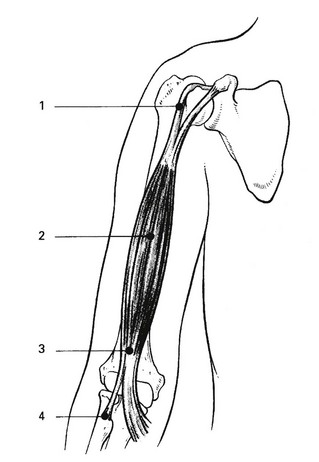
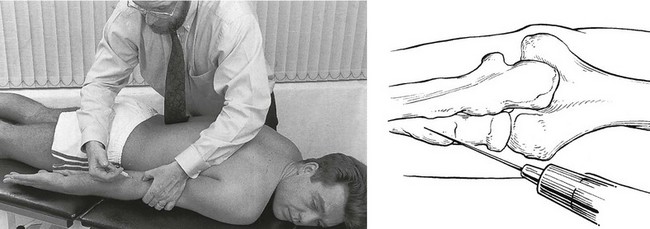
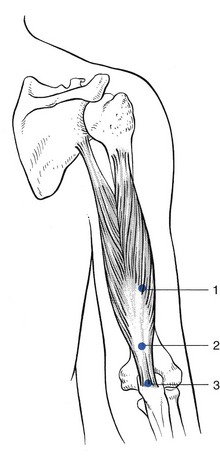
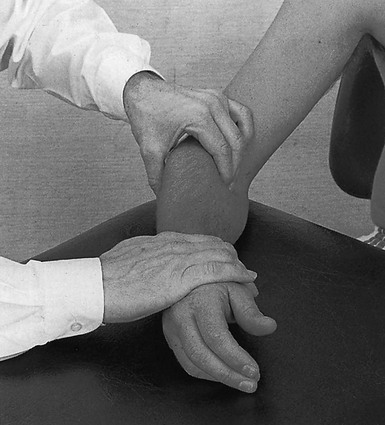
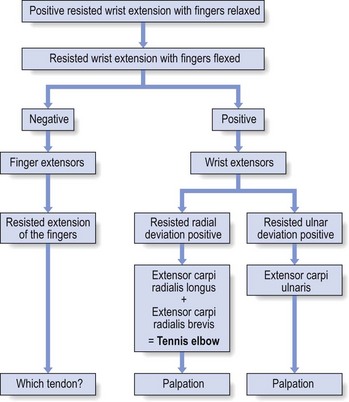
19 The biceps and brachialis muscles are tested during resisted flexion, which should be performed with the elbow bent at a right angle – the neutral position between flexion and extension and also the one in which elbow flexion strength is maximal1,2 – and the forearm held in active supination. This is the best position to test the biceps muscle,3 which is more often strained than the brachialis. Electromyographic studies confirm decreased activity of the biceps when flexion is performed in pronation.4–6 If the biceps muscle is at fault, resisted supination will also be painful. There are four possible localizations, indicated by the site of the pain (Fig. 19.1). Rupture of the long head of biceps is one of the commonest tendinous ruptures. It causes scarcely any symptoms, except the appearance of a round ball of muscle at the lower part of the arm when the patient flexes the elbow. Resisted flexion remains painless and strong, the brachialis muscle still functioning as the strongest flexor of the elbow – only 8% of elbow flexion strength and approximately 21% of forearm supination strength is lost.7 Treatment is not required. The therapist grasps the muscle belly at the point of the lesion with the ipsilateral hand in a pinching grip, holding the fingers well flexed, which enables the posterior aspect of the muscle to be reached (Fig. 19.2). The hand is then pulled anteriorly. This results in a transverse friction to the muscular fibres, which can be felt to pass under the fingers. The hand is then brought back to the starting position without losing contact with the patient’s skin. The manœuvre thus has two phases: an active phase, when the hand is pulled anteriorly, and a passive phase, when the hand is brought backwards again. Apart from the usual signs on examination, a localizing sign is present – pain at full passive pronation. This is the result of the bicipital insertion being pinched between the radial tuberosity and the shaft of the ulna as the radius turns over the ulna during pronation.8 Palpation is not necessary and would even be negative, as tenderness cannot be elicited by probing with a finger. The joint line between humerus and radius is palpated. The posterior edge of the ulna is easily felt. A point is chosen 2–3 cm further distally from the joint line and just laterally to the ulna. A 2 mL syringe is filled with triamcinolone and a thin needle, 2 cm long, is fitted. The needle is inserted at the chosen point and pushed vertically downwards until it hits the shaft of the radius, either directly or through a tendinous structure (Fig. 19.3). In the former case, the needle has to be partly withdrawn and reinserted in a slightly different direction in order to feel the tendinous resistance. Then a series of droplets is infiltrated at the tendinous insertion according to the usual infiltration technique. The ipsilateral hand, which grasps the patient’s forearm about the wrist, is used to perform a pronation movement. The forearm is pronated until the biceps tendon passes under the therapist’s thumb. The tendon now lies medial to it. Friction is thus performed by this indirect movement. During this part of the movement, the pressure on the tendon is augmented (active phase). The forearm is then brought back to the supinated position, while the pressure is released (passive phase). These repeated movements result in a transverse friction (Fig. 19.4), which is continued for 15 minutes. Treatment consists of 2 or 3 weeks’ deep transverse friction. Myositis ossificans is a benign condition, characterized by heterotopic bone formation, which occurs after injury to muscle fibres, connective tissue, blood vessels and underlying periosteum.9 It occurs most often in males aged between 15 and 30 years and presents with the following triad of symptoms: pain in the affected muscle, a palpable mass and a flexion contracture.10 The history of severe contusion is helpful in the early evaluation of these patients, before radiographic changes are evident.11 When, after an injury, usually fracture,12 pain in the elbow region increases and the range of movement gradually decreases,13 this may indicate the development of myositis ossificans. An increasing firm mass in the brachialis muscle is mostly palpable in the middle or distal segment of the arm and becomes visible on the radiograph in the course of a few weeks.14 A technetium bone scan is clearly positive.15 When myositis ossificans has fully developed, only a little movement to either side of the right angle is possible and even rotations are markedly limited. Myositis ossificans does not respond to conservative treatment and may disappear spontaneously over the course of 2 years. Lipscomb et al17 have stated that myositis ossificans in the upper extremity is very likely to resorb completely. If not, surgical excision may be performed, but only when the lesion is completely ossified, because removal of immature bone may cause extensive local recurrence.18 We have never encountered a lesion of the brachioradialis muscle but a case has been described by Barbaix.19 The patient, following exertion, experienced supracondylar pain at the radial aspect of the elbow occurring during activities which included elbow flexion and simultaneous rotations. The pain could be elicited on passive extension, which was slightly limited, and on resisted flexion of the elbow. Accessory examination showed resisted supination with the forearm in full pronation more painful with a flexed elbow than with an extended one. Diagnosis was confirmed with echography and the patient responded well to infiltration with triamcinolone acetonide. These clinical findings are compatible with an earlier electromyographic study showing electrical activity with flexion, especially with the forearm rotated in pronation.20 A distal biceps tendon rupture is usually at the tendinous insertion and sometimes accompanies an avulsion of the radial tuberosity.21 The lesion is reported increasingly in the current literature.22–26 The mechanism of injury is most commonly an eccentric load applied to a flexed elbow. On physical examination there may be swelling, haematoma and a ‘Popeye’ deformity of the upper arm. However, the normal contour of the distal biceps may still appear to be intact if the lacertus fibrosus is not torn.27 Range of motion is usually full unless there is severe swelling. Strength testing reveals weakness in forearm supination and, to a lesser extent, elbow flexion. The biceps squeeze test and the hook test are two physical examination manœuvres that have been shown to be sensitive and specific in diagnosing distal biceps tendon ruptures. The biceps squeeze test involves compression of the biceps muscle belly, which results in forearm supination if the tendon is intact.28 In the hook test, with the elbow actively flexed and supinated, an index finger should be able to ‘hook’ under a cord like structure in the antecubital fossa if the tendon is intact.29 The treatment of choice is surgery: anatomic repair of distal biceps tendon rupture provides consistently good results and early anatomic reconstruction can restore strength and endurance to the elbow.30–32 Lesions of the triceps muscle are rare. Three possible localizations can be differentiated by palpation (Fig. 19.5): the musculotendinous junction, which is the most common site; the body of the tendon; and the tenoperiosteal junction at the olecranon. A 1 mL syringe is filled with triamcinolone acetonide and a 2 cm needle is fitted. The tip of the olecranon is palpated and the tender point located. The needle is inserted 1 cm proximal to it and directed towards the olecranon (Fig. 19.6). Tendinous resistance should be felt before hitting bone. Infiltration is then carefully performed by several withdrawals and reinsertions of the needle and maintaining bony contact. The patient sits next to the couch with the arm rested, the elbow held in 90° flexion. The therapist sits at a right angle to the patient’s arm. With the contralateral hand the patient’s elbow is grasped, while the other hand stabilizes the patient’s forearm. The tender spot in the triceps tendon is palpated and then the index finger, reinforced by the middle finger, is placed at the medial side of the tendon. Counterpressure with the thumb is then applied at the lateral aspect of the proximal part of the forearm (Fig. 19.7). The therapist abducts the arm and then brings it back into the side. This is the active phase and is followed by relaxation while bringing the arm back into abduction. Such repeated movement results in a transverse friction to and fro over the lesion. Abrahamsson et al33 reported a case of lateral elbow pain caused by a chronic compartment syndrome of the anconeus muscle. The symptoms were lateral elbow pain and muscular dysfunction during heavy work. The pain was reproduced by repeated extension of the elbow and pronation of the forearm. There was a slightly bulging mass and pronounced tenderness of the anconeus muscle, which were successfully treated by fasciotomy. This has been reported as a rare injury.34,35 The most common form is an avulsion from the osseous tendon insertion.36 Injury at the musculotendinous junction occurs less often.37 The most common mechanism of injury is a deceleration stress superimposed on a contracted triceps muscle.38 A palpable gap, with complete weakness of arm extension, is pathognomonic of triceps rupture. In many cases, however, the palpable defect is not noted initially because of swelling and ecchymosis.39 Early surgical repair of the injury is the treatment of choice and gives predictably good results.40,41 Sometimes the same mechanism of injury causes a triceps avulsion fracture. Apart from the same symptoms and signs, the lateral radiograph will show the presence of flecks of avulsed osseous material from the olecranon (‘flake sign’), which is almost pathognomonic of this lesion.42 If the pain is the result of an injury and resisted extension of the elbow is painful and weak, the possibility of a fracture of the olecranon must be considered. Local tenderness and marked articular signs at the elbow joint will also be present: warmth, swelling and limitation of passive movements in the capsular pattern. In most cases, conservative treatment is sufficient.43 A radial palsy and a C7 root palsy are the most common of the other neurological disorders. Apart from known traumatic causes, a radial palsy is quite often the result of pressure from a crutch or sleeping with the inner side of the arm pressed against a hard edge (‘Saturday-night paralysis’). In this case, resisted extension of the wrist is also very weak and may even result in wrist-drop. The condition is painless and recovers spontaneously over the course of 3–6 months. Some severe cases require neurosurgical repair (see online chapter Nerve lesions and entrapment neuropathies of the upper limb). To confirm the diagnosis, the test is repeated with the elbow held actively in full extension – a position which inhibits the function of the biceps. The muscle is not found to be particularly tender and therefore an infiltration with a local anaesthetic should be given (Fig. 19.8). This may effect a cure, but treatment with deep transverse friction (Fig. 19.9) is usually necessary. It is successful in 1 or 2 weeks. The patient sits with the arm rested on the couch. The therapist sits at a right angle to the patient’s arm. The elbow is held in 90° flexion and the forearm in neutral position between pronation and supination. The therapist palpates at the anterior aspect of the forearm for the muscle belly, which may be facilitated by an active contraction by the patient. The fingertips of two or three fingers of the contralateral hand are then placed on the tender area and counterpressure is applied with the thumb at the lateral aspect of the forearm. The forearm is stabilized with the other hand (Fig. 19.10). The friction movement is begun underneath the muscle and the fingers are pulled over the muscle towards the therapist. This is the active phase. The fingers are then brought back to the previous position (passive phase). The sequence is repeated. The term ‘tennis elbow’ has been used to describe a multiplicity of conditions of the elbow. Renton,44 in 1830, was the first to describe a patient with pain along the outer forearm which increased on using the hand. In 1873, Runge, a German physician, wrote an article on ‘writer’s cramp’. He distinguished the condition from a case of 2 years’ inability to write, associated with tenderness on the lateral condyle of the humerus. Rest and electrotherapy had no effect and he then cauterized the skin over the tender area, after which the patient became well. He thought the cramp was the result of traumatic inflammation of the periosteum in this location, originally caused by a forcible supination effort and made chronic by the continual pull of the extensor muscles attached to the lateral condyle.45 Morris (1882)46 compared a condition named ‘lawn-tennis arm’ to rider’s sprain – a lesion of the adductor longus muscle at the hip – and Major also called the condition ‘lawn-tennis elbow’.47 An annotation in The Lancet (1885) drew attention to the number of people suffering from ‘tennis elbow’, whose plaintive letters had recently appeared in the lay press. From then on, the term ‘tennis elbow’ has been used to describe symptoms at the outer aspect of the elbow. Remak (1894)48 and Bernhardt (1896)49 agreed that it was a periosteal tear from occupational overuse of the extensor muscles that arise from the lateral condyle. Couderé (1896)50 called it a ‘ruptured epicondylar tendon’, Féré (1897)51 ‘épicondylalgie’, Franke (1910)52 ‘epicondylitis’. In 1921, Schmidt53 suggested superficial epicondylar bursitis, thereby incriminating the bursa described by Schreger in 1825.54 In 1922, Osgood55 and, in 1932, Carp56 believed the lesion to lie in the radiohumeral bursa, and extra-articular bursa under the extensor tendons, which was first described by Monro in 1788.57 In 1936, Cyriax58 compiled a list of no fewer than 26 different types of lesion to which the name tennis elbow had been given by 91 authors during the previous 63 years. He presented a synopsis of opinion as to the cause of tennis elbow and stated that a condition, the symptoms and signs of which are as constant as those of tennis elbow, may well be supposed to have but one background and, as a corollary, but one type of treatment. An enormous number of articles on tennis elbow have been published in the ensuing years, describing different pathological entities such as radiohumeral bursitis, radiohumeral synovitis, irritation of the synovial fringe, degeneration of the annular and collateral ligaments, fibrillation of the articular cartilage, osteoarthrosis of the radiohumeral joint, osteochondritis dissecans, aseptic necrosis of the radial head, stenosis of the orbicular ligament, chondromalacia of the radial head and capitellum, calcific tendinitis of the extensor muscles, myofasciitis, traumatic periostitis of the lateral epicondyle, and enthesopathy of the lateral epicondyle of the humerus, among others.59–68 A new concept was introduced in 1972 when Roles and Maudsley described the ‘radial tunnel syndrome’69 (see online chapter Nerve lesions and entrapment neuropathies of the upper limb). The most encompassing classification is perhaps that of O’Neill et al,70 who state that ‘tennis elbow or lateral epicondylitis consists clinically of pain localized in the region of the lateral aspect of the elbow with tenderness in the vicinity of the lateral epicondyle’. This vague description illustrates how unsure most authors are about the pathogenesis of tennis elbow. Most authors consider tennis elbow as a local condition in relation to the lateral epicondyle of the humerus. However, some authors have described this condition as resulting from a cervical problem and they claim curative results with treatment to the neck. Gunn et al71 considered a tennis elbow to be caused by a reflex localization of pain from radiculopathy at the cervical spine. Several authors agreed with this point of view.72–74 Weh75 believes that the idea of a local clinical assessment of tennis elbow should be broadened to an overall vision of a functional chain consisting of cervical spine, shoulder and elbow, in which local reflex inhibition of muscles innervated by the seventh nerve root and a limitation of movement of the cervical spine are causative elements. It is quite certain that elbow pain may have a cervical origin. This should not be designated ‘tennis elbow’ but instead ‘referred elbow pain’ from the cervical spine. If clinical examination shows the elbow pain to be evoked by movements at the elbow, then the lesion must be sought there. In contrast, if cervical examination is positive, this means that cervical movements must be the cause of pain in the elbow region. ‘Tennis elbow’ is technically a misnomer, since it most often occurs in non-tennis players: less than 5% of the patients play tennis.76–78 Even in a population of 500 tennis players complaining of lateral elbow pain, Grachaw and Pelletier found tennis elbow present in only 39.7%.79 This accords with Krämer’s findings.80 Neither is the term ‘epicondylitis’ right: at least 10% of the lesions do not lie at the epicondyle itself. Furthermore, the suffix ‘-itis’ indicates an inflammatory process, but histological analysis shows only disruption of the collagen bundles with vascular and fibroblast proliferation and without inflammation. Therefore the term ‘tendinosis’ should be preferred over ‘tendinitis’.81 Of all the patients seen in a general medical practice, 0.5% suffer from ‘tennis elbow’.82 The condition is therefore important enough to try to define it properly. The lesion lies at the elbow, in the structures controlling wrist extension and radial deviation (extensores carpi radiales). Theoretically, the lesion could also lie in the ulnar deviators or in the extensors of the fingers but this is much less common and should be separately named: for example, lesion of the extensor carpi ulnaris muscle, lesions of the extensor digitorum muscle. It is generally believed that tennis elbow is an overuse phenomenon caused by repeated contractions of the radial extensors of the wrist,61,83 and especially of the extensor carpi radialis brevis.84 Post-traumatic causes have also been described.85 In the early stages, when the tissue attempts repair, and often just as the tear begins to unite, continued muscular contraction pulls the healing surfaces apart once more. This results in the formation of a painful scar with self-perpetuating inflammation (Cyriax86: p. 178). Cyriax’s view was confirmed by Coonrad and Hooper in 1973.76 More recent observations during surgery have led Nirschl to classify this condition mostly under the heading ‘tendinosis’ rather than tendinitis: surgical inspection shows a typically ‘grayish color and homogenous and generally edematous and friable tissue’ indicating angiofibroblastic invasion – fibroblasts and vascular granulation-like tissue.87–89 Inflammatory cells are not usually found.90 The patient is usually between 30 and 60 years,91,92 and seldom under 20 or over 70. As the lesion is the result of overuse, the patient does not notice the pain the moment a tennis elbow develops but rather a few days later. A pain is described starting at the outer aspect of the elbow and radiating down the posterior aspect of the forearm, very often as far as the dorsum of the hand. Pain may be felt in the long and ring fingers. It is evoked by grasping, pinching and lifting – the movements that involve extension of the wrist and in which the wrist extensors merely act as stabilizers of the joint. The next approach is to differentiate the radial extensors from the ulnar extensor using two accessory tests. Resisted radial deviation is compared with resisted ulnar deviation, the wrist being held in the neutral position between flexion and extension. In the rare circumstance that resisted ulnar deviation is painful, the lesion lies in the extensor carpi ulnaris muscle. Much more frequently, resisted radial deviation is painful, which indicates a lesion in either the extensor carpi radialis longus or the extensor carpi radialis brevis – the structures involved in tennis elbow (Fig. 19.11).
Disorders of the contractile structures
Resisted flexion of the elbow
Pain
Biceps muscle
Pain at the shoulder
Pain at the mid-arm
Technique: deep friction to the biceps belly
Pain at the elbow
Technique: infiltration of the distal insertion of the biceps
![]()
Technique: friction to the distal insertion of the biceps
Brachialis muscle
The brachialis muscle and heterotopic ossification
Brachioradialis muscle
Weakness
Rupture
Resisted extension of the elbow
Pain
Triceps muscle
Technique: infiltration at the tenoperiosteal junction
Technique: friction to the musculotendinous junction, body of tendon and tenoperiosteal junction
Anconeus compartment syndrome
Weakness
Painful weakness
Total or partial rupture of the triceps tendon
Fracture of the olecranon
Painless weakness
Radial palsy
Resisted supination
Resisted pronation
Technique: friction to the pronator teres muscle
Pain on resisted extension of the wrist
Tennis elbow
Terminology
Pathological features
History
Functional examination
Disorders of the contractile structures