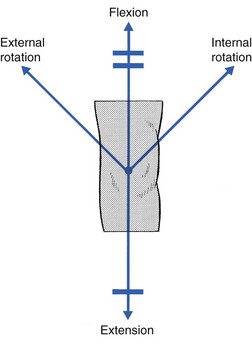
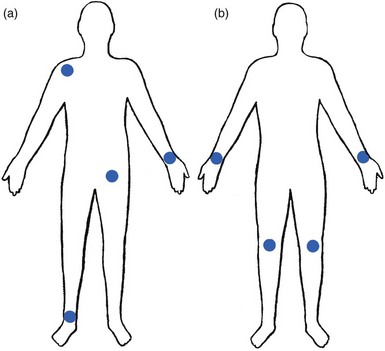
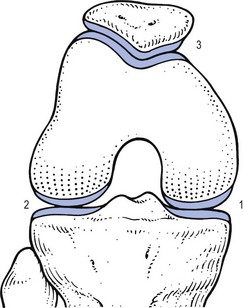
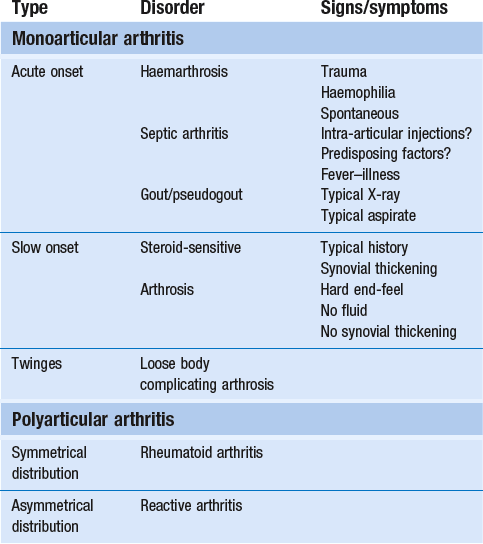
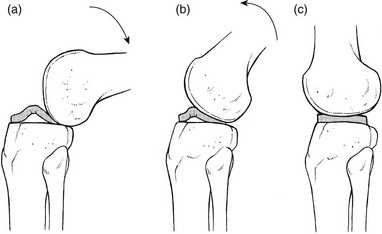
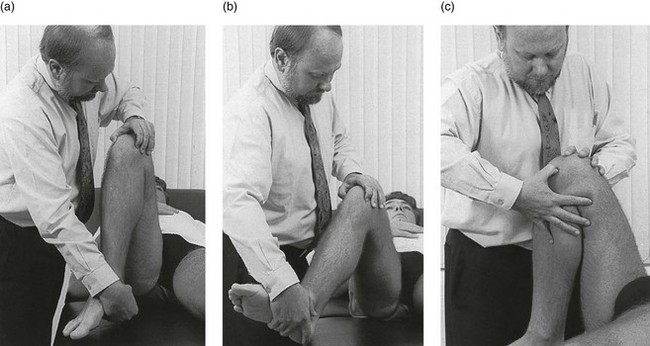
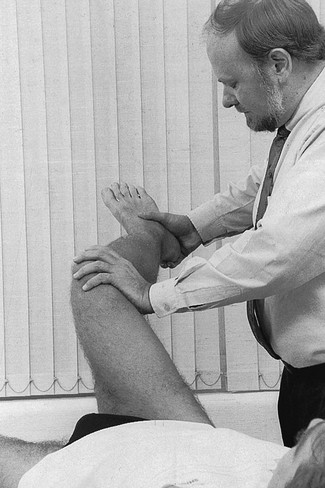
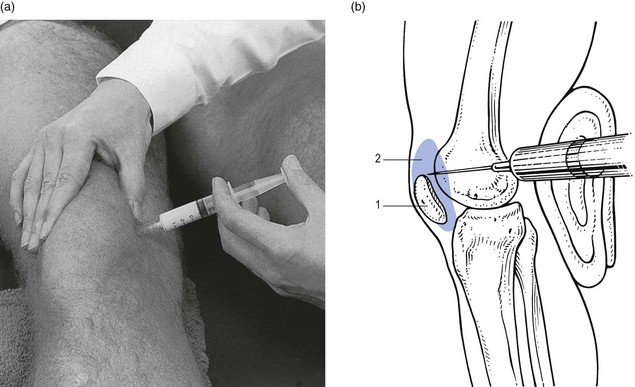
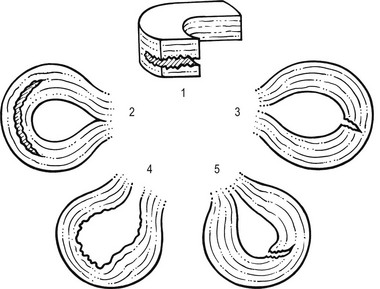
52 The normal capsular pattern at the knee joint is gross limitation of flexion and slight limitation of extension; the ratio of flexion : extension is roughly 1 : 10 (Fig. 52.1). Thus 5° of limited extension corresponds to 45–60° limitation of flexion and 10° to 90–100°. The range of rotation becomes restricted only in advanced arthritis. Recently, the concept of a capsular pattern of motion restriction at the knee was supported by a study of patients with inflamed knees.1 Rheumatoid arthritis is a common cause of knee inflammation. The symmetrical distribution of the affected joints is typical of this disease (Fig. 52.2). Reactive arthritis is an inflammation of the joint secondary to a generalized infection but in which the articular fluid remains aseptic (Crohn’s disease, Reiter’s syndrome, aseptic gonococcal arthritis).2,3 The arthritis can remain monoarticular but may involve other joints in an asymmetrical manner. In rheumatoid and reactive arthritis, intra-articular injections with triamcinolone give excellent but often only temporary results. Steroids injected into weight-bearing joints can cause arthropathy if injected too often.4,5 Therefore, injections must be restricted to two or three a year, which is enough to keep the patient comfortable. Nevertheless, considerable doubts about the dangers of repeated intra-articular steroid injections have arisen since a study report by Balch et al.6 They studied 65 patients with rheumatoid arthritis, who each received a minimum of 15 and a maximum of 167 injections at monthly intervals. Only two showed gross osteoarthrosis. These findings were confirmed later.7 The prime cause of gross degeneration in the knee joint is a disturbed distribution of load, which happens, for instance, when the patient suffers repeatedly from attacks of internal derangement because of a torn meniscus.8,9 Early osteoarthrosis will also occur if a valgus deformity is present from youth or there is an old malunited fracture that produces uneven load and repeated shearing strains. This also occurs if the meniscus is completely removed and its load-bearing function is therefore lost; the femoral condyles then exert pressure on the tibial platform over a much smaller area and the joint is apt to wear out rapidly.10,11 The knee is often affected in osteitis deformans and marked osteoarthrosis can then supervene. Aseptic necrosis of the medial condyle has been blamed as the cause of rapidly progressive, symptomatic osteoarthrosis in the elderly.12–14 The loss of articular cartilage, the structural changes of subchondral bone and the reactive osteophyte formation are the typical and well-known radiological appearances of progressive degenerative arthritis at the knee.15 It may be localized at the lateral, medial or patellofemoral compartment or may be generalized throughout the joint (Fig. 52.3). Although osteoarthrosis at the knee is considered very common, its prevalence is overestimated. The reason is quite simple: radiographs taken in a middle-aged or elderly patients complaining of knee pain will always show some evidence of cartilaginous degeneration. As age advances, some narrowing of the joint space and osteophyte formation always appear; they are normal and cause no harm.16 Therefore the diagnosis of symptomatic osteoarthrosis should be made not by radiography but on the typical findings on clinical examination. A minor degree of osteoarthrosis does not give rise to symptoms and it is only when gross osteoarthrosis with disintegration of the cartilage supervenes that the complaints can be attributed to it. What commonly, but incorrectly, is labelled ‘osteoarthrosis’ is a monoarticular steroid-sensitive arthritis or an impacted loose body. Both occur in middle-aged or elderly patients with osteophytes showing radiologically, and the diagnosis is missed if full clinical examination is not carried out properly. The treatment of osteoarthrosis is mainly with non-steroidal anti-inflammatory drugs (NSAIDs) and intra-articular injections with steroids. NSAIDs provide some relief of the symptoms but have clinically important side effects – they are estimated to cause 3300 deaths annually among the elderly in the US.17 Intra-articular injections with steroids also improve symptoms but the benefits are usually short-lived18,19 and there is always the potential for long-term joint deteriorations if injections are repeated too often. During the last decade, a number of promising reports on the effect of intra-articular injections with hyaluronic acid have been published. Hyaluronic acid is an important component of healthy synovial fluid and cartilage tissue; it is thought to protect the articular cartilage and soft tissue surfaces of the knee by acting as a lubricant and, because of its high viscosity, by imparting viscoelastic properties to the joint. Because intra-articular hyaluronic acid concentrations are lower in the synovial fluid of arthrotic knees,20 intra-articular injections with hyaluronic acid have been proposed as a means of restoring the viscoelastic properties of the knee joint, thereby providing symptom relief and improving joint function. Efficacy and safety of hyaluronic acid have been compared with that of saline,21–23 corticosteroids24 and NSAIDs. All the double-blind and randomized studies on the effect of hyaluronic acid on osteoarthrosis of the knee confirm that five intra-articular injections of sodium hyaluronate at weekly intervals are superior to placebo and are well tolerated in patients with osteoarthrosis of the knee, conferring a symptomatic benefit which persisted for 6 months.25–27 As hyaluronic acid seems to provide beneficial effects with minimal adverse reactions in a significant number of patients, it may be considered as a substantive addition to the therapeutic armamentarium in osteoarthrosis. When the condition is too advanced, joint replacement is the only solution. Cyriax described a monoarticular arthritis in the knee having some similarities with monoarticular arthritis in the shoulder and elbow. The cause and pathogenesis of this arthritis remain unclear but it heals immediately and lastingly after two injections of triamcinolone, thus earning it the title of ‘steroid-sensitive’ arthritis (Cyriax28: p. 404). The differential diagnosis of a monoarticular steroid-sensitive arthritis, summarized in Table 52.1, must be made from the following conditions29: • Polyarthritis: in monoarticular steroid-sensitive arthritis, disease does not spread to other joints and the laboratory findings remain normal, distinguishing it from rheumatoid and reactive arthritis.30,31 • Villonodular arthritis of Jaffé and Lichtenstein32 is an advanced arthritis, with marked synovial hyperplasia and thickening of the capsule.33 This type of arthritis is frequently complicated by spontaneous and recurrent haemarthrosis.34,35 In doubtful cases, arthroscopic biopsy is indicated.36 Treatment with steroid injections usually fails. Synovectomy is then advised.37 Good results have also been reported with intra-articular injections of thiotepa.38 • In middle age, a loose body complicating osteoarthrosis may be very difficult to distinguish. The distinct features of a loose body are sudden twinges, localized warmth and absence of synovial thickening. In long-standing arthritis, secondary wasting of the quadriceps muscle may make the knee feel weak and climbing stairs difficult; consequently, a complaint of twinges is not always a good sign. The only certain criterion may then be synovial thickening, which is not always ascertained easily, especially in middle-aged women, whose subcutaneous tissues are already somewhat thickened. In such circumstances, manipulation for a suspected loose body can be tried; if several attempts do not succeed, the joint should be injected. • Gout and pseudogout have an acute onset with an immediate and gross articular pattern. The treatment of monoarticular steroid-sensitive arthritis at the knee is two injections of 40 mg of triamcinolone at an interval of 2 weeks (Fig. 52.4). Fig 52.4 Intra-articular injection of the knee. Structures in (b): 1, patella; 2, suprapatellar pouch. Technique: injection for monoarticular steroid-sensitive arthritis The patient lies on the couch and relaxes the quadriceps muscle (Fig. 52.4a). If gross arthritis is present, it may be necessary to place a small cushion under the knee in order to keep it in slight flexion. The operator stands level with the other knee. With one hand the patella is pushed up and towards the operator, which makes the medial edge more prominent. A 5 mL syringe is filled with steroid suspension and fitted with a thin needle, 4 cm long, which is placed near the upper border of the patella and thrust in horizontally just between the patellar edge and the medial femoral condyle (Fig. 52.4b). It lies intra-articularly at about 2 cm depth.39 An acute arthritis at the knee occurs in 25% of all attacks of gout.40 There is considerable pain, swelling and redness, which makes the condition difficult to differentiate from septic arthritis, haemarthrosis or pseudogout. Sometimes analysis of the joint fluid is necessary to distinguish these conditions. Calcium pyrophosphate crystals are believed to induce the synovitis of pseudogout. The term chondrocalcinosis refers to the presence of these calcium-containing salts in the articular cartilage,41 which are seen on radiographs. The disease may be familial and is also commonly associated with a wide variety of metabolic disorders – for example, haemochromatosis, hyperparathyroidism, ochronosis and diabetes mellitus – and is also found in patients undergoing dialysis.42,43 This usually indicates a serious lesion, most commonly rupture of a cruciate ligament or an intra-articular fracture (see p. 599).44,45 Sometimes it is the result of a direct capsular contusion.46 The patient states that, after the injury, the knee became painfully swollen within 2–3 minutes. The speed of swelling, together with the severe pain, indicates an intra-articular haemorrhage; blood fills the joint at once and is a strong irritant. Blood left within the joint for weeks can cause severe arthritis and serious erosion of the articular cartilage. It should be removed at once.47–49 After a few days, it may be necessary to aspirate the remaining blood-tinged synovial effusion. Sudden pain and swelling without previous injury in an elderly patient will often be caused by an intra-articular haemorrhage, presumably as the result of the rupture of an intra-articular vein. Haemarthrosis should be suspected particularly when the patient is on anticoagulant therapy.50,51 Septic arthritis can follow haematogenous dissemination from focal infections, such as urethritis, cystitis, skin infections55 or dental abscesses. This is particularly so when resistance is decreased: diabetes, rheumatoid arthritis, renal failure or a deficient immune system are all possible causes of decreased resistance.56 Intravenous drugs and gonococcal infections, particularly with antibiotic-resistant gonococci,57 have also been blamed for the increased incidence of septic arthritis of the knee. Another cause of septic arthritis is direct inoculation of organisms during intra-articular injection. Treatment is with high doses of antibiotics intravenously and daily aspiration of the knee.58 A thorough clinical assessment can usually provide sufficient information to make a definitive diagnosis of internal derangement.59 Plain radiographs are of no use in the diagnosis of internal derangement. Arthroscopy may be useful but should never be performed without first completing a full preoperative examination. These can be grouped into congenital anomalies, traumatic conditions, cysts and metabolic disorders. The most common congenital anomaly with pathological sequelae is a discoid lateral meniscus. The incidence in autopsy specimens is between 0% and 7%,60 but most do not cause problems.61 Symptomatic disorder seems to occur only in the Wrisberg ligament type of discoid meniscus. This type is classically described as lacking a posterior capsular attachment and presents in childhood with a ‘snapping’ knee: the meniscus rolls up in front of the lateral compartment during flexion, as a consequence of increased friction and greater mobility; during extension, the rolled meniscus becomes trapped anteriorly, until it reduces suddenly with a dramatic audible snap (Fig. 52.5).62 The disorder affects children and adolescents. The presenting symptom is internal derangement at the lateral side of the knee. Clinical examination reveals an audible click and visible alteration of the knee at approximately 10–20° of extension.63 Diagnosis is confirmed with sonography or magnetic resonance imaging (MRI).64 Treatment of a congenital discoid meniscus is complete or partial meniscectomy.65 Disruption of collagen fibres within the meniscus occurs as the result of either an acute injury or gradual age-dependent degeneration (Fig. 52.6). The split may be either horizontal or vertical. Fig 52.6 Main types of meniscal tear: 1, horizontal; 2, longitudinal; 3, radial; 4, degenerative; 5, flap. Vertical tears are the most important clinicopathological condition of the meniscus and usually result from excessive force applied to a normal meniscus. Transverse tears are less common than longitudinal ones. The latter frequently involve the thin inner edge of the meniscus, which, when it separates, creates the bucket-handle tear, so characteristic of the locking knee.66 Peripheral longitudinal tears are defined as those occurring within 3 mm of the meniscosynovial junction and comprise about 30% of all vertical tears.67 Left untreated, most of these peripheral lesions heal spontaneously.68 The less mobile medial meniscus is much more commonly involved than the lateral meniscus. The medial meniscus is closely bound to the medial collateral ligament and the medial coronary ligament, which attaches the meniscus to the tibia, is only 4–5 mm long. The lateral meniscus, however, is separated from the lateral collateral ligament by the popliteus tendon, and its coronary ligament is much longer (13–20 mm).8 This difference in mobility is the reason for the higher proportion of torn medial menisci. The typical vertically torn meniscus, which results in a bucket-handle lesion, occurs between the ages of 15 and 30 years. The mechanism of injury is as follows: during flexion–extension, the menisci move with the tibia, to which they are attached (see online chapter Applied anatomy of the knee), but during rotational movements they follow the femoral condyles. During combined movements, the normal displacement of both menisci may be prevented and the menisci become trapped between tibia and femur. This typically happens in a football player who, in an attempt to kick the ball sideways, severely twists on the slightly flexed and weight-bearing knee: the rotation force of the femur on the immobilized tibia then ruptures the cartilage. It has also been suggested that meniscal lesions may appear as the result of knee instability, in particular after anterior cruciate lesions.69,70 It is generally accepted that these lesions result from normal forces acting on a degenerating meniscus.71 Degenerative horizontal cleavage lesions are therefore more common in individuals of more than 40 years of age and usually occupy the posterior half of the menisci.72,73 They are so common that most authors regard them as part of the usual degenerative processes in the knee (Noble and Turner,74 Fahmy et al,75 Smillie9: pp. 79, 97, 108, 145, 153). In a posterior crack, the history is less dramatic than in that of a vertical tear.72 For instance, the patient finds that, if there is a twist on the knee, something is occasionally felt to ‘give way’, usually at the back of the joint. It is immediately difficult to straighten the leg, but when it is shaken or kicked out, a click is heard and the limb returns to normal function. Sometimes the patient gives a different history: slight rotation and flexion during weight bearing – for example, on getting out of a car – produce an uncomfortable click which is relieved immediately on straightening the leg. If the patient is seen some time after reduction of the meniscus, the knee may appear normal or merely shows a sprained coronary ligament. Alternatively, the patient presents with a history of a minor posterior crack but the routine functional examination is normal. In these cases, the following tests can be used to elicit signs of a ruptured meniscus (Fig. 52.7). During recent decades, arthroscopy has made the diagnosis and treatment of a torn meniscus much easier.76,77 Nevertheless, arthroscopy does not make a clinical diagnosis redundant and routine arthroscopy without a previous thorough functional examination can lead to wrong conclusions and treatment. Because meniscal lesions are so common that they are a frequent finding in middle-aged people, it is very possible that a meniscal tear, found incidentally during ‘routine’ arthroscopy, is not the cause of the patient’s complaints. For instance, if a patient with a chronic ligamentous lesion of the medial collateral band or the coronary ligaments is subjected to arthroscopy before a clinical diagnosis has been made, the damaged meniscus will be blamed and thus unnecessarily removed. The use of the arthroscope has encouraged the widespread assumption that the source of chronic pain in the area of the knee is to be found in the interior of the joint itself. The more likely cause of pain, however, is in the surrounding ligaments, but this can only be demonstrated by a thorough clinical assessment.78 We, like Goodfellow (‘He who hesitates is saved’),79 believe that, although meniscal tears can be detected by arthroscopy with almost 100% accuracy, caution is needed in ascribing symptoms at the knee to meniscal lesions. Diagnosis of meniscal lesions should be made clinically and arthroscopy should be reserved for confirmation of clinical findings as an aid in therapeutic decision making. The hip is slightly rotated medially and strong valgus pressure is exerted at the knee (Fig. 52.8). In this position, repeated extensions are performed but not beyond the end of range – i.e. if the extension range is limited by 10°, the movement should stop at about 15°. In order to ensure this, the thumb placed in the popliteal fossa is used as a brake during the procedure. Once flexion and extension movements have been performed several times in this way, rapid to-and-fro rotations of the knee are added. The meniscal lesion itself causes no pain because the body of the meniscus is almost completely insensitive. Pain is the result of ligamentous strain caused by the repeated luxations and subluxations. However, damaged menisci frequently do not provoke any symptoms. In a postmortem study in patients above and below the age of 50, Noble and Hambden found that up to 60% of the former and 19% of the latter had meniscal tears.80,81 It is important to realize that most complaints following subluxation of a meniscus stem from a sprained coronary ligament. If a patient with a history of a former locked meniscus complains of persistent and localized pain but proves to have a full range of movement with a normal end-feel, a sprained coronary ligament should be suspected and appropriate treatment given. After successful manipulation, the reduced piece of cartilage may never subluxate again and the patient is cured for good. This was emphasized by Casscells,82 who stated that not all meniscal tears need surgical treatment. Asymptomatic meniscal tears identified at the time of arthroscopic examination for ligamentous lesions are best left in place or unrepaired, as they will remain asymptomatic.83 Furthermore, laboratory studies have demonstrated that torn menisci may have normal biomechanical function if the peripheral circumferential fibres remain intact.84,85 Although surgery of the meniscus should not be undertaken lightly, it is unwise to permit repeated attacks of internal derangement because they initiate a premature, troublesome and intractable osteoarthrosis.75,86 The choice lies, then, between total or partial meniscectomy or repair. Total meniscectomy leads to loss of integrity of the articular cartilage and impairment of joint stability.87–91 It is no longer considered the treatment of choice because of increasing dissatisfaction with the long-term results.10,92 Instead, and if this is technically possible, only the loose fragment is removed and the outer part of the meniscus, together with the coronary ligament, is left alone.93 The result is no increase in weight-bearing stress on the tibia.94 The outer rim of the meniscus can still bear weight and thus preserve the articular cartilage, as well as play a useful role in stabilizing the joint. In experienced hands, this partial removal of the meniscus using arthroscopy is much less damaging to the joint and requires only 2 days’ bed rest. Subsequent return to work and sport is also quicker.95 Several long-term studies have demonstrated the technique’s superiority over total meniscectomy.96–100 In recent years, suturing of the relatively vascular outer edge of the meniscus has been shown to result in healing by fibrous tissue.101–107 Meniscal repair is nowadays considered as the treatment of choice in single, vertical, longitudinal tears in the outer third of the meniscal substance.108 Good to very good long-term results may be expected if the longitudinal tear is less than 3 cm long and within 3 mm of the periphery, and the meniscal tissue is not degenerating.109,110
Disorders of the inert structures
Capsular and non-capsular patterns
Capsular pattern
Rheumatoid and reactive arthritis
Osteoarthrosis
Monoarticular steroid-sensitive arthritis
Differential diagnosis
Treatment
![]()
Crystal synovitis
Gout
Pseudogout
Haemarthrosis
Post-traumatic haemarthrosis
Spontaneous haemarthrosis in the elderly
Septic arthritis
Non-capsular pattern
Internal derangement
Introduction
Lesions of the meniscus
Congenital anomalies
Traumatic meniscal lesions
Vertical tears
Horizontal and posterior cracks
Diagnosis
Treatment
Natural history
Surgery
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree