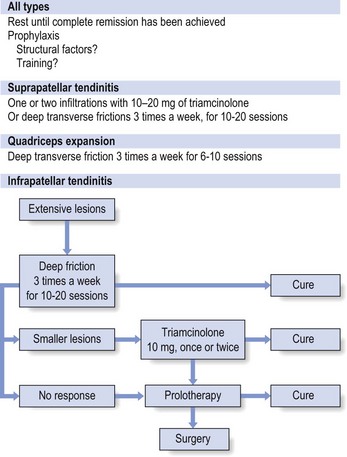
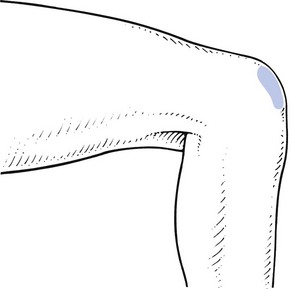
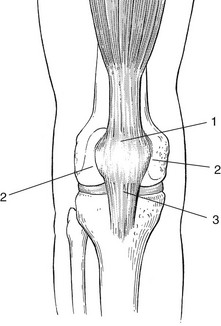
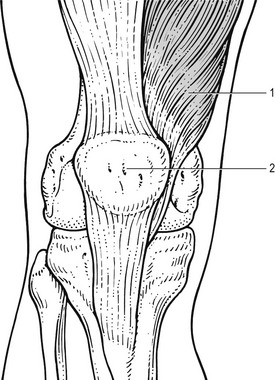
54 Patients who suffer an acute quadriceps strain will usually know right away. They are typically involved in sports requiring kicking, jumping, or initiating a sudden change in direction while running. Frequently, a sharp pain is felt, associated with a loss in function of the quadriceps. Sometimes pain will not fully develop during the athlete’s activity while the thigh is warm; consequently, the extent of the injury is underestimated. Stiffness, disability and pain then set in some time afterwards, e.g. late at night, and the following morning the patient can walk only with a limp.1 Clinical examination shows a normal hip and knee, although passive knee flexion is painful or both painful and limited, depending on the size of the rupture. Resisted extension of the knee is painful and slightly weak. As a rule, the lesion is in the rectus femoris, usually at mid-thigh level.2 The affected muscle belly is hard and tender over a large area. Sometimes a haematoma can be palpated. In serious lesions, a space can be detected by palpation. This is particularly the case in major ruptures just above the suprapatellar tendon, which occur mainly in patients over 40 years of age.3 In such cases, there is not only pain but also weakness during resisted extension, and the patient is unable to straighten the knee actively over the last 30°. Ultrasonography is an excellent imaging modality for visualizing the quadriceps muscles; it has the ability to image the muscles dynamically and assess for bleeding and haematoma.4 Development of myositis ossificans as a complication of a thigh contusion is not uncommon in adolescents and young adults.5 It occurs in 9% of quadriceps contusions and seems to be associated with five risk factors (knee motion less than 120°, injury occurring during American football, previous quadriceps injury, delay in treatment of more than 3 days and ipsilateral knee effusion).6 Early diagnosis is important and is usually made with the help of sonography.7,8 There is no proper treatment but the lesion undergoes spontaneous cure within 2 years.9 Therapy with deep transverse massage is contraindicated. Initial haemorrhage may be reduced by elastic strapping and an ice bag over the lesion. In the case of a contusion, holding the knee in 120° of flexion for 24 hours following a quadriceps contusion also appears to shorten the time needed for the patient to return to unrestricted full athletic activities.10 The patient sits with the knees outstretched. Flexion at the hips, together with maximal extension of the knees, induces complete relaxation of the quadriceps. The physiotherapist stands at the patient’s side. The correct level is sought. The fingers of one hand are placed deep to the affected fibres. The other hand can reinforce the palpating one. The thumbs are placed laterally to be used as a fulcrum. By flexion of the fingers, during an upward-drawing movement, the physiotherapist drives all the fibres between fingers and femur (Fig. 54.1). After the friction, active isometric contractions are done over 5–10 minutes. Again, this is carried out in a fully relaxed position, so that the contraction cannot exert tension on the healing tissue (see Ch. 5). The quadriceps tendon has a superficial and a deep layer. The superficial layer runs without interruption from the quadriceps muscle, over the patella to the tibial tuberosity. The deep layer inserts all around the patellar border, effectively making the patella a sesamoid bone in the tendon. Tendinous lesions therefore occur not only at the inferior aspect of the bone but also at the superior, medial and lateral borders. Tendinosis about the patella is a typical overuse phenomenon in sports characterized by high demands on leg extensor speed and power, such as volleyball, basketball, soccer and athletics. It was first described by Sinding-Larsen in 192111 and Johansson in 1924.12 Kulund13 and Ferretti14 also reported cases of tendinosis at the upper border of the patella. Cyriax15 describes three possible sites: the upper border (suprapatellar tendinosis), the apex – the classic ‘jumper’s knee’ (infrapatellar tendinosis) and at either side of the patella (tendinosis of the quadriceps expansion) (Fig. 54.2). The lesion was uncommon until the mid-1960s, when the syndrome of jumper’s knee became more and more frequent because of increased training and higher performance goals for athletes.16,17 During the last few decades, these lesions have reached epidemic proportions18; in sports medicine centres, patellar tendinopathy is one of the leading reasons for consultation and often contributes to the decision to give up an athletic career.19 Fig 54.2 Localizations of quadriceps tendinitis (with permission from Cyriax15: p. 408): 1, suprapatellar; 2, expansion; 3, infrapatellar. The history is obvious: during or after exertion, there is localized pain at the front of the knee. In mild examples, there is probably only a little pain after activity, whereas in a severe case pain forces the athlete to stop, and pain at rest can also supervene. The patient also states that walking upstairs or standing up from sitting is painful. The lesion can be classified by its symptoms into four stages (Table 54.1).13,20,21 Table 54.1 Staging of quadriceps tendinitis21 Palpation identifies the site. To make the deeper layers of the tendon accessible for the palpating finger, the patella must be tilted as much as possible (see pp. 716 and 717). Conventional radiographic techniques are of no use in the diagnosis of quadriceps tendinitis. Ultrasonography, however, seems to have some value in staging the disorder.22–24 On magnetic resonance imaging (MRI), swelling of the tendon and changes in the intrasubstance signal may be present.25 However, the sensitivity and specificity of MRI is 75% and 29%, respectively. In younger patients with relatively mild symptoms, MRI does not show significant changes and in older, active patients changes may be present in asymptomatic knees.26,27 Classically, conservative treatment for patellar tendinopathy consists of rest, ice, taping and anti-inflammatory drugs. Other modalities, such as electrotherapy, ultrasound, laser therapy and extracorporeal shock wave therapy, have also been used.28 If these measures are insufficient or fail to relieve the symptoms, surgery is usually advised.29 The patellar tendon is incised and the hyaline inflammatory tissue (usually the middle portion of the patellar ligament) is removed.30,31 However, the benefits of open tenotomy can be questioned on the basis of the results, which show a success rate that varies between 58%14 and 78%.32 Sporting success is seen in about 50% of tenotomy patients, with a median time to return to pre-injury level of activity of 10 months.33 Eccentric training as a treatment option for tendinopathy has gained credit in recent decades. The technique was first presented by Curwin and Stanish in 1984, with encouraging results.34 The programme is based on eccentric drop squats, which are performed with some level of discomfort. During the programme, the athlete should be removed from sports activity. When training becomes pain-free, load is increased by first increasing the speed of the eccentric phase and then adding weight.35,36 Our advice is to treat all peripatellar lesions with either a local infiltration of triamcinolone or a series of deep transverse friction.37 At the upper border and the apex, infiltration with triamcinolone can be used safely and with very good results, providing the injection is done exactly at the right spot, using a weak solution (10 mg/mL) and according to the general principles of infiltration. Deep transverse friction is preferred if the lesion is too extended for infiltration. If a small spot remains resistant to treatment, it can subsequently be infiltrated. Because relative rest is always the first measure in tendinous lesions, the patient should not return to athletics until complete remission of the lesion has been achieved. After successful treatment, and in order to prevent recurrence, it is important to detect the possible causes of the tendinitis (inappropriate or faulty training programme or structural factors) and to correct these.38 In recalcitrant cases, one or two infiltrations with sclerosing solution to the tenoperiosteal border can be tried.39 The patella must be tilted in such a way that the affected spot can be reached. This can be achieved by pressing the lower pole of the patella posteriorly with the web of the thumb or with thumb and index finger, which steadies the bone and forces the upper border upwards and forwards. With the middle finger of the other hand, the tender area can now be sought more easily. It is important to move the finger as far as possible under the inclined patella in order to catch the tendinous fibres of insertion deep under the bone. Deep friction is performed by pressing the tendon between the middle finger and the superior aspect of the patella (Fig. 54.3). The index finger is used to reinforce the middle finger. The thumb is placed as far distally as possible on the leg and used as a fulcrum. The friction consists of a to-and-fro movement of the whole forearm and hand, in a transverse direction over the tendinous fibres. The patient sits with the knee outstretched and the hip flexed, so that the quadriceps is fully relaxed. The patella is fixed as described earlier. The upper edge of the patella is marked and the tender area identified. Usually it lies at the medial edge of the upper border, less frequently at the lateral edge of the upper border, and as a rule it is no larger than 1 or 2 cm. A spot is chosen about 1.5–2.0 cm above the centre of the affected area. A 3 cm needle fitted to a 2 mL syringe is introduced at this spot and moved in the direction of the patella (Fig. 54.4). The more the patella is tilted, the better the needle can reach the affected area. Small injections are given only when the tip of the needle is felt to pierce tendinous structure and touch bone. Considerable resistance is felt during the injection. Caution is taken to infiltrate the whole tender area by the usual technique of fanwise insertions and withdrawals. Once again, the patient sits with the knees outstretched and the quadriceps muscle fully relaxed. The therapist sits level with the patient’s knees. With the thumb of one hand, the patella is pushed distally and over towards the affected side. This allows the edge of the patella to project outwards. The little finger of the other hand is extended as far as possible. The ring finger, reinforced by the middle finger, is placed under the patellar edge in such a way that it presses upwards, squeezing the tendinous fibres against the posterior aspect of the patella. Caution is observed so as to bring the hand into full supination, which means that the operating finger is horizontal, with pressure being applied against the back of the projecting edge of the patella. A vertical finger just presses against the femur and no friction on the tenoperiosteal junction results. Hand and forearm are held in line with the tibia, and friction is produced by a horizontal movement along the patellar edge (Fig. 54.5). Twenty minutes’ friction, three times a week for 2–3 weeks, nearly always results in cure. Infrapatellar tendinitis is by far the most common tendinitis at the patella. The lesion lies over an area of 1–2 cm at the inferior pole of the patella. In order to make this area more accessible, pressure is exerted at the upper part of the patella, in the following manner. The physiotherapist stands level with the extended knee. One hand is placed just above the patella, so that the web of the thumb can exert downward pressure. This stabilizes the patella and tilts the apex upwards, so that the tender area can be sought with great accuracy. Friction is given with the middle finger of the other hand, reinforced by the index finger. The thumb is placed as far proximally as possible on the thigh. Pressure is exerted upwards, so that the lesion becomes squeezed between finger and bone (Fig. 54.6). Sometimes a large osteophyte can be palpated at the apex; if so, it is important to investigate to establish which side of the osteophyte the tenderness is located. Friction is given by alternate adduction and abduction movements at the shoulder, which draw the finger strongly along the inferior border of the patella. Once the exact location is identified and the borders marked on the skin, a point is chosen 1.5–2 cm inferior to the midpoint of the affected area. A thin 3 cm needle is fitted with a syringe, containing 2 mL of triamcinolone. With the patella remaining tilted, the needle is inserted at the identified point and moved upwards, through the infrapatellar tendon, until it hits bone (Fig. 54.7). It is important to reach the posterior aspect of the patellar apex because most lesions lie deeply at the tenoperiosteal junction. The infiltration is now given using a series of small droplets along the inferior border. Considerable pressure has to be exerted on the syringe to push the drug in. Care is taken to inject only when the tip of the needle is felt to hit bone. Return to sport must be gradual, and a training programme that does not impose too much strain on the quadriceps during the first few weeks is advised. An underlying biomechanical factor as the basis for a possible recurrence should be sought.40,41,38 Treatment of quadriceps tendinitis is summarized in Figure 54.8. Rupture of the suprapatellar quadriceps tendon is an uncommon injury. Most of the patients are elderly, and sometimes there is diagnostic confusion with other causes of inability to use the legs, such as a mild stroke.41 The mechanism of injury usually involves forced hyperflexion or rapid extension from a weight-bearing position.42 Pain, swelling, a palpable gap and inability to straighten the leg against resistance are the cardinal features. Treatment is operative repair. A patellar tendon rupture may be caused by acute or chronic excessive traction force.43 The tendon is then pulled from the lower pole of the patella.44 Degenerative rheumatic disease may also give rise to rupture of the infrapatellar tendon.45,46 Osteochondrosis of the tibial tuberosity, or Osgood–Schlatter disease, occurs in boys between 10 and 15 years of age.48 The typical symptoms are local pain during sports or when walking upstairs. Local tenderness makes kneeling impossible.49 Clinical examination reveals local ache during resisted extension of the knee. Palpation shows an enlarged, tender and warm tuberosity. Radiography confirms the diagnosis and is important in differentiating the condition from more serious disorders such as osteomyelitis, arteriovenous malformations and osteosarcoma.50 Most patellar fractures are stellate fractures, occurring after a fall or a direct blow (dashboard injuries). In the last decade, an increasing number of patellar fractures in association with total knee replacement have been described.51,52 In young patients, an uncomplicated fracture heals quickly but early osteoarthrosis has to be expected.53 When accurate reduction and stable fixation cannot be achieved, partial or total patellectomy must be considered and seems to produce satisfactory results.54,55 Transverse fractures are uncommon, except in an elderly person with an osteoporotic patella. After the trauma, the patient can walk with pain; because the capsule enclosing the patella is not ruptured, displacement is avoided and therefore the disability is minor.56 Patellofemoral pain is a common condition. About 25% of the population will, at some stage in their lives, suffer from patellofemoral symptoms.57 There is no clear consensus in the literature concerning the terminology, aetiology and treatment for pain in the anterior part of the knee. The term ‘anterior knee pain’ is suggested to encompass all pain-related problems. By excluding anterior knee pain caused by intra-articular disorders, peripatellar tendinitis or bursitis, plica syndromes, Osgood–Schlatter disease and other rarely occurring conditions, it is suggested that those remaining patients with a clinical presentation of anterior knee pain could be diagnosed as having patellofemoral pain syndrome (PFPS).58 The term chondromalacia patellae, although once used as an all-inclusive term for anterior knee pain, is now only accepted to describe pathological lesions of the patellar articular cartilage found at arthroscopy or arthrotomy. A diagnosis of ‘chondromalacia patellae’ for anterior knee pain is made far too often.59,60 Stougard detected cartilaginous lesions at the posterior aspect of the patella in almost every knee joint at autopsy61 and Paar and Riehl observed damage to the patellar cartilage in almost every operated knee.62 The cause of patellofemoral pain is unknown.63 Currently, there are two theories to explain its origin: the mechanical and the neural theory.64 Most authors stress the importance of the congruency between the articular surfaces of the femur and the patella.65–67 During the last decade, a great deal of emphasis was given to the idea of imbalance of the soft tissues surrounding the patella as the prime cause of patellar ‘maltracking’. The soft tissue balance is particularly critical in the first 20° of knee flexion, where the position of the patella in relation to the femur is determined by the interaction of the medial and the lateral soft tissue structures; after this 20° of motion, the patella engages the femur and the bony architecture becomes more important for the position of the patella relative to the femur.68 Any imbalance in the soft tissue structures in the first 20° of flexion will mean that the patella does not encounter the trochlea optimally, which may lead to undue stress on various tissues around the joint and thus to pain. The imbalance may be the consequence of multiple biomechanical defaults. Weakness of the vastus medialis obliquus is thought to be the single most important factor causing momentary patellar subluxation.69 Also, the passive stabilizing structures are usually more extensive and stronger on the lateral than on the medial side. Active stabilization is provided by the quadriceps muscle – on the lateral side the vastus lateralis and on the medial side the vastus medialis. The fibres of the vastus medialis are divided functionally into two compartments: the vastus medialis longus and the vastus medialis obliquus (VMO). The latter does not play a role in active extension of the knee but keeps the patella centred in the trochlea of the femur throughout knee extension.70 The VMO is the only active stabilizer of the patella (Fig. 54.9); therefore the timing and the amount of activity in the VMO is critical to patellofemoral function and it is hypothesized that small changes in its activity may have considerable effects on the patellar position.71 Electromyography (EMG) studies have revealed that, in patients with patellofemoral pain, the VMO contracts at a significantly slower rate than the vastus lateralis, whereas in normal subjects the reflex response time of both muscles is equal.72–74 A recent MRI study examined VMO size in patients with patellofemoral problems and found atrophy in all of them. Although it is not clear whether this atrophy is a result or a cause of PFPS, there is obviously a strong relationship between the two.75 Fig 54.9 Active medial stabilization is provided by the vastus medialis obliquus (VMO): 1, VMO; 2, patella. Other biomechanical factors that may contribute to the development of patellofemoral pain are tightness in the lateral structures, increased Q angle (see p. 722) and faulty foot mechanisms.76–78 In a retrospective study on 282 male and female students enrolled in physical education classes, Witvrouw et al found a significant correlation between four parameters and the development of patellofemoral pain: a shortened quadriceps muscle, an altered VMO muscle reflex response time, a decreased explosive strength and a hypermobile patella.79 The normal articular cartilage is aneural, so defects in the surface are not thought to produce pain. It has therefore been suggested that irritation of the subchondral bone produces the pain.80 Schneider et al could reproduce the typical pain sensation by raising intrapatellar pressure in about 40% of patients suffering from persistent patellofemoral pain. This subgroup was treated with a new method of intraosseous drilling and decompression. Of the patients so treated, 90% experienced pain relief more than 3 years postoperatively, which may indicate osseous hypertension as a cause of the pain.81 Some authors have sought the origin of the pain in soft tissue structures around the knee. Nociceptive nerve fibres and neural markers (S-100 protein, neurofilament protein, substance P and neural growth factor) have been demonstrated in the medial and lateral retinacula and in the infrapatellar fat pad.82,83 It is important to stress the fact that most anterior knee pain is not caused by patellofemoral disorders but stems from infra-, supra- or peripatellar tendinitis, or a coronary ligament lesion. A basic functional examination should therefore always be performed first (see Box 54.1). However, if specific symptoms warrant, and the basic functional examination is totally negative, attention must be directed towards any peculiarities found during inspection of the patella and surrounding tissues. Alignment of the lower extremity is evaluated first by observing the patient standing. Excessive varus or valgus of the extremities and internal femoral rotation are often associated with an extensor mechanism malalignment. Hyperextendable knees may also contribute to the development of anterior knee pain. McConnell points out that shock absorption throughout the lower leg then comes from internal rotation of the femur, rather than from knee flexion.84 Some of the most important observations are made with the patient in the sitting position, with the legs bent to 90°. The position of the patella is assessed by viewing the knee from the lateral and the frontal aspects. In a lateral view (Fig. 54.10), the patella should be situated on the distal end of the femur, with the proximal patellar pole level with the anterior femur and the anterior surface of the patella in line with the tibial shaft. In ‘patella alta’, the upper border of the patella sits more on the anterior surface of the femur and ‘faces towards the ceiling’. Viewed from anterior, a normally positioned patella faces straight ahead (Fig. 54.11); ‘outfacing’ and ‘infacing’ patellae are easily recognized in this position.
Disorders of the contractile structures
Extensor mechanism
Quadriceps strains and contusions
Treatment
Technique: deep friction to the quadriceps muscle
![]()
Tendinous lesions about the patella
Stage
Symptoms
I
Pain after activity
II
Pain at onset, disappearing during activity and reappearing after it
III
Continuous pain, inability to perform
IV
Weakness due to rupture
Treatment
Technique: deep friction to the suprapatellar tendon
![]()
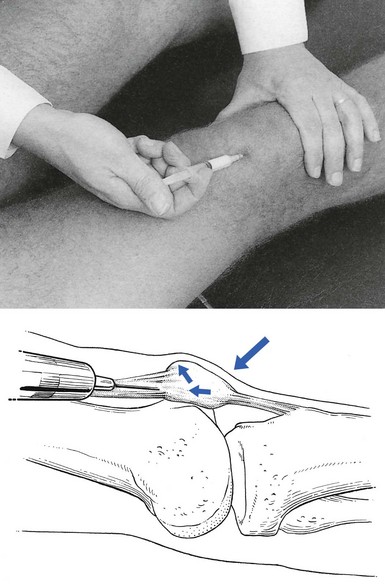
Technique: infiltration to the suprapatellar tendon
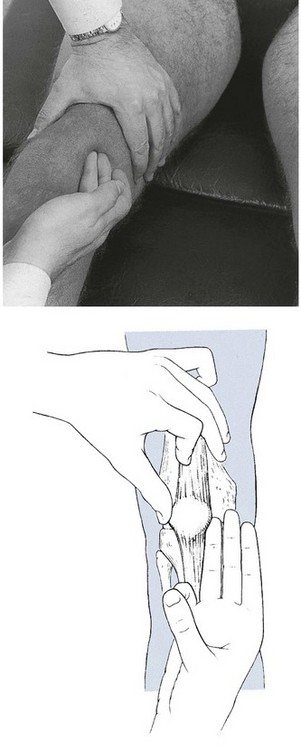
Technique: deep friction to the quadriceps expansion
![]()
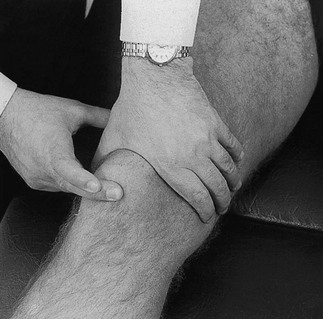
Technique: deep friction to the infrapatellar tendon
![]()
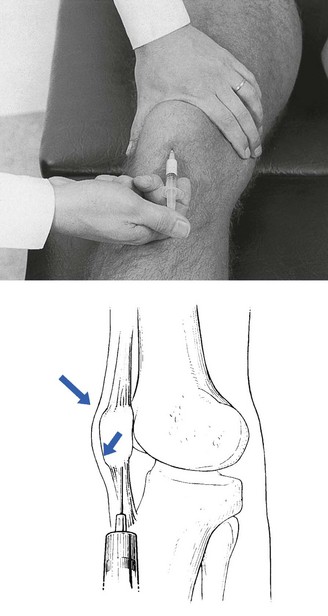
Technique: infiltration of the infrapatellar tendon
![]()
Rupture of the quadriceps tendon
Lesions of the infrapatellar tendon
Lesions of the insertion at the tibial tuberosity
Apophysitis
Patellar fracture
Patellofemoral disorders
Introduction
Mechanical theory
Neural theory
Clinical examination
Inspection on standing
Inspection on sitting
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Disorders of the contractile structures