai and Saotome have described a patient with palmar and plantar lesions associated with bilateral osseous fusion of both the acromioclavicular and sternoclavicular joints.23
Postmenopausal Arthritis.
Postmenopausal arthritis is seen primarily in postmenopausal women. Sadr and Swann24 reported on 22 patients with this problem who were seen in a 5-year study; 20 of the patients were women, and the majority of cases involved the sternoclavicular joint of the dominant arm. Nonoperative treatment was recommended.
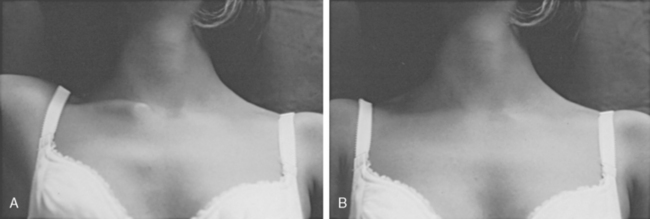
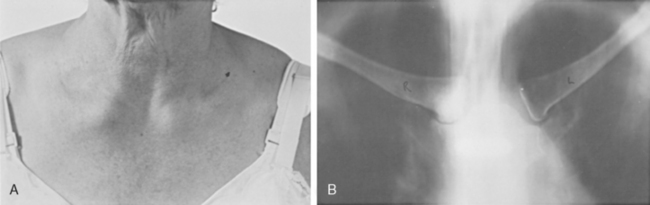
The condition is the result of normal degeneration of a frequently moved joint. It is almost without symptoms; a lump develops at the sternoclavicular joint and, occasionally, a vague ache (Fig. 13-14). Patients have no previous history of injury or disease. Radiographs reveal sclerosis and enlargement of the medial end of the clavicle, reactive sclerosis of the sternum, and subluxation of the joint. The pathologic changes are those of degenerative arthritis.
Infection
Spontaneous swelling with the appearance of joint subluxation may be associated with acute, subacute, or chronic bacterial arthritis. Predisposing conditions include intravenous (IV) drug addiction, bacteremia, rheumatoid arthritis, alcoholism, chronic debilitating diseases, and human immunodeficiency virus (HIV) infection.25,26 Sternoclavicular joint sepsis and osteomyelitis have also been reported in patients undergoing subclavian vein catheterization and in dialysis patients.27,28 CT is very helpful in making an early diagnosis of a septic sternoclavicular joint (Fig. 13-15).
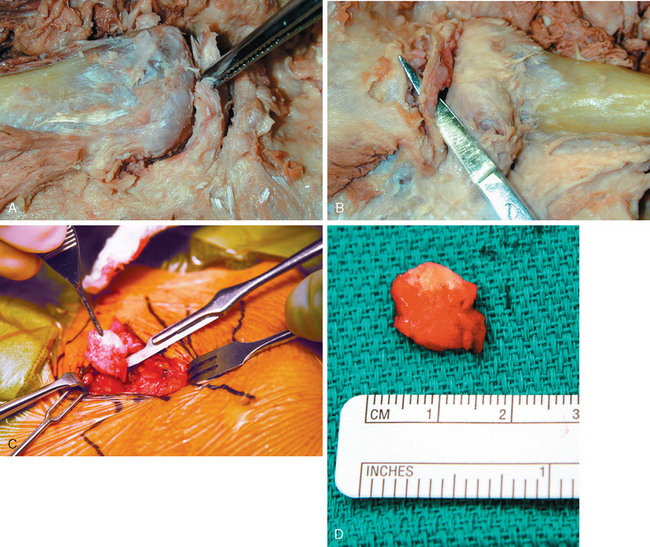
In 2002, Song and coworkers29 presented seven patients who had sternoclavicular joint infections. Predisposing factors included diabetes mellitus, HIV infection, immunosuppression, and pustular skin disease. All patients had local symptoms, including a medial clavicular mass and swelling. Antibiotic therapy and simple drainage and débridement were generally ineffective, with recurrence of infection in five of six patients. The patients were subsequently treated by resection of the sternoclavicular joint and the involved portions of adjacent ribs with an advancement flap from the pectoralis major muscle. The response to therapy was excellent in all patients and there were no wound complications.
Richter and coauthors30 reported on nine patients with infection of the sternoclavicular joint secondary to tuberculosis. The average time from onset of the disease to diagnosis was 1.4 years.
Higoumenakis31 has stated that unilateral enlargement of the sternoclavicular joint is a diagnostic sign of congenital syphilis. The enlargement of the sternoclavicular joint can be mistaken for an anterior dislocation. He reported the sign to be positive in 170 of 197 patients with congenital syphilis. The enlargement is attributed to hyperostosis of the medial aspect of the clavicle occurring in the sternoclavicular joint of the dominant extremity, which reaches its permanent stage and size at puberty.
INCIDENCE OF INJURY TO THE STERNOCLAVICULAR JOINT
The incidence of sternoclavicular dislocation, based on the series of 1603 injuries of the shoulder girdle reported by Cave and colleagues,5 is 3%. (Specific incidences of dislocation in the study were glenohumeral, 85%; acromioclavicular, 12%; and sternoclavicular, 3%.) In the series by Cave’s group, and in our experience, dislocation of the sternoclavicular joint is not as rare as posterior dislocation of the glenohumeral joint.
In a study of 3451 injuries during alpine skiing, Kocher and Feagin32 showed that injuries involving the shoulder complex accounted for 39% of upper extremity injuries and 11.4% of all alpine skiing injuries. Of the 393 injuries involving the shoulder complex, sternoclavicular separations accounted for 0.5%.
The largest series from a single institution is reported by Nettles and Linscheid,14 who studied 60 patients with sternoclavicular dislocations (57 anterior and 3 posterior). However, in our series of 185 traumatic sternoclavicular injuries, 135 patients had anterior dislocation and 50 patients had posterior dislocation.
Dislocations of Both Ends of the Clavicle
Dislocation of both ends of the clavicle is a rare, high-energy injury with fewer than 30 cases reported in the literature. In 1990, Sanders and associates33 reported six patients who sustained a dislocation of both ends of the clavicle (anterior dislocation of the sternoclavicular joint and posterior dislocation of the acromioclavicular joint). Two patients who had fewer demands on the shoulder did well with only minor symptoms after nonoperative management. The other four patients had persistent symptoms that were localized to the acromioclavicular joint. Each of these patients underwent reconstruction of the acromioclavicular joint that resulted in painless full range of motion and return to normal activity.
Combinations of Sternoclavicular Fractures and Dislocations of the Clavicle
Elliot34 reported on a tripartite injury about the clavicular region in which the patient sustained an anterior subluxation of the right sternoclavicular joint, a type II injury to the right acromioclavicular joint, and a fracture of the right midclavicle. Velutini and Tarazona35 reported a bizarre case of posterior dislocation of the left medial clavicle, the first rib, and a section of the manubrium. Others have reported fracture of the clavicle associated with posterior sternoclavicular dislocation, anterior subluxation, and injury to the long thoracic nerve.36 All of these injuries involving the sternoclavicular joint and the clavicle were associated with severe trauma to the shoulder region: The involved shoulder struck an immovable object or was severely compressed (Fig. 13-16).
Combination of Sternoclavicular Dislocation and Scapulothoracic Dissociation
Tsai and colleagues37 reported a patient with a sternoclavicular dislocation associated with a scapulothoracic dissociation. The patient had also sustained a transection of the axillary artery, an avulsion of the median nerve, and a complete brachial plexopathy. Surgical management included vascular repair and an above-elbow amputation.
SIGNS AND SYMPTOMS OF INJURIES TO THE STERNOCLAVICULAR JOINT
Atraumatic Subluxation and Dislocations
Atraumatic subluxation and dislocations are usually anterior and are usually not associated with a great deal of pain. As the patient raises the arm forward, the medial clavicle spontaneously displaces anteriorly and superiorly, and, when the arm is returned to the patient’s side, the medial clavicle is reduced. Occasionally, the displacement and reduction are associated with a sharp pain. Rockwood and Odor38 reported on this condition in 37 patients and urged nonoperative treatment.